Abstract
Background
During the COVID-19 pandemic, pregnant women were identified as a high-risk and vulnerable group. To reduce risk of transmission, maternity healthcare services were modified to limit exposure but maintain services for pregnant women. However, the change in hospital practice may have compromised quality maternal care standards. Therefore, this review aims to explore parental experiences and views with maternity care received from healthcare institutions during the COVID-19 pandemic.
Methods
A mixed studies systematic review was conducted. Six electronic databases (Medline, CINAHL, Embase, PsycInfo, Web of Science, and Maternity and Infant Care) were searched for qualitative, observational, and mixed method studies from the year 2019 to February 2022. Study quality was appraised using the Mixed Methods Appraisal Tool. Quantitative findings were converted to narrative findings. Data was synthesised thematically using a convergent synthesis design.
Results
Fifty-eight articles were included. Four themes were generated: (1) Distress associated with COVID-19 regulations (perception of hospital restrictions, confusion with ever changing policies), (2) adaptability with maternity services (prenatal: changes in birth plans, prenatal: altered antenatal appointments, education, and care, intrapartum: medicalization of birth, postpartum: varied views on care received and Breastfeeding woes, postpartum: skin-to-skin contact and mother infant bonding) (3) importance of support persons, and (4) future direction for maternity services.
Conclusions
Parental experiences highlighted how maternity care during the COVID-19 pandemic did not adhere to WHO standards of quality maternity care. This calls for healthcare institutions to continuously appraise the implementation of restrictive practices that deviate from evidence-based frameworks underpinning quality care.
Keywords: Quality of healthcare, Maternal health services, Mothers, Covid-19, Perinatal care
1. Introduction
On 11th March 2020, the World Health Organisation (WHO) declared Coronaviru-2019 (COVID-19) a pandemic and by April 2021, over three million deaths have been reported to the WHO [1]. Given the aggressive and rapid spread of COVID-19 globally, governments have implemented immediate and drastic measures to curb the rising infections, but this has caused widespread panic and concern amongst the population, particularly vulnerable population groups [2], [3]. In the early stages of the pandemic, pregnant women were identified as one of the high-risk and vulnerable subgroups due to natural physiological changes that occur during pregnancy which increases their risk of infection and developing more severe forms of pneumonia [4], [5], [6]. With the added risk of vertical transmission in newborns [7], maternity healthcare services were modified to limit exposure but maintain services for pregnant women.
Maternity care refers to all care that is related to pregnancy, birth and the postpartum period [8]. The WHO has identified respectful maternity care as a central tenet to high-quality perinatal care, in which healthcare must be safe, effective, timely, efficient, equitable and people-centred [9]. To improve the quality of maternal and newborn care in health facilities, the WHO developed eight standards of quality care which include: (1) implementation of evidence-based practices for routine care and management of complications, (2) having actionable information systems, (3) having functional referral systems, (4) ensuring effective communication, (5) showing respect and preservation of dignity, (6) providing emotional support, (7) having competent, motivated human resources, and (8) making essential physical resources available [9]. Yet, in response to the COVID-19 pandemic, health system policies have deemphasised many aspects of high-quality maternity care including respect, dignity, informed choice, early skin-to-skin contact with the newborn, and continuous support during labour [10], [11].
Although many reviews, guidelines and recommendations related to maternity care during COVID-19 have been published by various organisations [5], [12], [13], to the authors’ knowledge, no systematic review has examined parental perceptions and birth experience related to the changes in maternity care services during the COVID-19 pandemic. Existing reviews were either scoping reviews or limited to examining the effect of these pandemics on maternal and foetal clinical and psychological outcomes [14], [15], [16], [17], [18], [19], [20] or the risk of transmission from mother to neonate [21], [22], [23], [24].
Since pregnancy in a pandemic-free context is already stressful with high levels of depression and anxiety in some cases [25], it is crucial to examine the impacts of modified maternity services on the perinatal experiences of parents in a pandemic. This would provide a better insight into their needs and improve the quality of care. Therefore, this systematic review aims to explore the experiences and views of parents concerning maternity care received from healthcare institutions during the COVID-19 pandemic.
2. Methods
2.1. Study design
A mixed studies systematic review was conducted using Pluye and Hong’s framework [26] to consolidate both quantitative and qualitative data on parents’ experiences with maternity care during the COVID-19 pandemic. A mixed studies approach can facilitate a holistic and better understanding of the phenomenon by synthesising deductive and inductive evidence from studies with diverse designs, which is appropriate for this review. The seven stages of Pluye and Hong’s framework are (i) formulate a research question, (ii) define eligibility criteria, (iii) apply an extensive search strategy, (iv) identify potentially relevant studies, (v) study selection, (vi) study quality appraisal, (vii) synthesize included studies [26].
This review is guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [27]. No protocol was registered. As this is a systematic review, ethics approval and participant informed consent were not sought.
2.2. Research question
The research question is, what does existing qualitative and quantitative evidence inform us about parents’ experiences and views with changes in maternity care practices during the COVID-19 pandemic?
2.3. Search strategy
A systematic search was conducted in six electronic databases (Medline, CINAHL, Embase, PsycInfo, Web of Science, and Maternity and Infant Care) from January 2019 (when COVID-19 first appeared) to February 2022. The search strategy was developed by the research team and verified by an experienced librarian (GS). The search strategy comprised of keywords based on seven concepts related to COVID-19, pregnancy, birth processes, and postpartum maternity care that were most likely affected by COVID-19 restrictions: COVID-19 AND (analgesia OR instrumental delivery OR caesarean section OR birth partner separation OR mother/partner separation from child OR NICU OR breastfeeding). The detailed search strategy can be found in Supplementary material table 1. The reference lists of included studies were also examined for potentially relevant articles.
2.4. Study selection and eligibility
Due to logistical limitations (i.e. limited access to a reliable translator), only English language studies were included in the review. A study is included if: (i) it is a primary study with a qualitative (any study design), quantitative (observational, non-experimental, cross-sectional) or mixed methodology, and (ii) it examines mothers’ birth experience or mothers and support partners’ encounter with maternity care services during COVID-19, or (iii) it examines parental and infant psychosocial outcomes due to hospital COVID-19 restrictions. Mothers and support partners are included regardless of their COVID-19 infection status. As the present review aimed to obtain a holistic understanding of parents’ experiences with maternity care services, studies that exclusively focus on specific refugee or ethnic minority groups were excluded since they often offer unique perceptions or needs that cannot be generalised to the overall parent population [28]. Opinion papers, correspondence, guidelines, editorial letters, commentaries, case study reports, randomised controlled trials, reviews, conference abstracts, and unpublished papers were excluded.
