Abstract
The present study examined whether adolescent attachment security and attachment-related representations moderate and mediate, respectively, the link between parent symptoms (depressive and anxiety) and adolescent depressive symptoms. Participants were 189 (118 girls) eleventh graders and their parents in a community sample. Results showed that adolescent attachment moderated the connection between parent and adolescent symptoms; in most cases attachment security was more protective if both parents were high on anxiety symptoms or if one parent was high on anxiety but the other parent was low on depressive symptoms. Mediational analyses indicated that representations of their mothers as a secure base mediated the link between maternal and adolescent depressive symptoms. Perceptions of fathers as a secure base did not play a mediating role, although paternal depressive symptoms were associated with lower perceptions of the father as a secure base. Neither parent’s anxiety symptoms were related to perceptions of the parent as a secure base or to adolescent depressive symptoms.
A well-documented body of research has demonstrated clear links between adolescent psychological functioning and that of their mothers and fathers (for reviews, see Downey & Coyne, 1990; Goodman & Gotlib, 1999). Moreover, although most of this research has focused on participants with clinical diagnoses, compelling evidence of links between parent and adolescent symptoms exists within community samples as well (e.g., Bosco, Renk, Dinger, Epstein, & Phares, 2003; Ge, Conger, Lorenz, Shanahan, & Elder, 1995). Several researchers have called for increased research examining moderating and mediating factors that might clarify the contexts and mechanisms underlying the connection between parent and adolescent symptoms (Connell & Goodman, 2002; Phares, 1996). Attachment theory and research lead to the possibility that adolescent attachment may help explain the link between parent and adolescent psychological symptoms because adolescent attachment is a central component of family relationships (e.g., Allen, 2008; Hazan & Zeifman, 1994) with important connections to the development of psychopathology (Allen, Hauser, & Borman-Spurrell, 1996; DeKlyen & Greenberg, 2008). The present study examines of how adolescent attachment and attachment-related representations may moderate and mediate, respectively, the links between parent and adolescent psychological symptoms in a community sample of high school students and their parents.
ADOLESCENT ATTACHMENT AS A MODERATOR OF THE LINKS BETWEEN PARENT AND ADOLESCENT SYMPTOMS
Attachment security during adolescence is typically examined through assessment of the adolescent’s “state of mind with respect to attachment” in the Adult Attachment Interview (AAI; George, Kaplan, & Main, 1984, 1985, 1996; see Hesse, 2008), which is thought to capture the adolescent’s history of experiences with multiple attachment figures as well as the organization of current cognitive and affective structures about these relationships. Adolescents classified as secure on the AAI value attachment relationships and have a set of representations that permit flexible assessment of their own and others’ feelings and behaviors in attachment-related circumstances, as well as a full range of emotions, including negative ones (Hesse, 2008). Secure adolescents tend to have had experiences in which distressing emotions are discussed, openly communicated, understood, and responded to effectively—experiences thought to contribute to a sense that negative emotions can be tolerated and safely faced (Cassidy & Kobak, 1988; Fonagy, Gergely, & Target, 2008; Kobak & Duemmler, 1994). In contrast, insecure children, who lack support when faced with distress, are likely to view distress as overwhelming and intolerable (Bowlby, 1986). Attachment security is thought to provide adolescents with capacities to function well in close relationships and to maintain positive representations of themselves and others even when under stress (Allen, 2008). Moreover, Main, Goldwyn, and Hesse (2002) describe the related construct of attachment “coherence of mind”—an individual’s ability to coherently communicate about his or her attachment-related experiences, including negative experiences of psychological distress—as a core component of attachment security.
Evidence from a variety of studies suggests that attachment security can act as a protective factor for children and adolescents. For instance, Dallaire and Weinraub (2007) found that infant attachment security was protective against anxiety in early childhood, and Sroufe, Egeland, Carlson, and Collins (2005) found that secure attachment buffered children from the negative effects of poverty. There are several reasons to believe that attachment may serve a similar protective function for adolescents whose parents exhibit elevated symptoms. First, it may be that secure adolescents have learned to discuss negative emotions and to seek support during times of distress (Cassidy & Kobak, 1988; Fonagy et al., 2008; Kobak & Duemmler, 1994). A second possibility is that attachment security is associated with a number of positive cognitive and social outcomes. Cognitions about others as supportive and about the self as competent and worthwhile are associated with secure attachment (Bowlby, 1973; Bretherton & Munholland, 2008; Cassidy, 1986), and such cognitions may insulate the adolescent from the harmful effects of parental symptoms. Moreover, attachment security is associated with better peer relationships and other sources of support (see Berlin, Cassidy, & Appleyard, 2008, and Thompson, 2008, for reviews), and these positive relationships with others may help to buffer secure adolescents from potential negative effects of parental symptoms. Thus, adolescents’ attachment could serve as a moderator whereby links between parent and adolescent symptoms exist not for more secure adolescents but only for more insecure adolescents.
It is important to examine the role of attachment in the context of other potential moderators. Phares and Compas (1992) and Cassano, Adrian, Veits, and Zeman (2006) noted that in studies of the development of children’s psychological difficulties, fathers’ symptoms are frequently either neglected entirely or examined using aggregated “parental symptom” variables that fail to differentiate which parent presents symptoms. In addition, Connell and Goodman (2002) noted that even with increasing recognition of the contributions that fathers make to their children’s functioning, results about fathers’ impact have been inconsistently reported. Moreover, several researchers have described the importance of considering more than main effects for each parent (Connell & Goodman, 2002; Landman-Peeters et al., 2008). Thus, one of the most important questions of moderation is whether the link between a parent’s psychological symptoms and those of his or her adolescent is moderated by the symptoms of the second parent. Given substantial evidence that both parents’ psychological functioning influences adolescent functioning (e.g., Bosco et al., 2003; Compas et al., 1989; Jacob & Johnson, 1997; Phares & Compas, 1992), research examining the cumulative and interactive effects of parental symptomatology provides additional information about psychosocial functioning within two-parent families (see Goodman & Gotlib, 1999, for a review).
In addition to examination of the moderating role of attachment when both mother and father are considered in the context of the family, it is also important to examine the moderating roles of different types of parental symptoms that often co-occur (Kessler et al., 1996; Merikangas, Prusoff, & Weissman, 1988). Previous work suggests that different types and combinations of parental symptoms may vary in how they relate to adolescent symptoms (Biederman, Rosenbaum, Bolduc, Faraone, & Hirshfeld, 1991; Sylvester, Hyde, & Reichler, 1987). Thus, an important question of moderation is whether the link between one aspect of a parent’s psychological symptoms and those of his or her adolescent is moderated by comorbid symptoms. We chose to examine anxiety as a comorbid symptom, given the high degree of co-occurrence of these two symptoms and because depressive and anxiety symptoms are relatively common in community samples (Kessler et al., 1996).
ATTACHMENT REPRESENTATIONS AS MEDIATORS OF THE LINK BETWEEN PARENT AND ADOLESCENT SYMPTOMS
Dweck and London (2004) emphasized the importance of studying children’s cognitive representations of their experiences as mediators of links between children’s exposure to negative situations (such as parent psychological symptoms) and outcomes for children. Little research has examined children’s and adolescents’ cognitive representations as mediating mechanisms in the link between parent symptoms and child depression, although Garber, Keiley, and Martin (2002) found that adolescents’ negative self-attributions mediated the link between maternal depression and the trajectory of adolescent depression. Although a number of studies have found an association between children’s and adolescents’ attachment representations and their psychological symptoms (e.g., Shirk, Gudmundsen, & Burwell, 2005), we are not aware of any study that examines attachment-related representations as a mediator of the association between parental and adolescent symptoms.
