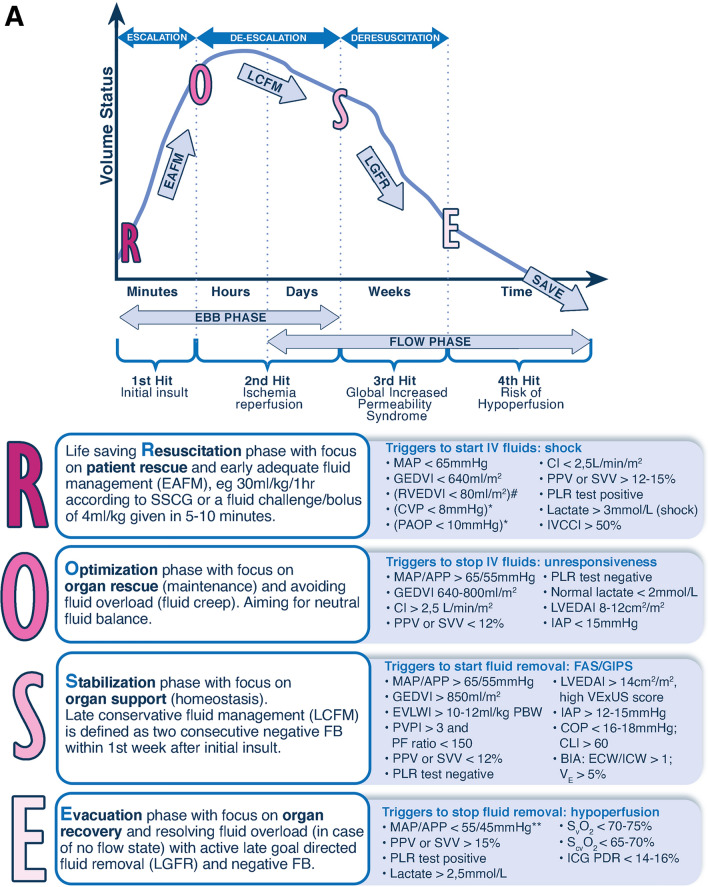
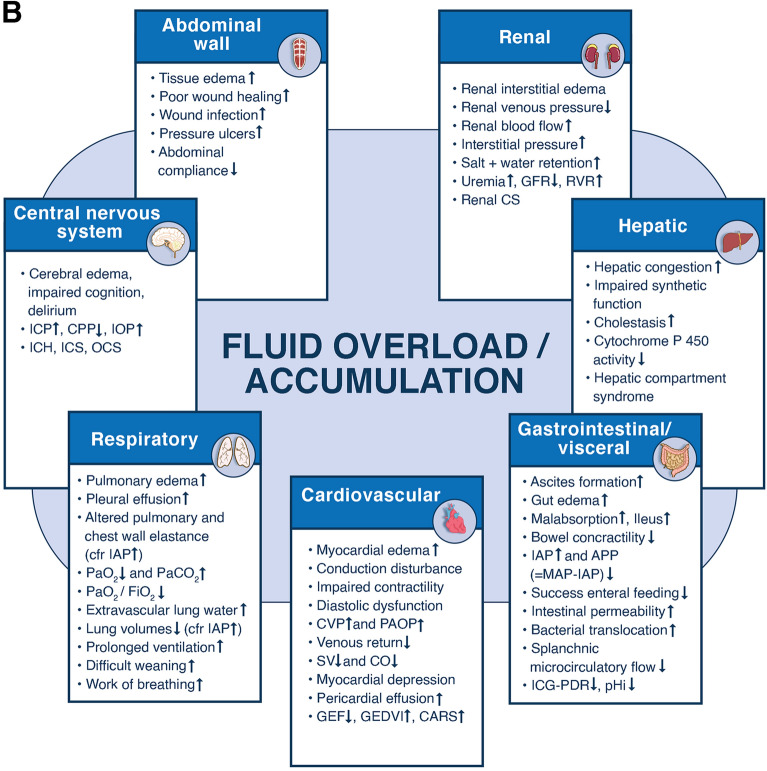
Fig. 1.
The 4 phases conceptual model and deleterious effects of fluid accumulation syndrome. Panel A The four-hit model of shock with evolution of patients’ cumulative fluid volume status over time during the five phases of resuscitation: Resuscitation (R), Optimization (O), Stabilization (S), and Evacuation (E) (ROSE), followed by a possible risk of Hypoperfusion in case of too aggressive deresuscitation. On admission patients are often hypovolemic, followed by normovolemia after fluid resuscitation (escalation or EAFM, early adequate fluid management), and possible fluid overload, again followed by a phase returning to normovolemia with de-escalation via achieving zero fluid balance or late conservative fluid management (LCFM) and followed by late goal directed fluid removal (LGFR) or deresuscitation. In case of hypovolemia, O2 cannot get into the tissue because of convective problems, in case of hypervolemia O2 cannot get into the tissue because of diffusion problems related to interstitial and pulmonary edema, gut edema (ileus and abdominal hypertension). *Volumetric preload indicators like GEDVI, LVEDAI, or RVEDVI are preferred over barometric ones like CVP or PAOP. **Vasopressor can be started or increased to maintain MAP/APP above 55/45 during deresuscitation phase. #Can only be measured via Swan-Ganz pulmonary artery catheter (PAC) and became obsolete. Panel B Potential consequences of fluid accumulation syndrome (formerly known as fluid overload) and GIPS (global increased permeability syndrome) on end-organ function. Figures adapted from Malbrain et al. with permission, according to the Open Access CC BY Licence 4.0 [2, 7]. ACS abdominal compartment syndrome, APP abdominal perfusion pressure = MAP-IAP, BIA bio-electrical impedance analysis, CARS cardio-abdominal-renal syndrome, CI cardiac index, CLI capillary leak index (serum CRP divided by serum albumin), CO cardiac output, COP colloid oncotic pressure, CPP cerebral perfusion pressure, CS compartment syndrome, CVP central venous pressure, ECW/ICW extracellular/intracellular water, EVLWI extra-vascular lung water index, FAS fluid accumulation syndrome, GEDVI global end-diastolic volume index, GEF global ejection fraction, GFR glomerular filtration rate, IAH intra-abdominal hypertension, IAP intra-abdominal pressure, ICG-PDR indocyanine green plasma disappearance rate, ICH intracranial hypertension, ICP intracranial pressure, ICS intracranial compartment syndrome, IOP intra-ocular pressure, IVCCI inferior vena cava collapsibility index, LVEDAI left ventricular end-diastolic area index, MAP mean arterial pressure, OCS ocular compartment syndrome, PAOP pulmonary artery occlusion pressure, PF PaO2 over FiO2 ratio, pHi gastric tonometry, PLR passive leg raising, PPV pulse pressure variation, PVPI pulmonary vascular permeability index, RVEDVI right ventricular end-diastolic volume index, RVR renal vascular resistance, ScvO2 central venous oxygen saturation, SSCG surviving sepsis campaign guidelines, SvO2 mixed venous oxygen saturation, SV stroke volume, SVV stroke volume variation, VE volume excess (from baseline body weight), VExUS venous congestion by ultrasound