The EndNote and Covidence applications were used to manage search results, remove duplicates, and facilitate screening. Afterward, the titles and abstracts of all studies were screened using the eligibility criteria to identify potentially relevant studies. Full-text screening was then conducted to determine the inclusion status of these selected studies. The screening process was conducted by two independent reviewers (JL and SS) and disagreements were resolved by having discussions with an independent team member not involved in the screening process.
2.5. Quality appraisal
The quality of the included studies was appraised using the Mixed Methods Appraisal Tool (MMAT) [29]. The MMAT separate studies based on their study type (e.g., qualitative, quantitative descriptive, mixed methods), with five appraisal items mainly evaluating the appropriateness and adequacy of choice of method, sampling, data collection and analysis. The calculation of an overall score is discouraged [29] but the appraisal of each included study is available in Supplementary material table 2. Overall, all the qualitative studies had high ratings on the MMAT, indicating that the studies have good quality. On the other hand, some of the quantitative studies were found to have a higher risk of nonresponse bias, and two studies [30], [31] did not employ a sampling strategy that was suitable for addressing the research question. As quality appraisal was done to enhance the rigour of the review [32], all studies were included regardless of their ratings.
2.6. Data extraction
Key details from the included studies were extracted using a form developed by two independent reviewers. These details included the study author(s), year of publication, country, study design, aim, participants’ characteristics, data collection method, and findings. The two reviewers (SS and EDN) tested the chart on five random studies before conducting discussions to improve the form further. After making minor amendments to the form, it was used to collate information from all included studies narratively. Both primary findings and secondary constructs related to maternity care services were extracted for analysis in this review. Any discrepancies were discussed with a third independent researcher until consensus was met.
2.7. Data synthesis
Due to the heterogeneity of quantitative studies, quantitative data analysis was not attempted, and a narrative synthesis approach was undertaken to summarize the diverse findings in a structured manner [33]. Following a convergent synthesis design for mixed studies review [26], quantitative and mixed methods findings were converted to qualitative findings through thematic synthesis using Thomas and Harden’s [34] three-step approach: inductive coding of the text, development of descriptive themes, and generation of analytical themes. The translation of context [34] between studies as described in the three-step approach was done through line-by-line coding which generated initial codes that are grouped together based on their similarities. New codes were then created to capture the meaning of these groups of codes, creating a tree structure with various layers that were organised using descriptive themes. Reviewers used colour coding schemes to indicate the different themes. As the descriptive themes were still highly similar to the original findings of the included studies, analytical themes had to be developed so that the review’s aims could be addressed. This was done by re-reading and comparing the descriptive themes with original data of included studies and interpreting the data beyond the content of original studies. In doing so, the reviewers could infer more meaningful findings related to the experiences of parents when receiving maternity care during the pandemic. The themes were finalised when a consensus was reached between the two independent reviewers (SS and EDN) after several discussions with a third independent researcher.
3. Results
3.1. Search outcomes
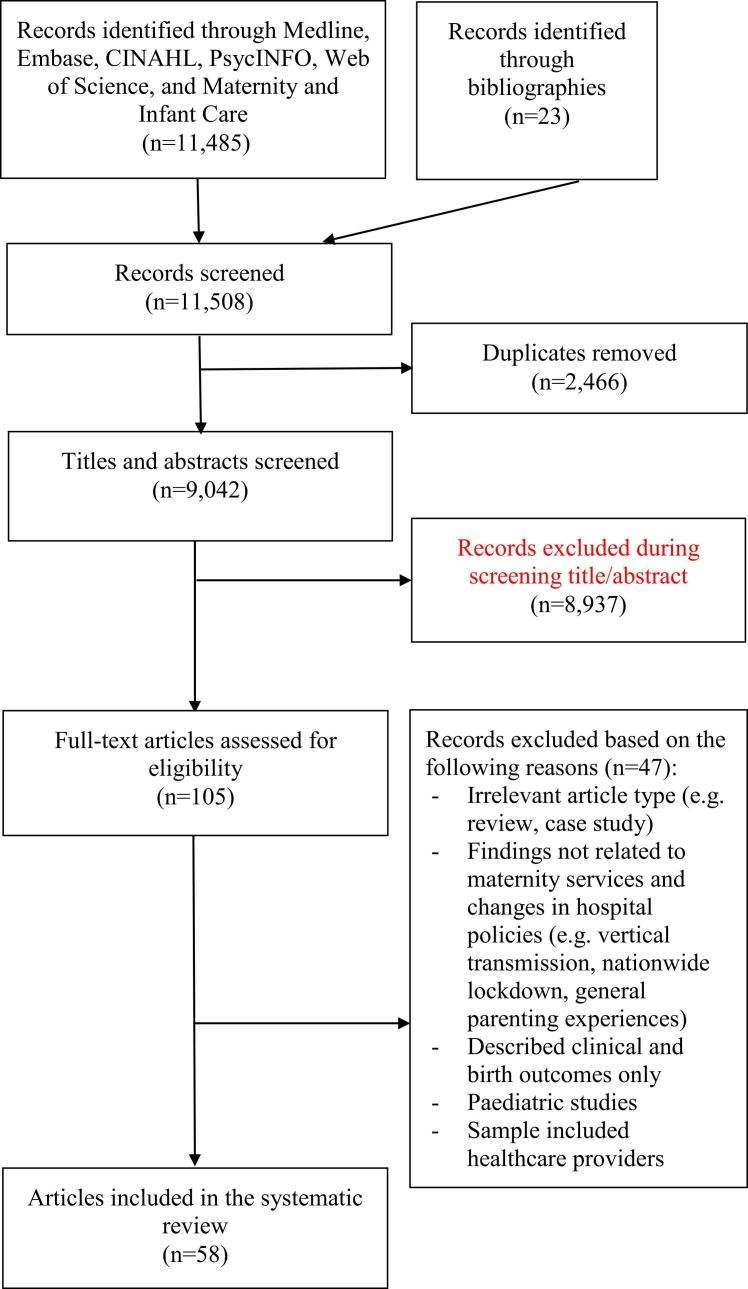
There were 11,485 articles retrieved from the database search. After identifying and removing 2466 duplicates and excluding 8937 articles based on irrelevant titles and abstracts, 105 articles underwent full-text screening to determine their eligibility. Following the screening process, 58 articles were included in this review. The search outcomes are illustrated in the PRISMA flow diagram ( Fig. 1).
Fig. 1.
PRISMA flow diagram.