One possible mediator of the link between parental symptoms and adolescent depressive symptoms is adolescents’ representations of the parent as a secure base. According to Bowlby (1988), children and adolescents perceive their parents as a secure base when they have had a history of relationship experiences in which the parent has been available and supportive when needed. Thus, adolescents whose parents have heightened psychological symptoms may have experience-based representations of their parents as relatively unlikely to provide them with a secure base. Such representations, in turn, are thought to increase the likelihood of problematic functioning: As Bowlby (1988) noted, “as [an individual] grows into adolescence … a secure home base remains indispensable nonetheless for optimal functioning and mental health” (p. 122).
THE PRESENT STUDY
The central purpose of the present study was twofold: (a) to examine adolescent attachment as part of a set of theoretically important moderators of the link between parent psychological symptoms and adolescent depressive symptoms in community sample of 11th-grade high school students and their parents, and (b) to explore the role of adolescents’ attachment-related representations of the parent as a secure base as a potential mediator of the association between parent psychological symptoms and adolescent depressive symptoms in the same sample. We chose to focus on adolescent depressive symptoms because of depression’s status as one of the most prevalent mental health conditions world-wide (Murray & Lopez, 1996). In addition, we felt that it was important to consider both parental depressive and anxiety symptoms as separate risk factors for adolescent depressive symptoms, given evidence that adolescents whose parents have both depression and anxiety fare worse than adolescents whose parents have only one diagnosed disorder (Biederman et al., 1991; Sylvester et al., 1987). Our decision to focus on a community sample allows us to extend knowledge of psychosocial functioning in the large number of families that reflect the range of normally occurring variation. Despite evidence that systematic differences exist between youth who seek treatment and those who do not (Goodman et al., 1997) as well as between adults who are clinically referred and those who are not (e.g., Kendler, 1995), the meta-analysis by Connell and Goodman (2002) found no evidence of effect size differences in the contributions of parental symptoms to child adjustment based on whether clinical or community samples were used.
Since, as just stated, attachment has been found to be a protective factor, we asked whether attachment might be more protective in some combinations of parental symptoms than in others. For example, it is possible that attachment may be more protective in situations of higher risk, such as when both parents are highly symptomatic. Conversely, it may be that if risk is too high, security of attachment is no longer protective. Further, particular combinations of mother and father depressive and anxiety symptoms may interact with attachment differently. Because this is a relatively new area of research, we did not have specific hypotheses. Finally, we also examined a novel mediational model in which we hypothesized that adolescent attachment-related representations of a parent as a secure base would mediate the link between parent and adolescent symptoms. Notably, we examined “representations of the parent as a secure base” to examine adolescents’ views of a specific parent as a secure base (i.e., as an available and responsive caregiver when needed). Thus, we examined factors that may explain the mediational pathway through which a specific parent’s symptoms may be linked to the adolescent’s symptoms and the adolescent’s self-report of the extent to which that particular parent serves as a secure base.
METHOD
Participants
One hundred eighty-nine 11th-grade students (71 boys, 118 girls) and their parents were recruited from seven public high schools in the suburbs of a large metropolitan area to participate in a larger study about attachment and relationships. Seventy-three percent of participants were White/Caucasian, 14% were Black/African American, 10% were Asian, and 3% were Hispanic. More than 90% of parents reported having at least some college education, and 95% of families reported having an annual household income greater than $41,000. Families were paid $125 for their participation in the larger study.
Procedure
The data collection period took place during the spring/summer of adolescents’ junior year of high school. First, adolescents completed a packet of questionnaires, including the measure of depressive symptoms, in their classrooms. Next, in our university laboratory, mothers, fathers, and adolescents completed a variety of questionnaires, including measures pertaining to their psychological symptoms and representations of other family members as a secure base. Finally, adolescents completed the AAI in the laboratory. This study was approved by the University of Maryland’s Institutional Review Board. Parents provided informed consent and adolescent participation was considered to be adolescent assent.
Parent Measures
Center for Epidemiological Studies Scale for Depression (Radloff, 1977).
This widely used 20-item self-report measure was designed to assess depressive symptoms in the general population. Participants are asked to respond to each item by using a 4-point scale to indicate the frequency of symptoms during the past week. Radloff (1977) reported good psychometric properties across many populations, including good internal consistency, test–retest reliability, and convergent validity (see also Orme, Reis, & Herz, 1986). Alphas for this sample were .81 for the mothers and .82 for the fathers. Center for Epidemiological Studies Scale for Depression scores of 16 or greater are typically indicative of clinically significant depression (McDowell & Newell, 1996); 11.1% of the mothers and 9.4% of the fathers in our sample scored 16 or above.
Brief Symptom Inventory (BSI; Derogatis, 1993).
This 53-item self-report measure was designed to assess the psychological symptom patterns of adolescents and adults in nonpatient community, psychiatric, and medical settings. The items are rated on a 5-point scale from 0 (not at all) to 4 (extremely) with higher scores indicating greater symptomatology. The BSI assesses a variety of symptoms of distress; in the present study, we used the six-item Anxiety subscale. Following Derogatis, we used raw scores in all analyses because this is a nonclinical sample (L. R. Derogatis, personal communication, June 2003). Evidence of good internal consistency, test–retest reliability, and convergent validity has been reported for the BSI Anxiety scale (Derogatis, 1993). To our knowledge clinical cutoff scores are not currently available for the BSI Anxiety scale. The BSI Anxiety scale alpha coefficients in the present study were .72 for mothers and .76 for fathers.
Adolescent Measures
AAI (George et al., 1984, 1985, 1996).
The AAI is a 60-min semi-structured interview designed to assess adolescents’ and adults’ “current state of mind with respect to attachment” through a series of questions focused on memories of attachment-related experiences during early childhood (George et al., 1985; Hesse, 2008). Verbatim interview transcripts were rated on a series of 9-point scales that reflect the interviewee’s inferred attachment experiences (e.g., having a loving parent). Based on an integrated consideration of both inferred experience and state of mind with respect to attachment (e.g., valuing of attachment, dismissing of attachment), blind certified coders assigned one of four possible attachment classifications to the transcript: secure/autonomous, dismissing of attachment, preoccupied with attachment, and unresolved with respect to loss or abuse. The secure/autonomous classification is associated with coherent descriptions of childhood experiences (whether positive or negative). The remaining attachment classifications are associated with different patterns of incoherence in descriptions of attachment-related experiences. A number of studies have provided evidence of strong psychometric properties, including construct and divergent validity, and substantial stability of the AAI over 1 year (see Hesse, 2008). We used the “coherence of mind” scale score from the AAI, which is thought to represent the “best overall predictor [of] a speaker’s overall functioning insofar as it is related to attachment” (Main et al., 2002, p. 62). The use of a continuous measure of attachment security is a common technique to enhance statistical power (Hesse, 2008; Roisman, Fraley, & Belsky, 2007). A randomly selected 29% of cases (n = 55) were coded by at least two coders. Satisfactory interrater reliability emerged for the coherence of mind scale (ICC =.73).
Children’s Depression Inventory (Kovacs, 1985, 1992).