3.2. Study characteristics
Out of the 58 included studies, 18 were qualitative studies, 31 were quantitative, and nine were mixed-method studies. The majority of the studies were conducted in Europe (n = 23), followed by North America (USA and Canada, n = 17), then Asia (n = 7), and Oceania (Australia, n = 4). Seven were international studies that were conducted across three to 64 countries [30], [35], [36], [37], [38], [39], [40]. This review encapsulates the experiences and views of 107 support partners and 65,543 pregnant and postpartum women who gave birth during the COVID-19 pandemic. Detailed characteristics of the included studies are available in Supplementary material table 3.
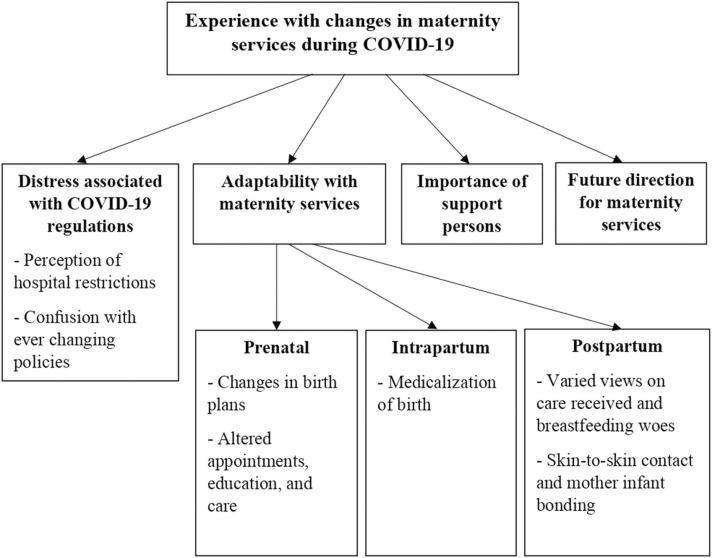
Four themes and five subthemes were identified: (1) Distress associated with COVID-19 regulations, (2) Adaptability with maternity services, (3) Importance of support persons, and (4) Future direction for maternity services. An overview of themes and subthemes is presented in Fig. 2, and representative quotes for each theme are presented in Supplementary material table 4 .
Fig. 2.
Overview of themes and subthemes.
3.3. Distress associated with COVID-19 Regulations
3.3.1. Perception of hospital restrictions
In response to the COVID-19 pandemic, the hospitals adopted various restrictions, which led to mixed responses by pregnant women and new mothers. Healthcare workers had to wear personal protective equipment (PPE) during ward examination and conducting of birth, 22.6 % of mothers felt safer by staff wearing PPE [41], 31.6 % of mothers were indifferent, and 19.2 % felt it made communication more difficult [42]. Others described a colder birthing experience with mask-wearing and distancing as facial expressions of healthcare professionals were hidden [41], [42].
Additionally, mothers (14.5–97 %) were made to wear masks or even PPE during labour, birth, breastfeeding and throughout their hospital stay regardless of their COVID-19 status [35], [43], [44], [45], [46], [47], [48], [49], [50], 13 % of mothers were annoyed by having to wear PPE during labour [35], [48]. Another mother shared how the mask-wearing impaired mother-child bonding, as her newborn was unable to see her face [50]. Other hospital practices reported by mothers that added to their distress included frequent temperature taking, handwashing with soap [42], mandatory COVID-19 testing [47], being restricted to their room and a shorter hospital stay [47].
Another most reported (62–88.4 %) change in hospital care was the restriction of support partners during labour and postpartum visitors [38], [41], [44], [47], [51], [52]. Some mothers were allowed one support person during labour and birth, while some were not allowed any support person [51], however, the majority of the mothers (83–84.4 %) across studies were in agreement with hospital visitation policies [44], [51], [52]. In Sanders and Blaylock’s study [41], 49.9% of mothers felt healthcare workers were too strict with the implementation of visitor arrangements and this sentiment was echoed by partners in Nespoli et al.’s study [53], where some found it unreasonable and lack of compassion.
3.3.2. Confusion with ever changing policies
In Cullen et al.’s study [52], 90.7 % of mothers agreed that the hospital communicated information about visiting restrictions, but 57.5 % of mothers in Sanders and Blaylock’s study [41] found the information provided to be unclear and confusing. Similarly, qualitative studies highlighted how the rapidly changing guidelines, varying hospital protocols, and unclear, inconsistent, conflicting or lack of information received on restrictions resulted in confusion, uncertainty, and anxiety among mothers [35], [40], [41], [43], [44], [52], [54], [55], [56], [57], [58], [59]. In one study [60], fathers were also unsure if they can support their partners given the changing restrictions. Women also mentioned the lack of updates and information from the hospital on the risk of COVID-19 in pregnancy, COVID-19 symptoms and complications, and available health services, hence they had to be proactive in information seeking [40], [43], [52], [54], [55], [56]. According to Estaban-Gonzalo et al.’s study [61], women with higher satisfaction levels with the information provided by healthcare professionals and a greater degree of information about COVID-19 restrictions, symptoms, and complications had a lower state anxiety score, whereas lack of information on restrictive measures was associated with higher state anxiety scores.
In four quantitative survey studies [37], [48], [51], [62], most mothers (40–74 %) mentioned that the COVID-19 pandemic had affected their overall birth experience especially in accessing healthcare services. Restricted access to maternity healthcare services was associated with a higher risk of psychological distress and mental health impairment [62]. In-person appointments were often suspended, rescheduled, or converted to virtual or telemedicine [31], [37], [49]. The suspension of in-person pregnancy-related services led to some mothers giving up on pregnancy care [31], [37], and caused others to feel anxious, neglected, sad, frustrated [37], lonely [30], and fearful of not receiving desired treatment [63]. Altered appointments also reduced birth satisfaction [49] and maternal perception of quality of care [37]. Moreover, approximately 70 % of mothers who changed their birth plan due to COVID-19-related reasons reported experiencing some level of distress [64].
3.4. Adaptability with maternity services
Despite alterations to maternity services, more than half the mothers in Stacey et al.’s [65] and Jafree et al.’s [66] studies reported being satisfied with antenatal appointments (face-to-face and virtual), and intrapartum care, postnatal care, and newborn care. Studies had shown that birth satisfaction is often associated with a myriad of prenatal, intrapartum, and postpartum factors [37], [47], [48], [49], [66], [67], of which parental experiences in these three stages will be further elaborated in the following subthemes.
3.4.1. Prenatal: Changes in birth plans
In most studies, a proportion of mothers (<32 %) considered changing or had changed birth plans or birth location [37], [44], [51], [58], [64], [68]. Mothers’ intention to change or changed birth plans and location were also mentioned in qualitative studies [35], [45], [58], [69]. During the pandemic, mothers were more likely to change from vaginal birth to planned caesarean [64], [70], and change from hospital birth to home birth [41], [55], [64], [68], [70], [71]. In Schroder et al.’s [68] study, reasons cited by mothers for the change to home birth were because they felt less safe in the hospital (20%), felt most safe in their surroundings (81 %), and to avoid COVID-19 infections in the hospital (50 %). These sentiments corresponded with qualitative findings [54], [55].