This 27-item self-report measure assesses symptoms of depression including disturbed mood, vegetative states, self-evaluative thoughts, and interpersonal behaviors in children between the ages of 7 and 17. School administrators requested that the suicidal ideation item be dropped, leaving 26 items (α = .85). For each item, adolescents were asked to select the sentence that best described them in the past 2 weeks from a cluster of three sentences. Each item was scored from 0 to 2 (possible total scores of 0–52). There is evidence to support the reliability and validity of the Children’s Depression Inventory (Kovacs, 1992; see also Craighead, Smucker, Craighead, & Ilardi, 1998, for evidence of good psychometric properties in a community sample in which the suicide item was dropped). The Cronbach’s alpha for the Children’s Depression Inventory in the present study was .85. Kovacs (1992) reported test–retest reliability coefficients of rs ranging from .74 to .82 over 2- to 3-week intervals across four studies with nonclinical samples. Scores at or above 20 are typically used as a clinical cut-off score; 7.4% of our sample reported scores at or above 20.
Parent as a Secure Base Scale—Revised (Cassidy & Woodhouse, 2003).
This 13-item scale was designed to assess the adolescent’s representations of each parent as a secure base (e.g., “My mother/father is someone I can count on when I need help.” “My mother/father is someone I can go to when I’m upset.”) Adolescents completed the measure separately for mothers and fathers. Each item was scored on a 5-point scale. Support for scale validity includes associations of this scale with attachment, with adolescent perceptions of parenting, such as perceptions of parental warmth and understanding (Cassidy, Ziv, Rodenberg, & Woodhouse, 2003; Dykas, Ziv, Woodhouse, & Cassidy, 2007), and with adolescents’ internalizing and externalizing symptoms (Woodhouse, Dykas, & Cassidy, 2009). The alpha coefficients in the present study were .91 for representations of mothers and .91 for representations of fathers. It is important to note that representations of the parent as a secure base are conceptualized to be different from measurement of attachment security on the AAI. As stated earlier, the AAI is intended to measure a general “state of mind with respect to attachment,” and is not intended to measure attachment to any one attachment figure (Hesse, 2008). Unlike the AAI, which explores attachment experiences with multiple attachment figures and focuses in particular on the ways in which the individual’s cognitive and affective organization relate to attachment experiences in general, measures of representations of the parent as a secure base capture the degree to which the adolescent reports perceptions that one specific parent serves as a secure base and provides support when needed.
RESULTS
Descriptive Statistics and Correlational Analyses
The 189 adolescents included 79 girls and 47 boys with secure attachments, and 38 girls and 24 boys with insecure attachments (and 1 adolescent who did not complete the AAI due to time constraints). The distribution of 67% of adolescents with secure attachments is identical to that reported in a meta-analysis of more than 1,500 mother–infant dyads (van IJzendoorn, Schuengel, & Bakermans-Kranenburg, 1999) and is comparable to that found in similar community samples of adolescents (i.e., Ammaniti, van IJzendoorn, Speranza, & Tambelli, 2000; Scharf, 2001). Correlations among all study variables, as well as means, standard deviations, and sample sizes, are presented in Table 1.
TABLE 1.
Intercorrelations and Descriptive Statistics for Adolescent and Parental Symptoms
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| 1. Adolescent Gender | — | −.12 | −.04 | .14* | .11 | −.01 | −.09 | .03 | −.02 | ||
| 2. Adolescent Depressive Symptoms | 9.80 | 6.32 | — | −.16** | −.37*** | −.30*** | .28*** | .13 | .12 | .12 | |
| 3. Adolescent Coherence of Mind | 5.51 | 1.92 | — | .28*** | .29*** | −.05 | −.07 | −.02 | −.01 | ||
| 4. Mother as a Secure Base | 56.69 | 7.80 | — | .60*** | −.27*** | −.14 | −.14 | −.12 | |||
| 5. Father as a Secure Base | 53.75 | 8.89 | — | −.22** | −.34*** | −.11 | −.21** | ||||
| 6. Maternal Depressive Symptoms | 7.25 | 6.17 | — | .11 | .45*** | .17** | |||||
| 7. Paternal Depressive Symptoms | 7.23 | 6.39 | — | −.08 | .60*** | ||||||
| 8. Maternal Anxiety Symptoms | 2.14 | 2.51 | — | .09 | |||||||
| 9. Paternal Anxiety Symptoms | 2.44 | 2.86 | — | ||||||||
p = .05.
p < .05.
p < .001.
Links Between Parental Psychosocial Functioning and Adolescent Depressive Symptoms: Moderational Analyses
We present the results of a hierarchical linear regression in which we examined predictors of adolescent depressive symptoms. Predictors in the first block included adolescent attachment, adolescent gender, maternal depressive symptoms, maternal anxiety symptoms, paternal depressive symptoms, and paternal anxiety symptoms. All continuous independent variables were standardized. The second block included two-way interaction terms that were necessary to examine the three-way interactions of interest examined in the third block (see Table 2). Because we had a particular interest in the moderating role of adolescent attachment, we included all possible three-way interactions involving adolescent attachment in the third block of the regression (see Table 2). We did not attempt to examine interactions at the four-way level or beyond due to the limitation of sample size. The results of the moderational anlysis are presented in terms of the degree to which coherence appeared to play a protective role in reducing adolescent depressive symptoms in the context of varying levels of mother and father psychological symptoms.
TABLE 2.
Summary of Hierarchical Multiple Regression Analysis for Prediction of Adolescent Depressive Symptoms from Adolescent Attachment (Coherence of Mind), Gender, and Parental Symptoms
| Predictor Variables | R2 | ΔR2 | ΔF | df1 | df2 | B | β | sr2 |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Block 1 | .12** | .12** | 3.64 | 6 | 158 | |||
| Coherence | −0.97 | −0.14 | .02 | |||||
| Adolescent Gender | −1.32 | −0.10 | .01 | |||||
| Maternal CES–D | 1.63** | 0.26 | .05 | |||||
| Paternal CES–D | 0.45 | 0.07 | .00 | |||||
| Maternal ANX | 0.05 | 0.01 | .00 | |||||
| Paternal ANX | 0.25 | 0.04 | .00 | |||||
| Block 2 | .20** | .08 | 1.91 | 8 | 150 | |||
| Coherence | −1.08 | −0.16 | .02 | |||||
| Adolescent Gender | −1.37 | −0.10 | .01 | |||||
| Maternal CES–D | 1.34* | 0.21 | .03 | |||||
| Paternal CES–D | 0.74 | 0.12 | .01 | |||||
| Maternal ANX | 0.61 | 0.09 | .01 | |||||
| Paternal ANX | 0.30 | 0.05 | .00 | |||||
| Coherence × Maternal CES–D | 0.71 | 0.11 | .01 | |||||
| Coherence × Paternal CES–D | 0.50 | 0.08 | .00 | |||||
| Coherence × Maternal ANX | 0.02 | 0.00 | .00 | |||||
| Coherence × Paternal ANX | −0.85 | −0.13 | .01 | |||||
| Maternal CES-D × Paternal CES–D | −1.18 | −0.17 | .01 | |||||
| Maternal ANX × Paternal ANX | −1.51* | −0.24 | .03 | |||||
| Maternal CES-D × Paternal ANX | 0.12 | 0.02 | .00 | |||||
| Maternal ANX × Paternal CES–D | 1.15 | 0.19 | .02 | |||||
| Block 3 | .26** | .06* | 2.81 | 4 | 146 | |||
| Coherence | −0.93 | −0.14 | .01 | |||||
| Adolescent Gender | −1.09 | −0.08 | .01 | |||||
| Maternal CES–D | 1.40* | 0.22 | .03 | |||||
| Paternal CES–D | 0.99 | 0.15 | .01 | |||||
| Maternal ANX | 0.87 | 0.13 | .01 | |||||
| Paternal ANX | 0.34 | 0.05 | .00 | |||||
| Coherence × Maternal CES–D | 0.86 | 0.14 | .01 | |||||
| Coherence × Paternal CES–D | 1.13 | 0.17 | .01 | |||||
| Coherence × Maternal ANX | −0.36 | −0.05 | .00 | |||||
| Coherence × Paternal ANX | −1.46* | −0.23 | .02 | |||||
| Maternal CES-D × Paternal CES–D | −2.06* | −0.30 | .03 | |||||
| Maternal ANX × Paternal ANX | −2.16** | −0.35 | .05 | |||||
| Maternal CES-D × Paternal ANX | 1.43 | 0.24 | .02 | |||||
| Maternal ANX × Paternal CES–D | 1.95** | 0.32 | .04 | |||||
| Coherence × Maternal CES-D × Paternal CES–D | −1.45 | −0.26 | .01 | |||||
| Coherence × Maternal ANX × Paternal ANX | −2.27* | −0.42 | .03 | |||||
| Coherence × Maternal CES-D × Paternal ANX | 1.43* | 0.31 | .02 | |||||
| Coherence × Maternal ANX × Paternal CES–D | 2.67** | 0.56 | .04 | |||||
Note: n = 165. CES–D = Center for Epidemiological Studies Scale for Depression. ANX = Brief Symptom Inventory Anxiety Scale.
p < .05.
p < .01.
Although the measures of parental symptoms were correlated with one another within parent and in some cases across parents (see Table 1), we were not concerned about multicollinearity because none of the correlations reached the generally accepted cutoff point of .70 (Tabachnick & Fidell, 1996). Further, VIF statistics for the main effect terms in the regression ranged from 1.01 to 1.63, also indicating no problem with multicollinearity. Because we tested several two-way and three-way interactions, we used G*Power (Faul, Erdfelder, Lang, & Buchner, 2007) to perform post hoc power calculations to ensure that we had sufficient power to detect these interactions. For each block we used G*Power to calculate the effect sizes from the variances, the alpha level was entered as .05, and the numerator df and number of predictors were entered from the regression. Results of the post hoc power analyses indicated that power for Block 1 was .96, power for Block 2 to detect effects above and beyond Block 1 was .83, and power for Block 3 to detect effects above and beyond Blocks 1 and 2 was .81. Thus, we concluded that we had had sufficient power to proceed with interpretation of the results obtained in the hierarchical regression analysis.
As indicated in Table 2, Block 1 of the regression was significant. In this first block, the only significant predictor was maternal depressive symptoms, with greater maternal depressive symptoms linked to greater adolescent depressive symptoms. Block 2 was not significant at conventional levels of alpha; thus it appeared that Block 2 did not add significantly to explaining the variance above and beyond Block 1. Block 3, however, was significant. Three three-way interactions were significant. Using procedures recommended by Aiken and West (1991), we plotted each interaction and evaluated differences between slopes of the plotted lines following procedures outlined by Dawson and Richter (2006). Dawson and Richter argued compellingly that their method resolves many of the problems inherent in other methods for probing three-way interactions and allows the additional benefit of being able to statistically test differences between slopes of all the lines so as to make comparative statements.
The first significant three-way interaction was that of Adolescent Attachment Coherence × Mother Anxiety Symptoms × Father Anxiety Symptoms (see Figure 1a). Because six pairs of slopes were tested, it was important to consider adjusting alpha via a Bonferroni correction, such that the adjusted alpha was set to .0083. Using a Bonferroni correction, tests of significant slope differences resulted in identification of a significant difference between the slopes of Lines 1 and 2 (t = −3.07, p = .003). This significant slope difference indicated that when both parents were high on anxiety symptoms, attachment coherence was significantly more protective against adolescent depressive symptoms than when only mother (and not father) anxiety symptoms were high. Given the exploratory nature of beginning to examine the interactions between adolescent attachment and parental symptoms, we believed there was also some justification for considering comparisons of significant differences between slopes at the less stringent level of α = .05. These tests revealed two additional significant slope differences. When both parents were high on anxiety symptoms, higher levels of adolescent coherence were associated with lower adolescent depressive symptoms than (a) when only father anxiety symptoms (and not mother anxiety symptoms) were high (slopes of Lines 1 vs. 3; t = −2.27, p = .024), and (b) when both parents were low on anxiety symptoms (slopes of Lines 1 vs. 4; t = −1.98, p = .05). Taken together, these findings suggest that attachment coherence serves a more protective role with regard to adolescent depressive symptoms in the context of both parents reporting higher levels of anxiety symptoms than when either only one parent or neither parent was experiencing higher levels of anxiety symptoms.
FIGURE 1.
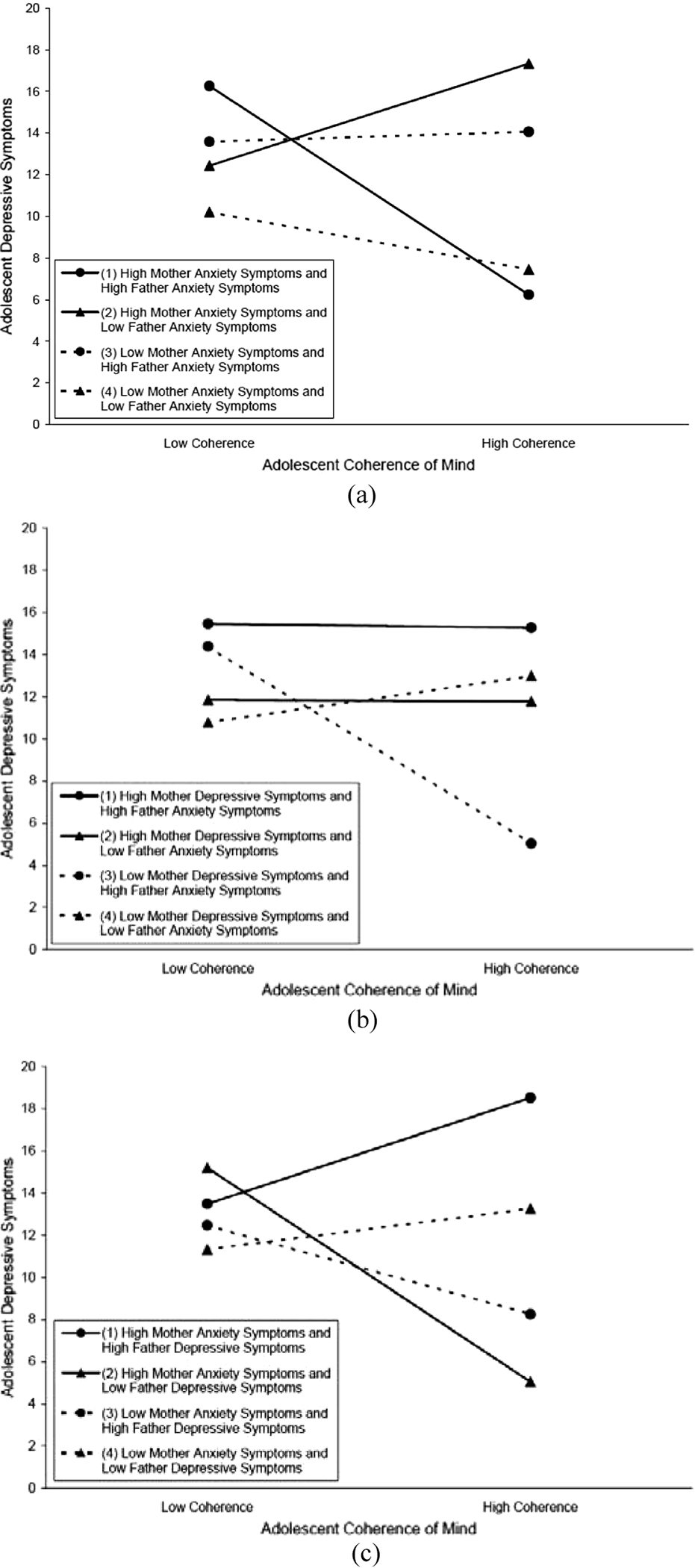
Three-way interactions predicting adolescent depressive symptoms as a function of adolescent coherence of mind and parental symptoms. (a) Adolescent depressive symptoms as a function of the interaction among adolescent coherence of mind, maternal anxiety symptoms, and paternal anxiety symptoms. (b) Adolescent depressive symptoms as a function of the interaction among adolescent coherence of mind, maternal depressive symptoms, and paternal anxiety symptoms. (c) Adolescent depressive symptoms as a function of the interaction among adolescent coherence of mind, maternal anxiety symptoms, and paternal depressive symptoms.