3.4.2. Prenatal: Altered appointments, education, and care
There were significantly fewer in-person antenatal check-ups and ultrasounds conducted during the COVID-19 pandemic than before COVID-19 [72]. The antenatal appointments were either cancelled, delayed, or replaced with online or virtual classes or telephone appointments. More than half the mothers (51.8–55.1 %) in McMillan [64], Sanders and Blaylock [41] and Burgess [51] studies reported a change to virtual antenatal visits or telephone or video calls. Some mothers praised virtual consultations and telemedicine as time-saving, efficient, and providing access to healthcare professionals [40], [56], [59], [73]. Although 61.4 % of mothers in Burgess’ study [51] were satisfied with virtual care and 86 % reported adequate antenatal care, 93.2 % still preferred face-to-face classes. On the other hand, 73.4 % of mothers in Stampini’s study [74] do not plan to or did not participate in the online birth course. The inadequacy of virtual appointments in meeting parents’ needs was reflected in qualitative findings as well [40], [41], [51], [54], [60], [71], where “a lot of women had fallen through the cracks (missed appointments) during the switch to virtual” [41] and parents were unsure if they were doing the birth exercises correctly [58], [60]. The cancellation of in-person antenatal appointments and education created a sense of loss among parents as it removed a much-needed source of education for parents, especially new parents [40], [43], [44], [51], [56], [59], [60], [75], [76]. Mothers were also concerned about not having physical check-ups to gauge whether their pregnancy was going fine [57], [59], [65], [68], [69], [77] and whether the lack of in-person antenatal classes would affect their childbirth and childcare abilities [44], [68]. In-person antenatal appointments were harder to schedule and reduced in frequency with shorter consultation time and longer intervals, which led to anxiety and nervousness among mothers, especially those with medical complications [40], [41], [44], [51], [57], [59], [69], [71], [73], [78]. A survey by Meaney and colleagues [40] reported that 38.2 % of mothers preferred more antenatal check-ups, and 34.3 % found the interval between appointments to be too long and 35 % would prefer more time with the healthcare professionals. However, 78.1% of mothers were satisfied with the waiting time at hospitals [40]. Mothers shared that hospitals were more peaceful, less crowded, and processes were more streamlined and efficient resulting in shorter waiting times [43], [52], [78]. Additionally, mothers were also disappointed by the decreased options of birth tools (e.g., birthing ball) [79], birth options (e.g., water birth) [44], and pregnancy therapies (e.g. yoga, hydrotherapy, acupuncture) [44], [71] during the pandemic period.
3.4.3. Intrapartum: Medicalization of birth
A regression study by Preis and colleagues [49] discovered that pandemic-related unpreparedness stress was associated with more medicalized birth and greater incongruence with birth preference. Mothers from two studies [38], [58], reported little to no autonomy for the preferred birth position, and no permission was sought by healthcare professionals for instrumental birth and medical interventions. Few mothers reported feeling pressured to have an induction (25.7 %) or the caesarean section (9.5 %) [44]. While some deemed induction and the caesarean section as unnecessary [71], most mothers elected for an earlier induction and operative birth to avoid the rising COVID-19 cases and unpredictability of hospital restrictions [44], [50], [58], [71].
In Liu et al.’s study [70], 13.2 % of mothers reported reduced access to preferred medications (e.g. nitrous oxide and epidural) during birth, and this restriction was found to be associated with increased postnatal depression scores. Limited pain management options (no nitrous oxide) were also mentioned in a qualitative study [71]. In comparison with pre-COVID-19 cohort of mothers, studies did not find any difference in birth mode and use of epidural, but there was a higher rate of induction of labour during COVID [48], [72]. Induction of labour was also associated with reduced maternal satisfaction in the COVID cohort [48]. During the COVID period, more women favoured pharmacological pain relief measures such as epidurals [77], [80] and received pethidine injections [79]. Between mothers who tested positive for COVID and those who tested negative, there was also no difference in the mode of birth [39], [81], [82], induction, and use of epidural [39], [82].
3.4.4. Postpartum: Varied views on care received and breastfeeding woes
In Cullen et al.’s study [52], 94.7 % of mothers reported receiving adequate postpartum support from hospital staff, however, 31.4% of mothers in Lazzerini et al.’s study [38] reported slow response and attention from hospital staff. Due to COVID-19 restrictions, mothers were often confined and isolated in a recovery room where some reported feeling abandoned, overwhelmed, like a prisoner, less aware of what is going on, and received very little attention or slow responses from healthcare professionals [41], [44], [54], [71]. Additionally, with the restriction of postpartum visitors, many mothers were eager to discharge and reunite with their partner and family [55], [83], but others perceived the rushed discharge as negligence and poor quality of care [44], [54], [71]. Moreover, a longer postpartum hospital stay during COVID was associated with higher postpartum depression scores [84].
Qualitative findings also highlighted the absence of postpartum support from healthcare professionals [41], [43], [44], [54], [65], [75], [78], where the lack of follow up doctor appointments for mother and baby and no home visits from health visitors caused mothers to feel abandoned, unsure, and worried as to whether the baby was hitting all the developmental milestones and if they were recovering properly from birth [43], [78]. Although some mothers were appreciative of virtual or telephone postpartum follow up [59], [73], it was found to be still inadequate in assessing mother and child’s physical and mental health [65], [75], [78], [83].
As compared to pre-pandemic, there was a higher rate of breastfeeding within 2 h of birth during the pandemic [72]. While a minority (23 %) of new mothers worried about not being able to breastfeed [30], most mothers (50–94 %) breastfed during their hospital stay [37], [38], [52], [62], [85] of which 48.3–89.3 % reported receiving adequate breastfeeding support. Furthermore, a comparison of breastfeeding rates between COVID positive mothers and COVID negative mothers showed no difference between groups [39], [73], with 57 % [81] to 69 % [46] of COVID positive mothers doing direct breastfeeding during their hospital stay. However, qualitative findings revealed that mothers who were unable to get in-person breastfeeding support or had virtual lactation consultation instead reported more difficulty in breastfeeding [44], [50], [57], [75], [78] with some resorting to a change to formula feeding [43], [45].