The second significant three-way interaction was that of Adolescent Attachment Coherence × Mother Depressive Symptoms × Father Anxiety Symptoms (see Figure 1b). Although there were no pairs of slopes that were significantly different at the Bonferroni-corrected level of α = .0083, there were three significant slope differences at the α = .05 level. If father anxiety symptoms were high and mother depressive symptoms were low, coherence appeared to play a significantly more protective role with regard to adolescent depressive symptoms than (a) if father anxiety symptoms were high and mother depressive symptoms were high (slopes of Lines 3 vs. 1; t = 2.66, p = .009) and (b) if father anxiety symptoms were low and mother depressive symptoms were either low (slopes of Lines 3 vs. 4; t = −2.65, p = .009) or high (slopes of Lines 3 vs. 2; t = 2.39, p = .018).
The third significant three-way interaction was that of Adolescent Attachment Coherence × Mother Anxiety Symptoms × Father Depressive Symptoms (see Figure 1c). Probing of this interaction revealed a pattern of results largely parallel to results for the previous interaction. As before, using a Bonferroni correction, coherence appeared to play a significantly more protective role with regard to adolescent depressive symptoms if mother anxiety symptoms were high and father depressive symptoms were low than (a) if mother anxiety symptoms were high but father depressive symptoms were high (slopes for Lines 2 vs. 1; t = 2.98, p = −2.61, p = .010). The single departure from the previous pattern was that coherence was significantly more protective regarding adolescent depressive symptoms when mother anxiety symptoms were low and father depressive symptoms were high than if both mother anxiety symptoms and father depressive symptoms were high (slopes for Lines 3 vs. 1; t = 2.24, p = .027). This was the only instance in which a protective effect for coherence was found in the context of one parent being low on anxiety symptoms and the other parent being high on depressive symptoms.
Connections Between Parent and Adolescent Psychosocial Functioning: Mediational Analysis
The hypothesized path model predicted adolescent depressive symptoms from all four measures of parental functioning (maternal and paternal depressive and anxiety symptoms). In addition, adolescent representations of mother as a secure base and of father as a secure base were each posited as mediators of the relations between parent and adolescent symptoms. See Figure 2 for variables that were allowed to covary. Complete data were available for 166 adolescents. The path model was fit to the data using AMOS’s maximum likelihood estimation techniques. The set of path weights that best reproduced the variance–covariance matrix characterizing our data was generated. To determine the model fit for our analysis, we used the joint criteria suggested by Hu and Bentler (1999) of a comparative fit index (CFI) of .96 or more in conjunction with a standardized root mean residual (SRMR) of .10 or less.
FIGURE 2.
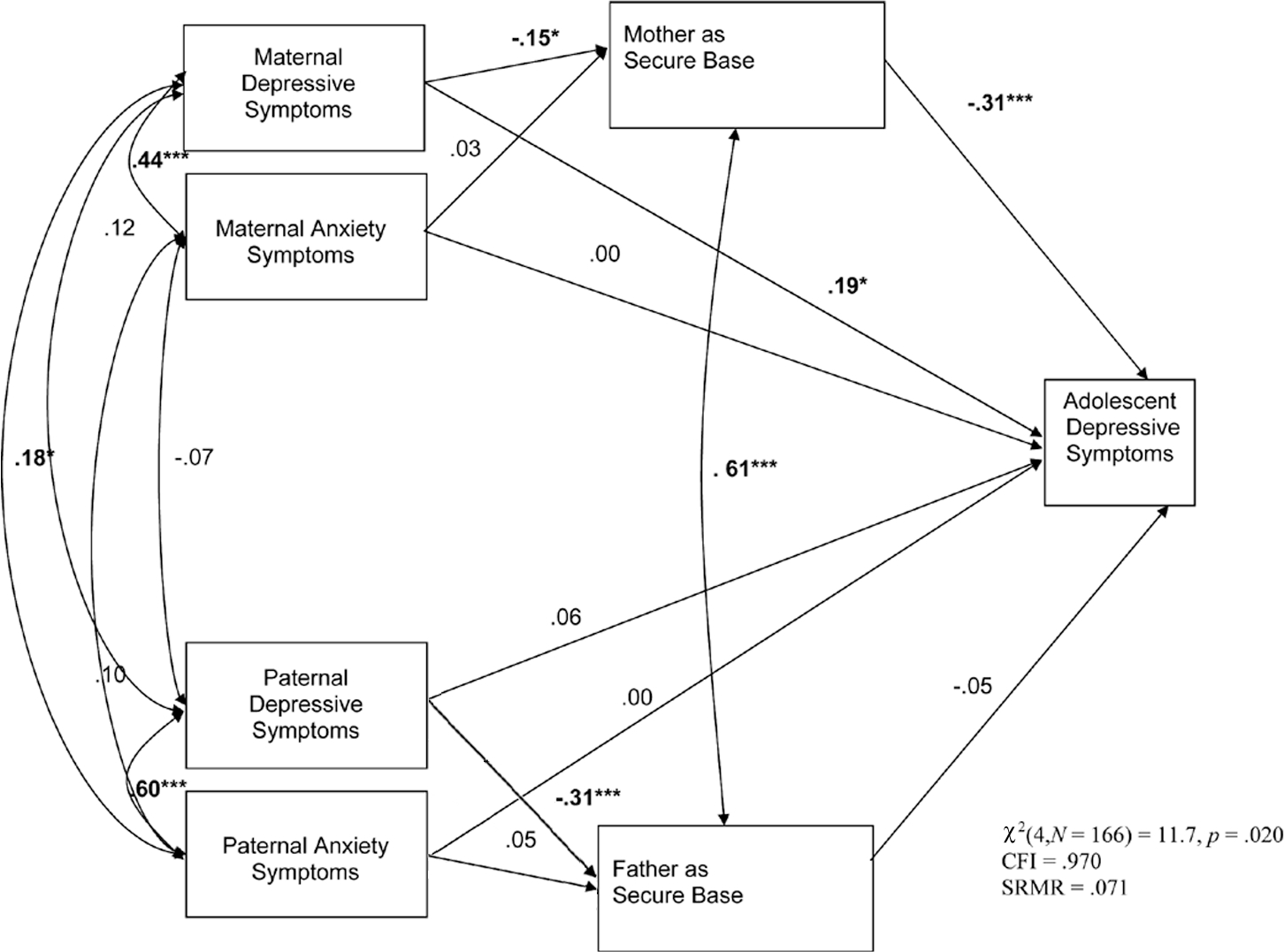
Path analysis of the mediating role of adolescent perceptions of parents as a secure base in the link between parental symptoms and adolescent symptoms (n = 166). Note: All path coefficients are standardized (beta-weights).
As presented in Figure 2, although χ2(4) = 11.7, p = .02, the resulting path model fit the data well (CFI = .970, SRMR = .071). As expected, mothers’ depressive symptoms negatively predicted adolescents’ representations of the mother as secure base, and fathers’ depressive symptoms negatively predicted adolescents’ representations of the father as secure base. In contrast to expectations, neither mothers’ nor fathers’ anxiety symptoms predicted adolescents’ secure base representations. As hypothesized, representations of mother as a secure base mediated the relation between maternal depressive symptoms and adolescents’ depressive symptoms; unexpectedly, however, maternal depressive symptoms also had a direct effect on adolescents’ depressive symptoms. In contrast, there was no mediating role of representations of father, which were not related to adolescent symptoms.
DISCUSSION
The Moderating Role of Attachment Coherence of Mind
The central study findings were that adolescent attachment security moderated the link between parent symptoms and adolescent depressive symptoms, such that results were consistent with the notion that secure attachment plays a protective role in some situations. This protective role, however, was particularly evident in the context of parental anxiety symptoms as opposed to the context of depressive symptoms. In every case but one, attachment security was associated with significantly greater protection from depressive symptoms either when both parents were high on anxiety symptoms or when one parent was high on anxiety symptoms and the other parent was low on depressive symptoms.
It is interesting that attachment security emerged as a protective factor primarily in the context of parental anxiety symptoms (as opposed to parental depressive symptoms). Bowlby (1969/1982) theorized that the attachment system evolved in conjunction with the fear system to enhance the survival of the child. When circumstances become stressful or threatening, both the fear system and attachment system become activated and the child seeks proximity to and protection from the attachment figure, and indeed there is experimental evidence that the attachment figure’s availability and responsiveness help to reduce a child’s fearfulness (Sorce & Emde, 1981). It is possible that if both parents are high in anxiety, the adolescent may see the world reflected in the parents’ eyes as a threatening place. Insecure adolescents may respond to this sense of threat with depressive symptoms because they lack a sense that they can turn to others when needed or that they are worthy to receive care during times of threat. On the other hand, adolescents with secure attachments may have a history of experiences that help them to feel confident and secure regardless of parent symptoms of anxiety. Typically secure adolescents have had positive attachment-related experiences with parents in the past, such that parents have been available when needed. Such adolescents would be less likely to give up and experience depressive symptoms when a threat is perceived because they are more likely to have a sense that parents will be available as needed.
Perhaps attachment security was not protective in the context of depression symptoms because depressive symptoms tend to immobilize the parent and thus interfere with the adolescent’s trust that the parent will be available if needed to provide protection or support. Although an adolescent may generally have a secure state of mind with respect to attachment, he or she may not trust that the parents will be able to be responsive when needed. Thus, adolescents with secure attachments may give up in the face of such parental immobilization and experience depressive symptoms. For this reason, attachment security may not be protective in most contexts in which parents are experiencing depressive symptoms. Further research is needed to explore this possibility.
The Mediating Role of Representations of Parent as a Secure Base
Our finding that, as expected, adolescents’ secure base representations of the mother served as a partial mediator between mother depressive symptoms and adolescent depressive symptoms is congruent with two central tenets of attachment theory: that is, parents with psychosocial difficulties are less able to provide a secure base for their children, and the lack of a parental secure base leads to problematic psychosocial functioning for offspring. This finding that maternal depressive symptoms were linked with perceptions of reduced secure base provision meshes with the substantial literature showing that symptomatic mothers have difficulties serving as a secure base for their infants (Campbell et al., 2004). Research with infants and young children has also long provided evidence of the importance of a secure base for well-being (Ainsworth, Blehar, Waters, & Wall, 1978; Sorce & Emde, 1981; Thompson, 2008), and more recent fMRI data indicate that this connection holds later in life as well (Coan, Schaefer, & Davidson, 2006). Moreover, the fact that both mothers’ and fathers’ depressive symptoms were linked to lower adolescent representations of parent as secure base is consistent with the idea that attachment security may not be protective in the context of parental depressive symptoms because depressive symptoms interfere with parental availability to the child.
As expected, maternal depressive symptoms were linked directly to adolescents’ depressive symptoms, and this link was not fully mediated by adolescents’ representations of the mother as a secure base. Given the evidence for the heritability of depressive disorders (Lopez-Leon et al., 2008; McGuffin, Katz, Watkins, & Rutherford, 1996), genetic factors may also influence the direct link observed. There may also be other factors involved. For example, mothers with depressive symptoms may vary in their capacity to manage their symptoms and provide a secure base, whereas adolescents may tend to respond consistently with sadness to their mothers’ sadness.
It is interesting to speculate about why adolescents’ representations of the mother as a secure base were linked to adolescents’ depressive symptoms, but their representations of father as a secure base were not (although note that fathers’ depressive symptoms were linked to adolescents’ representations of them as a secure base). Observational data indicate that adolescents engage in more emotionally charged and intimate interactions, both positive and negative ones, with their mothers than with their fathers (Larson & Richards, 1994; Youniss & Smollar, 1985). Feelings that the mother is not reliable as a secure base may be particularly problematic and may contribute to adolescent depressive symptoms given that it is the relationship with the mother that is typically most emotionally close.
Implications for Research, Policy, and Practice
In terms of future research, this work can be extended in several important ways. It is important to note the preliminary nature of the present results and the need for replication in order to better understand complex, higher order interactions in the family. Such higher order interactions are of great theoretical and practical interest. Nevertheless, three-way interactions are notoriously difficult to detect because the terms tend to be highly colinear and tend to create suppression effects. Limitations in the sample size of the present study may limit the stability of the interactions found. Thus, replication will be very important. It will also be important to examine these processes in more at-risk and clinically symptomatic family samples. This sample was a community sample of middle-class, intact families. In a sample of clinically diagnosed parents, the moderating influence of attachment security might disappear. For example, any protective effects of attachment security may be overwhelmed by high levels of parental psychopathology. It is also important to note that all of the participating families were intact, two-parent families; thus, results may not be generalizable to other family constellations. Moreover, it is unclear whether self-selecting participating families differed systematically from families who chose not to participate.
The cross-sectional design of our study brings with it several limitations that could be addressed by longitudinal, prospective studies. Longitudinal studies will allow examination of whether attachment continues to play the same protective role over time. Moreover, because of the “snapshot” nature of our data, we are unable to determine the temporal order of effects for parent and adolescent symptoms. Our model, along with most previous conceptualizations, has focused on the influence of parents’ symptoms on their offsprings’ depressive symptoms. There has been increasing recognition, however, of transactional reciprocal processes wherein offspring influence their parents as well (Patterson, 1982). In addition, of course, a third variable may be the causal influence of both parental and adolescent symptoms. Although the few longitudinal studies that have attempted to examine temporal relations between parental and child functioning have yielded mixed findings, across studies there is support for the proposition of mutual influence (see Elgar, McGrath, Waschbusch, Stewart, & Curtis, 2004, for discussion and review). Thus, an alternate model for the moderating effects in the present data could be that the parents of secure adolescents become anxious themselves in response to the symptoms they observe in their children. Future longitudinal work examining the temporal order of parent and adolescent symptoms is important.
In terms of policy and practice, it is important to note that because we know that attachment security may play a role in buffering the effects of parental anxiety symptoms on adolescent depressive symptoms, it may be beneficial for professionals to attend to the relationship between parents and their adolescents when parents experience anxiety symptoms. Moreover, adolescents living with symptomatic parents may benefit from other sources of interpersonal support in addition to professional services, such as supportive relationships and activities with other relatives, school counselors, support groups, and community groups. Such relationships may help to provide a secure base with others besides parents that could potentially help to buffer adolescents from negative effects of parental symptoms. Because the buffering effects of attachment security in the context of parental anxiety seem to disappear if the other parent is high in depressive symptoms, efforts to improve attachment may prove difficult if symptoms interfere with secure base provision. In such cases, clinical attention to the adolescent may be helpful.