3.4.5. Postpartum: Skin-to-skin contact and mother-infant bonding
A higher rate of mother and newborn skin-to-skin contact immediately after birth was reported during the pandemic [72]. Most of the mothers (84.4–90.9 %) had skin-to-skin with their newborn [38], [44], [85] and 80.6–89.2 % were able to room-in with their newborn during their hospital stay [38], [85]. In Ciagran et al.’s study [31], 73.2 % of mothers did not perceive the pandemic restrictions to have affected their relationship with their baby. A small percentage of mothers (3.6–17.7 %) were separated from their babies immediately after birth [67], [70], [85] which is associated with lower birth satisfaction [67] and higher risk of postnatal depression [84].
On the contrary, Donati et al.’s descriptive study [46] which focused on COVID positive mothers, reported a higher rate of mother-infant separation at birth (39 %), a lower rate of skin-to-skin contact (26.6 %) and rooming in with infant (72.1 %), which align with the findings of Bartick and colleagues [36] that compared COVID positive with negative mothers. However, Maholtra [81] and Mayapoulos [39] did not find any difference in the rate of skin-to-skin contact between COVID positive and negative mothers. In Cojocaru’s study [86], most COVID-positive mothers still opted to room in with their newborns and continue with skin-to-skin contact. In contrast, Peng and colleagues [87] reported a longer period of mother-infant separation and lower infant attachment score among COVID positive mothers than COVID negative mothers did. The concerns and difficulty of neonatal separation faced by COVID positive mothers were flagged in qualitative studies, where mothers mentioned a lack of updates on their baby and the fear of infecting their baby [83], [88].
3.5. Importance of support persons
One of the most significant hospital COVID-19 restrictions that affected parents’ birth experience was the restriction of support persons during antenatal appointments and labour, and postpartum visitors [62], [68], [89]. Women’s accounts highlighted their need for partner accompaniment during antenatal appointments, scans, and ultrasounds as some mentioned feeling lonely, overwhelmed by information, stressed, vulnerable, anxious, and fearful that they will be alone if something goes wrong, especially when going for the abnormality scan [40], [41], [43], [52], [54], [56], [59], [65], [90]. These emotions were heightened among first-time mothers and women who had previous complications [41], [52], [54], [56], [58]. Women’s partners also felt worried, empty, disappointed and anxious from being excluded from antenatal appointments. They also mentioned being unfamiliar with the hospital environment and unsure how to support their partners during labour and missing the early connection that mothers have with the newborn baby [53], [60], [76].
During COVID, the absence of a partner in the delivery room was higher than before the pandemic [72], [79] and it was the main cause of worry for some mothers as they feared loneliness during childbirth [32], [60], [71], [74], [77], [86]. In most studies, the majority of mothers (91.9–97.5 %) reported having one support person during birth [48], [67], [74], [85], but only 39 % reported having adequate support during labour [85] and 31% complained that support partner was not allowed to stay beyond labour [48]. Among a sample of COVID positive mothers, only 51.9% had a birth support partner [46]. In Liu’s study [70], 45.8 % of mothers did not have a support person during birth, and another study [49] found lower birth satisfaction in mothers who did not have a birth support partner than those who had. Qualitative findings often reported negative experiences of mothers who did not have a support partner present during labour [30], [36], [39], [45], [46], [61], [66], [68], [87]. Some mothers perceived the absence of a birth partner as a loss of reassurance and advocate [55], [78] while others felt alone, stressed, anxious, and that their mental health was at stake [44], [45], [52], [65]. On the other hand, partners were often left waiting in the car parking lots or at home with limited or no updates from healthcare professionals, which they described the experience as unpleasant, nerve-wrecking, traumatising, lonely, and that negatively impacted their mental health [60], [65], [76]. Partners also mentioned feeling more emotionally detached from the birth experience which impairs their ability to bond with the infant [60], [65], [76].
The restrictions on postpartum hospital visitation received mixed reviews from mothers and their partners. While some needed the continued emotional and physical support from their partners and others were disappointed by the inability to share the joyful moment with family [35], [40], [44], [52], [54], [55], [78], many mothers and their partners appreciated the peace and time to adjust to parenthood, to rest, to bond with their baby [50], [52], [76], and mothers were able to breastfeed comfortably without feeling exposed [52], [78].
3.6. Future directions for maternity services
The most cited area of improvement is the need for healthcare professionals and institutions to be more proactive in providing timely updates and information on COVID-19 risks and changes made to health services, appointments and restrictions [37], [53], [56], [75]. Clearer communication and guidance on birth options were needed from healthcare professionals to better prepare mothers for their hospital stay and relaying updates on birth status or baby’s health was crucial to reduce uncertainty and anxiety in parents [53]. Mothers also requested more personal touch and follow-up on their mental health. Many felt unsupported emotionally and telephone calls were inadequate [41], [56], [65]. A few mothers recommended additional COVID-19 testing for themselves and other family members during the hospital stay and after hospital discharge [88]. Moreover, partners suggested a need for more family-centred practices that encourage and acknowledge partners’ involvement in the pregnancy journey [53], [60].
4. Discussion
This review examined quantitative and qualitative evidence on parents’ experiences and perceptions related to changes in maternity care during the COVID-19 pandemic. Findings described parents’ experience with COVID-19 regulations such as wearing PPE and masking up during the hospital stay, support person and postpartum visit restrictions, and modified perinatal appointments and classes. Parental experiences highlighted how maternity care during the COVID-19 pandemic did not adhere to WHO standards of quality maternity care, specifically in terms of effective communication; respect and preservation of dignity; emotional support; access to competent and motivated human resources [9]. However, it is crucial to note that qualitative findings often emphasise negative parental experiences even though quantitative findings reveal that only a minority group encountered such experiences. This could be that parents were specifically probed to explain and discuss their negative experiences. Future qualitative studies could seek a more balanced approach in probing parents to share both negative and positive experiences around maternity care during the COVID-19 pandemic. Additionally, the majority of the included studies were conducted in high-income countries (HICs) (e.g., Denmark, Italy, Canada and Ireland). Maternity care services in these countries are found to be widely accessible with various facilities to cater to high-risk pregnancies and sufficient staffing to provide close monitoring [91]. On the other hand, maternity care provided in low- and middle-income countries (LMICs) (e.g., Nepal, Pakistan and Mexico) tend to be less accessible. Parents have criticised maternity care facilities in LMICs to have poorly trained staff, providing preferential treatment to certain groups (insurance holders) and lack of facilities [92]. Thus, the experiences of parents with maternity care services may differ significantly depending on the country in which they received the care. However, as the included studies in the present review mainly represented HICs, there was a lack of comparisons between the maternity care experiences of parents in LMICs and HICs and thus the findings may not be generalisable to LMICs.