In addition, the evidence for the mediating role of adolescents’ representations of mothers as a secure base in the link between maternal depressive symptoms and adolescents’ depression indicates that it might be useful for professionals to work with symptomatic mothers to provide a secure base despite ongoing symptoms. It may be helpful for clinicians to assist symptomatic mothers and adolescents to communicate openly in therapy about what would help the adolescent feel greater maternal support. In addition, helping adolescents living with a symptomatic mother to build other sources of support, as just described, may also help to reduce symptoms in adolescents.
Acknowledgments
Stephanie Warner is now at St. Luke’s House, Inc., Bethesda, Maryland. This research was supported by Grant HD36635 from the National Institute for Child Health and Human Development to Jude Cassidy. Fatima Ramos-Marcuse was supported by Grant MH58907 from the National Institute of Mental Health. Portions of this research were presented at the biennial meetings of the Society for Research in Child Development in Atlanta (2005) and Boston (2007). We thank the students who participated in this research. We also thank Steven Bottjer, Jeremy Rachlin, Elizabeth Mizrek, and Jessica Smith for their assistance with data collection; Mindy Rodenberg Cabrera for supervising data collection; and Jonathan Mohr for his helpful comments on an earlier draft. We are grateful to Inbal Kivenson Bar-On, Mindy Rodenberg Cabrera, June Sroufe, Sue Watson, and Marina Zelenko for coding the attachment interviews used in this study.
Contributor Information
Susan S. Woodhouse, Department of Counselor Education, Counseling Psychology, and Rehabilitation Services, Pennsylvania State University
Fatima Ramos-Marcuse, University of Maryland School of Nursing.
Katherine B. Ehrlich, Department of Psychology, University of Maryland at College Park
Stephanie Warner, Department of Psychology, University of Maryland at College Park.
Jude Cassidy, Department of Psychology, University of Maryland at College Park.
REFERENCES
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage. [Google Scholar]
- Ainsworth MDS, Blehar MC, Waters E, & Wall S (1978). Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Allen JP (2008). The attachment system in adolescence. In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 419–435). New York: Guilford. [Google Scholar]
- Allen JP, Hauser ST, & Borman-Spurrell E (1996). Attachment theory as a framework for understanding sequelae of severe adolescent psychopathology: An 11-year follow-up study. Journal of Consulting and Clinical Psychology, 64, 254–263. [DOI] [PubMed] [Google Scholar]
- Ammaniti M, van IJzendoorn MH, Speranza AM, & Tambelli R (2000). Internal working models of attachment during late childhood and early adolescence: An exploration of stability and change. Attachment and Human Development, 2, 328–346. [DOI] [PubMed] [Google Scholar]
- Berlin LJ, Cassidy J, & Appleyard K (2008). The influence of early attachments on other relationships. In Cassidy J & Shaver PR (Eds.), The handbook of attachment: Theory, research and clinical applications (2nd ed., pp. 333–347). New York: Guilford. [Google Scholar]
- Biederman J, Rosenbaum JF, Bolduc EA, Faraone SV, & Hirshfeld DR (1991). A high risk study of young children of parents with panic disorder and agoraphobia with and without comorbid major depression. Psychiatry Research, 37, 333–348. [DOI] [PubMed] [Google Scholar]
- Bosco GL, Renk K, Dinger TM, Epstein MK, & Phares V (2003). The connections between adolescents’ perceptions of parents, parental psychological symptoms, and adolescent functioning. Applied Developmental Psychology, 24, 179–200. [Google Scholar]
- Bowlby J (1973). Attachment and loss: Vol. 2. Separation. New York: Basic Books. [Google Scholar]
- Bowlby J (1982). Attachment and loss: Vol. 1. Attachment. New York: Basic Books. (Original work published 1969) [Google Scholar]
- Bowlby J (1986). The nature of the child’s tie to his mother. In Buckley P (Ed.), Essential papers on object relations (pp. 153–199). New York: New York University Press. [Google Scholar]
- Bowlby J (1988). A secure base: Parent–child attachment and healthy human development. New York: Basic Books. [Google Scholar]
- Bretherton I, & Munholland KA (2008). Internal working models in attachment relationships: Elaborating a central construct in attachment theory. In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 102–127). New York: Guilford. [Google Scholar]
- Campbell SB, Brownell CA, Hungerford A, Spieker SJ, Mohan R, & Blessing JS (2004). The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Development and Psychopathology, 16, 231–252. [DOI] [PubMed] [Google Scholar]
- Cassano M, Adrian M, Veits G, & Zeman J (2006). The inclusion of fathers in the empirical investigation of child psychopathology: An update. Journal of Clinical Child and Adolescent Psychology, 35, 583–589. [DOI] [PubMed] [Google Scholar]
- Cassidy J (1986). The ability to negotiate the environment: An aspect of infant competence as related to quality of attachment. Child Development, 57, 331–337. [Google Scholar]
- Cassidy J, & Kobak RR (1988). Avoidance and its relation to other defensive processes. In Belsky J & Nezworski T (Eds.), Clinical implications of attachment (pp. 300–323). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cassidy J, & Woodhouse S (2003). The Secure Base Scale–Revised. Unpublished manuscript. [Google Scholar]
- Cassidy J, Ziv Y, Rodenberg M, & Woodhouse SS (2003, April). Adolescent perceptions of parents: Associations with adolescent attachment (AAI) and interactions with parents. In Kobak (Chair) R, Assessing attachment in middle childhood and adolescence: Toward a multi-method approach. Symposium conducted at the biennial meeting of the Society for Research in Child Development, Tampa, FL. [Google Scholar]
- Coan JA, Schaefer HS, & Davidson RJ (2006). Lending a hand: Social regulation of the neural response to threat. Psychological Science, 17, 1032–1039. [DOI] [PubMed] [Google Scholar]
- Compas BE, Howell DC, Phares V, Williams RA, & Ledoux N (1989). Parent and child stress and symptoms: An integrative analysis. Developmental Psychology, 25, 550–559. [Google Scholar]
- Connell AM, & Goodman SH (2002). The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin, 128, 746–773. [DOI] [PubMed] [Google Scholar]
- Craighead WE, Smucker MR, Craighead LW, & Ilardi SS (1998). Factor analysis of the Children’s Depression Inventory in a community sample. Psychological Assessment, 10, 156–165. [Google Scholar]
- Dallaire DH, & Weinraub M (2007). Infant–mother attachment security and children’s anxiety and aggression at first grade. Journal of Applied Developmental Psychology, 28, 477–492. [Google Scholar]
- Dawson JF, & Richter AW (2006). Probing three-way interactions in moderated multiple regression: Development and application of a slope difference test. Journal of Applied Psychology, 91, 917–926. [DOI] [PubMed] [Google Scholar]
- DeKlyen M, & Greenberg MT (2008). Attachment and psychopathology in childhood. In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 637–665). New York: Guilford. [Google Scholar]
- Derogatis LR (1993). Brief Symptom Inventory (BSI): Administration, scoring, and procedures manual. Baltimore: Clinical Psychometric Research. [Google Scholar]
- Downey G, & Coyne JC (1990). Children of depressed parents: An integrative review. Psychological Bulletin, 108, 50–76. [DOI] [PubMed] [Google Scholar]
- Dweck C, & London B (2004). The role of mental representation in social development. Merrill-Palmer Quarterly, 50, 428–444. [Google Scholar]
- Dykas MJ, Ziv Y, Woodhouse SS, & Cassidy J (2007). Internal working models of attachment in adolescence: How do adolescent attachment organization, representations, and styles relate to one another and to adolescent–parent interaction? Unpublished manuscript.