In the early stage of the pandemic, the limited knowledge of COVID-19 and the rapidly evolving nature of the situation had led to constant changes in hospital regulations and policies, often causing confusion and anxiety among parents. This confusion was exacerbated by the lack of updates and poor adherence to international maternity care guidelines [93], resulting in conflicting information and fluctuating standards of maternity care. Admittedly, healthcare sectors globally were facing immense logistical challenges such as strained manpower and shortage of resources (e.g. PPE) which might have resulted in compromised care [94], [95], [96], [97]. Nonetheless, many mothers in the included studies felt less anxious when they were more satisfied with the information they had received. This was congruent with existing literature on maternity care during COVID-19, where the forwardness and openness of obstetricians in terms of providing information to parents had helped to improve the parents’ experiences during the perinatal period [76]. Thus, to uphold quality maternal care, effective communication between healthcare professionals and women and their families has to be maintained, even more so during a pandemic, where information and care provided should be coordinated, clear and accurate [9]. Providing updated information is vital for informed decision making and it allays feelings of uncertainty, anxiety and fear among mothers, generating a sense of control, autonomy and preparedness for motherhood [98], [99], which may improve maternal outcomes and birth experience.
Another tenet of quality maternal care is the ease of access to competent and motivated healthcare staff for routine care and management of complications. As evident from the review findings, accessibility to prenatal and postpartum maternity care had been greatly impacted (i.e., cancelled, reduced frequency) due to pandemic restrictions. In another study on the impact of COVID-19 on prenatal care, Javaid and colleagues [100] further elaborated some women had to seek a new primary care provider as a result of the restrictions. This was because some doctors, especially those in larger countries where they have different practice locations, tend to travel to different facilities regularly to provide maternity care. As such, when the restrictions require doctors to remain in one maternity care facility, patients residing in other locations were no longer able to receive care from their usual care provider. Some healthcare institutions addressed this by modifying care services into online, virtual or telephone-based consultations and classes. According to the findings of this review, the majority of parents felt satisfied with the virtual care they had received. However, they still preferred to have face-to-face appointments as some parents felt that the virtual care was insufficient in facilitating parents’ learning of hands-on skills and were reported to be inadequate in assessing women and child’s physical condition and health. According to Bandura [101], the key sources to enhance parenting self-efficacy, which is a person’s belief in performing parenting tasks successfully, are enactive mastery, vicarious experience, verbal persuasion, and physiological and emotional states. The shortcomings of virtual, online or phone consultations and classes are their inability to allow parents to model after the healthcare professionals (vicarious experience) and receive real-time coaching and evaluative feedback (verbal persuasion). This might have hindered parents’ development of confidence and perceived self-efficacy in birthing, support, breastfeeding, and infant care skills. Although most parents had a positive experience with virtual care, it is not an ideal replacement for in-person appointments as new parents especially first-time mothers preferred face-to-face consultations.
Based on our findings, women reported that respectful maternity care and preservation of women’s dignity were not upheld as mothers recounted being denied preferred birth choices, pain management, and undergoing unnecessary induction and operative birth. The over medicalisation of normal pregnancy and birth had been found to cause harm to both mother and infant that might further contribute to a culture of abuse and disrespect [102], [103]. Therefore, in recent years, maternal health researchers and professionals have been adopting a more health-promoting salutogenic model of care, which aims to reduce the medicalisation of childbirth [103], [104], [105]. However, progress seems to have regressed during the pandemic as many mothers were electing for medical interventions and operative births for a quicker birth. Although the WHO [99] had previously recommended non-clinical interventions targeted at women and healthcare professionals to reduce unnecessary operative births such as psychoeducation, childbirth workshops, couple-based workshops and medical guidelines, these interventions were not feasible given pandemic restrictions. Hence, more research in the pandemic-context is needed to develop more relevant interventions to reduce adverse women and child outcomes.
The last quality standard that was compromised due to COVID-19 restrictions was the availability of emotional support to women and their family members. Our findings highlighted the restriction of partner accompaniment during prenatal appointments, absence of support partner during labour and even limited visitation of partner and family postpartum. However, the evidence suggests that quality care involves women being given the option to experience labour and childbirth with a companion of their choice and to be given the support that strengthens their capability during childbirth [8]. It has also been well researched that the lack of adequate social support (formal and informal) received by women during the perinatal period can have detrimental effects on their psychological and subjective wellbeing [106], [107], [108], [109], [110]. Poor maternal psychological wellbeing during the perinatal period was especially found to be crucial as it has lifelong ripple effects on partner wellbeing and child development [111], [112]. Therefore, more appraisal and evaluation of flexibility of visitor restrictions are needed [93] in consideration of long term psychosocial impacts on women and the family unit.
4.1. Limitations
The inclusion of quantitative, qualitative, and mixed-method studies in this review provided a broad overview and in-depth insight into parental birth experiences with maternity care during the COVID-19 pandemic. However, the sole inclusion of English papers could have resulted in publication bias, focusing on studies primarily from English-speaking countries (the UK and North America). Unclear titles or abstracts and poor indexing could have missed out on relevant studies. The quality of some quantitative findings was limited as well, due to the uncertainty regarding the sampling strategies and higher risk of nonresponse bias.
Furthermore, the included studies were mainly conducted in HICs limiting the generalisability of the current review’s findings. As such, future quality research is needed to obtain a comparative and deeper understanding of how experiences differ between parents across countries with varying availability of maternity care services.
4.2. Future implications for research and maternity services
There is a paucity of studies from Southeast Asia, the Middle East and Africa, which calls for more research from these regions to facilitate future cultural comparison studies and to provide a holistic view of parental experiences with maternity care during the COVID-19 pandemic. Also, more research is needed on birth partner and healthcare provider perspectives on restrictions and modified care to triangulate the findings and well-rounded views to understand all stakeholder needs. Additionally, more appraisal and evaluation of new services are needed when restrictions and changes in practices deviate from evidence-based frameworks that underpin quality care [93].
Future research can consider triangulating the findings by considering views of healthcare providers to obtain a holistic understanding of how the COVID-19 pandemic has influenced the overall maternity care. While not all experiences with maternity services were negative, most of the studies focused on areas of improvement rather than highlighting the aspects of care that they enjoyed. As such, future research may also specifically consider gathering positive feedback from parents to obtain a more balanced understanding of their experiences with maternity care. Based on parental feedback, healthcare services or professionals should be more diligent in providing consistent, clear, and updated information to better prepare parents. Moreover, healthcare providers should perform follow-up COVID-19 testing for women and their families as a form of reassurance after the hospital discharge. Apart from the need for more mental health support services, healthcare providers should be more empathetic and personal when conducting postpartum follow-ups with mothers. Lastly, healthcare providers should acknowledge, engage and include birth partners during appointments, information sharing, and childbirth to prevent feelings of exclusion and detachment amid partners. Despite being in the midst of a pandemic, healthcare institutions should strive to observe quality maternal care standards specifically in terms of effective communication, respect and preservation of dignity, providing emotional support and access to competent and motivated human resources.
5. Conclusion
This mixed studies systematic review examined parents’ experiences and views with changes in maternity care during the COVID-19 pandemic. Current findings highlight how maternity care during the COVID-19 pandemic did not adhere to WHO standards of quality maternity care which was found to affect mothers’ and partners’ psychological wellbeing. This serves as a call for healthcare institutions and professionals to be more mindful in their appraisal and implementation of restrictive practices that deviate from evidence-based frameworks underpinning quality care.
CRediT authorship contribution statement
Joan Gabrielle Lalor: Conceptualization, Investigation, Writing - Review & Editing. Greg Sheaf: Resources, Investigation, Writing - Review & Editing. Andrea Mulligan: Writing - Review & Editing. Magdalena Ohaja: Writing - Review & Editing. Ashamole Clive: Writing - Review & Editing. Sylvia Murphy-Tighe: Investigation, Writing - Review & Editing. Esperanza Debby Ng: Methodology, Formal analysis, Investigation, writing of manuscript draft, Writing - Review & Editing. Shefaly Shorey: Methodology, Formal analysis, Investigation, Writing - Review & Editing.
Funding
No external funding.
Conflict of interest
None.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.wombi.2022.08.004.
Appendix A. Supplementary material
Supplementary material
.
References
- 1.WHO. WHO Coronavirus (COVID-19) Dashboard. 〈https://covid19.who.int/〉.
- 2.Li Q., Guan X., Wu P., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iyer M., Jayaramayya K., Subramaniam M.D., et al. COVID-19: an update on diagnostic and therapeutic approaches. BMB Rep. 2020;53(4):191. doi: 10.5483/BMBRep.2020.53.4.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Y.-H., Keller J., Wang I.-T., Lin C.-C., Lin H.-C. Pneumonia and pregnancy outcomes: a nationwide population-based study. Am. J. Obstet. Gynecol. 2012;207(4):288. e1–288. e7. doi: 10.1016/j.ajog.2012.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poon L.C. ISUOG Interim Guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. 2020; [DOI] [PMC free article] [PubMed]
- 6.Dashraath P., Wong J.L.J., Lim M.X.K., et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020;222(6):521–531. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tolu L.B., Ezeh A., Feyissa G.T. Vertical transmission of severe acute respiratory syndrome coronavirus 2: a scoping review. PLOS One. 2021;16(4) doi: 10.1371/journal.pone.0250196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiegers T.A. The quality of maternity care services as experienced by women in the Netherlands. BMC Pregnancy Childbirth. 2009;9(1):18. doi: 10.1186/1471-2393-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. Standards for improving quality of maternal and newborn care in health facilities. 〈https://www.who.int/publications/i/item/9789241511216〉.
- 10.Reingold R.B., Barbosa I., Mishori R. Respectful maternity care in the context of COVID‐19: a human rights perspective. Int. J. Gynaecol. Obstet. 2020;151(3):319. doi: 10.1002/ijgo.13376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sadler M., Leiva G., Olza I. COVID-19 as a risk factor for obstetric violence. Sex. Reprod. Health Matters. 2020;28(1) doi: 10.1080/26410397.2020.1785379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pavlidis P., Eddy K., Phung L., et al. Clinical guidelines for caring for women with COVID-19 during pregnancy, childbirth and the immediate postpartum period. Women Birth. 2021;34(5):455–464. doi: 10.1016/j.wombi.2020.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiLorenzo M.A., O’Connor S.K., Ezekwesili C., et al. COVID‐19 guidelines for pregnant women and new mothers: a systematic evidence review. Int. J. Gynaecol. Obstet. 2021;153(3):373. doi: 10.1002/ijgo.13668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iyengar U., Jaiprakash B., Haitsuka H., Kim S. One year into the pandemic: a systematic review of perinatal mental health outcomes during COVID-19. Front. Psychiatry. 2021:845. doi: 10.3389/fpsyt.2021.674194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kotlar B., Gerson E., Petrillo S., Langer A., Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod. Health. 2021;18(1):1–39. doi: 10.1186/s12978-021-01070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banaei M., Ghasemi V., Naz M.S.G., et al. Obstetrics and neonatal outcomes in pregnant women with COVID-19: a systematic review. Iran. J. Public Health. 2020;49(Suppl 1):38. doi: 10.18502/ijph.v49iS1.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Della Gatta A.N., Rizzo R., Pilu G., Simonazzi G. Coronavirus disease 2019 during pregnancy: a systematic review of reported cases. Am. J. Obstet. Gynecol. 2020;223(1):36–41. doi: 10.1016/j.ajog.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elshafeey F., Magdi R., Hindi N., et al. A systematic scoping review of COVID‐19 during pregnancy and childbirth. Int. J. Gynecol. Obstet. 2020;150(1):47–52. doi: 10.1002/ijgo.13182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Juan J., Gil M.M., Rong Z., Zhang Y., Yang H., Poon L.C. Effect of coronavirus disease 2019 (COVID‐19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstet. Gynecol. 2020;56(1):15–27. doi: 10.1002/uog.22088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith V., Seo D., Warty R., et al. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PLOS One. 2020;15(6) doi: 10.1371/journal.pone.0234187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gordon M., Kagalwala T., Rezk K., Rawlingson C., Ahmed M.I., Guleri A. Rapid systematic review of neonatal COVID-19 including a case of presumed vertical transmission. BMJ Paediatr. Open. 2020;4(1) doi: 10.1136/bmjpo-2020-000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huntley B.J., Huntley E.S., Di Mascio D., Chen T., Berghella V., Chauhan S.P. Rates of maternal and perinatal mortality and vertical transmission in pregnancies complicated by severe acute respiratory syndrome coronavirus 2 (SARS-Co-V-2) infection: a systematic review. Obstet. Gynecol. 2020;136(2):303–312. doi: 10.1097/AOG.0000000000004010. [DOI] [PubMed] [Google Scholar]