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, & Curtis LJ (2004). Mutual influences on maternal depression and child adjustment problems. Clinical Psychology Review, 24, 441–459. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Gergely G, & Target M (2008). Psychoanalytic theory from the viewpoint of attachment theory and research. In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 783–810). New York: Guilford. [Google Scholar]
- Garber J, Keiley MK, & Martin NC (2002). Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology, 70, 79–95. [DOI] [PubMed] [Google Scholar]
- Ge X, Conger RD, Lorenz FO, Shanahan M, & Elder GH (1995). Mutual influences in parent and adolescent distress. Developmental Psychology, 31, 406–419. [Google Scholar]
- George C, Kaplan N, & Main M (1984). Adult attachment interview protocol. Unpublished manuscript, University of California at Berkeley. [Google Scholar]
- George C, Kaplan N, & Main M (1985). Adult attachment interview protocol (2nd ed.). Unpublished manuscript, University of California at Berkeley. [Google Scholar]
- George C, Kaplan N, & Main M (1996). Adult attachment interview protocol (3rd ed.). Unpublished manuscript, University of California at Berkeley. [Google Scholar]
- Goodman SH, & Gotlib IH (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Lahey BB, Fielding B, Dulcan M, Narrow W, & Regier D (1997). Representativeness of clinical samples of youths with mental disorders: A preliminary population-based study. Journal of Abnormal Psychology, 106, 3–14. [DOI] [PubMed] [Google Scholar]
- Hazan C, & Zeifman D (1994). Sex and the psychological tether. In Bartholomew K & Perlman D (Eds.), Attachment processes in adulthood (pp. 151–178). Philadelphia: Jessica Kingsley. [Google Scholar]
- Hesse E (2008). The Adult Attachment Interview: Historical and current perspectives. In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 552–598). New York: Guilford. [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Jacob T, & Johnson SL (1997). Parent–child interaction among depressed fathers and mothers: Impact on child functioning. Journal of Family Psychology, 11, 391–409. [PubMed] [Google Scholar]
- Kendler K (1995). Is treatment for depression predicted by a history of depression in relatives? Implications for family studies of affective disorder. Psychological Medicine, 25, 807–814. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Liu J, Swartz MS, & Blazer DG (1996). Comorbidity of DSM–III—R major depressive disorder in the general population: Results from the US National Comorbidity Survey. British Journal of Psychiatry, 168, 17–30. [PubMed] [Google Scholar]
- Kobak RR, & Duemmler S (1994). Attachment and conversation: Toward a discourse analysis of adolescent and adult security. In Bartholomew K & Perlman D (Eds.), Attachment processes in adulthood (pp. 121–149). London: Kingsley. [Google Scholar]
- Kovacs M (1985). The Children’s Depression Inventory. Psychopharmacology Bulletin, 21, 995–1124. [PubMed] [Google Scholar]
- Kovacs M (1992). Children’s Depression Inventory manual. New York: Multi-Health Systems. [Google Scholar]
- Landman-Peeters KMC, Ormel J, Van Sonderen ELP, Den Boer JA, Minderaa RB, & Hartman CA (2008). Risk of emotional disorder in offspring of depressed parents: Gender differences in the effect of a second emotionally affected parent. Depression and Anxiety, 25, 653–660. [DOI] [PubMed] [Google Scholar]
- Larson R, & Richards MH (1994). Divergent realities: The emotional lives of mothers, fathers, and adolescents. New York: Basic Books. [Google Scholar]
- Lopez-Leon S, Janssens AC, Gonzalez-Zuloeta Ladd AM, Del-Favero J, Claes SJ, Oostra BA, et al. (2008). Meta-analyses of genetic studies on major depressive disorder. Molecular Psychiatry, 13, 772–785. [DOI] [PubMed] [Google Scholar]
- Main M, Goldwyn R, & Hesse E (2002). Adult attachment scoring and classification system. Version 7.2. Unpublished manuscript, University of California at Berkeley. [Google Scholar]
- McDowell I, & Newell C (1996). Measuring health: A guide to rating scales and questionnaires (2nd ed.). New York: Oxford. [Google Scholar]
- McGuffin P, Katz R, Watkins S, & Rutherford J (1996). A hospital-based twin registry study of the heritability of DSM–IV unipolar depression. Archives of General Psychiatry, 53, 129–136. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Prusoff BA, & Weissman MM (1988). Parental concordance for affective disorders: Psychopathology in offspring. Journal of Affective Disorders, 15, 279–290. [DOI] [PubMed] [Google Scholar]
- Murray CJL, & Lopez AD (Eds.). (1996). The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press. [Google Scholar]
- Orme JG, Reis J, & Herz EJ (1986). Factorial and discriminant validity of the Center for Epidemiological Studies Depression (CES–D) scale. Journal of Clinical Psychology, 42, 28–33. [DOI] [PubMed] [Google Scholar]
- Patterson GR (1982). Coercive family process. Eugene, OR: Castalia. [Google Scholar]
- Phares V (1996). Fathers and developmental psychopathology. New York: Wiley. [Google Scholar]
- Phares V, & Compas BE (1992). The role of fathers in child and adolescent psychopathology: Make room for daddy. Psychological Bulletin, 111, 387–412. [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES–D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Roisman GI, Fraley RC, & Belsky J (2007). A taxometric study of the Adult Attachment Interview. Developmental Psychology, 43, 675–686. [DOI] [PubMed] [Google Scholar]
- Scharf M (2001). A “natural experiment” in childrearing ecologies and adolescents’ attachment and separation representations. Child Development, 72, 236–252. [DOI] [PubMed] [Google Scholar]
- Shirk SR, Gudmundsen GR, & Burwell RA (2005). Links among attachment-related cognitions and adolescent depressive symptoms. Journal of Clinical Child and Adolescent Psychology, 34, 172–181. [DOI] [PubMed] [Google Scholar]
- Sorce JF, & Emde RN (1981). Mother’s presence is not enough: Effect of emotional availability on infant exploration. Developmental Psychology, 17, 737–745. [Google Scholar]
- Sroufe LA, Egeland B, Carlson EA, & Collins WA (2005). The development of the person: The Minnesota study of risk and adaptation from birth to adulthood. New York: Guilford. [Google Scholar]
- Sylvester CE, Hyde TS, & Reichler RJ (1987). The Diagnostic Interview for Children and Personality Inventory Studies of Children at Risk for Anxiety Disorders or Depression. Journal of American Academy of Child and Adolescent Psychiatry, 26, 668–675. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (1996). Using multivariate statistics. New York: HarperCollins. [Google Scholar]
- Thompson RA (2008). Early attachment and later development: Familiar questions, new answers. In Cassidy J & Shaver PR (Eds.), The handbook of attachment: Theory, research and clinical applications (2nd ed., pp. 348–365). New York: Guilford. [Google Scholar]
- van IJzendoorn MH, Schuengel C, & Bakermans-Kranenburg MJ (1999). Disorganized attachment in early childhood: Meta-analysis of precursors, concomitants, and sequelae. Development and Psychopathology, 11, 225–249. [DOI] [PubMed] [Google Scholar]
- Woodhouse S, Dykas MJ, & Cassidy J (2009). Perceptions of secure base provision within the family. Attachment & Human Development, 11(1), 47–67. [DOI] [PubMed] [Google Scholar]
- Youniss J, & Smollar J (1985). Adolescent relations with mothers, fathers, and friends. Chicago: University of Chicago Press. [Google Scholar]