- 23.Walker K.F., O'Donoghue K., Grace N., et al. Maternal transmission of SARS‐COV‐2 to the neonate, and possible routes for such transmission: a systematic review and critical analysis. BJOG: Int. J. Obstet. Gynaecol. 2020;127(11):1324–1336. doi: 10.1111/1471-0528.16362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang Z., Liu Y. Vertical transmission of severe acute respiratory syndrome coronavirus 2: a systematic review. Am. J. Perinatol. 2020;37(10):1055–1060. doi: 10.1055/s-0040-1712161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yirmiya K., Yakirevich-Amir N., Preis H., Lotan A., Atzil S., Reuveni I. Women’s depressive symptoms during the COVID-19 pandemic: the role of pregnancy. Int. J. Environ. Res. Public Health. 2021;18(8):4298. doi: 10.3390/ijerph18084298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pluye P., Hong Q.N. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu. Rev. Public Health. 2014;35:29–45. doi: 10.1146/annurev-publhealth-032013-182440. [DOI] [PubMed] [Google Scholar]
- 27.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. (Group* P) [DOI] [PubMed] [Google Scholar]
- 28.Toh R.K.C., Shorey S. Experiences and needs of women from ethnic minorities in maternity healthcare: a qualitative systematic review and meta-aggregation. Women Birth. 2022 doi: 10.1016/j.wombi.2022.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Hong Q.N., Fàbregues S., Bartlett G., et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018;34(4):285–291. [Google Scholar]
- 30.Basu A., Kim H.H., Basaldua R., et al. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLOS One. 2021;16(4) doi: 10.1371/journal.pone.0249780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cigăran R.-G., Botezatu R., Mînecan E.-M., et al. The psychological impact of the COVID-19 pandemic on pregnant women. Multidiscip. Digit. Publ. Inst. 2021:725. doi: 10.3390/healthcare9060725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walsh D., Downe S. Meta‐synthesis method for qualitative research: a literature review. J. Adv. Nurs. 2005;50(2):204–211. doi: 10.1111/j.1365-2648.2005.03380.x. [DOI] [PubMed] [Google Scholar]
- 33.Popay J., Roberts H., Sowden A., et al. Guidance on the conduct of narrative synthesis in systematic reviews. A Prod. ESRC Methods Program. Version. 2006;1(1):b92. [Google Scholar]
- 34.Thomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008;8(1):1–10. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ajayi K.V., Harvey I.S., Panjwani S., Uwak I., Garney W., Page R.L. Narrative analysis of childbearing experiences during the COVID-19 pandemic. MCN Am. J. Matern. Child Nurs. 2021;46(5):284. doi: 10.1097/NMC.0000000000000742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bartick M.C., Valdés V., Giusti A., et al. Maternal and infant outcomes associated with maternity practices related to COVID-19: the COVID mothers study. Breastfeed. Med. 2021;16(3):189–199. doi: 10.1089/bfm.2020.0353. [DOI] [PubMed] [Google Scholar]
- 37.Brislane Á., Larkin F., Jones H., Davenport M.H. Access to and quality of healthcare for pregnant and postpartum women during the COVID-19 pandemic. Front. Glob. Women'S. Health. 2021;2 doi: 10.3389/fgwh.2021.628625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lazzerini M., Covi B., Mariani I., et al. Quality of facility-based maternal and newborn care around the time of childbirth during the COVID-19 pandemic: online survey investigating maternal perspectives in 12 countries of the WHO European Region. Lancet Reg. Health-Eur. 2022;13 doi: 10.1016/j.lanepe.2021.100268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mayopoulos G., Ein-Dor T., Li K., Chan S., Dekel S. Giving birth under hospital visitor restrictions: heightened acute stress in childbirth in COVID-19 positive women. Res. Sq. 2020 [Google Scholar]
- 40.Meaney S., Leitao S., Olander E.K., Pope J., Matvienko-Sikar K. The impact of COVID-19 on pregnant womens’ experiences and perceptions of antenatal maternity care, social support, and stress-reduction strategies. Women Birth. 2022;35(3):307–316. doi: 10.1016/j.wombi.2021.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanders J., Blaylock R. “Anxious and traumatised”: users’ experiences of maternity care in the UK during the COVID-19 pandemic. Midwifery. 2021;102 doi: 10.1016/j.midw.2021.103069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adhikari S., Pariyar J., Sapkota K., Gurung T., Adhikari S. Evaluation of knowledge, attitude, practice and hospital experience regarding COVID-19 among post-partum mothers at a tertiary care center: a cross-sectional study. Kathmandu Univ. Med. J. 2020;18(2):10–14. [PubMed] [Google Scholar]
- 43.Riley V., Ellis N., Mackay L., Taylor J. The impact of COVID-19 restrictions on women's pregnancy and postpartum experience in England: a qualitative exploration. Midwifery. 2021;101 doi: 10.1016/j.midw.2021.103061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Breman R.B., Neerland C., Bradley D., Burgess A., Barr E., Burcher P. Giving birth during the COVID‐19 pandemic, perspectives from a sample of the United States birthing persons during the first wave: March‐June 2020. Birth. 2021;48(4):524–533. doi: 10.1111/birt.12559. [DOI] [PubMed] [Google Scholar]
- 45.Rice K., Williams S. Women’s postpartum experiences in Canada during the COVID-19 pandemic: a qualitative study. Can. Med. Assoc. Open Access J. 2021;9(2):E556–E562. doi: 10.9778/cmajo.20210008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Donati S., Corsi E., Salvatore M.A., et al. Childbirth care among SARS-CoV-2 positive women in Italy. Int. J. Environ. Res. Public Health. 2021;18(8):4244. doi: 10.3390/ijerph18084244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Basile Ibrahim B., Kennedy H.P., Combellick J. Experiences of quality perinatal care during the US COVID‐19 pandemic. J. Midwifery Women'S. Health. 2021;66(5):579–588. doi: 10.1111/jmwh.13269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Inversetti A., Fumagalli S., Nespoli A., et al. Childbirth experience and practice changing during COVID‐19 pandemic: a cross‐sectional study. Nurs. Open. 2021;8(6):3627–3634. doi: 10.1002/nop2.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Preis H., Mahaffey B., Heiselman C., Lobel M. The impacts of the COVID-19 pandemic on birth satisfaction in a prospective cohort of 2,341 US women. Women Birth. 2021 doi: 10.1016/j.wombi.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shuman C.J., Morgan M.E., Chiangong J., et al. “Mourning the experience of what should have been”: experiences of peripartum women during the COVID-19 pandemic. Matern. Child Health J. 2022;26(1):102–109. doi: 10.1007/s10995-021-03344-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Burgess A., Breman R.B., Bradley D., Dada S., Burcher P. Pregnant women's reports of the impact of COVID-19 on pregnancy, prenatal care, and infant feeding plans. MCN: Am. J. Matern. /Child Nurs. 2021;46(1):21–29. doi: 10.1097/NMC.0000000000000673. [DOI] [PubMed] [Google Scholar]
- 52.Cullen S., Doherty J., Brosnan M. Women's views on the visiting restrictions during COVID-19 in an Irish maternity hospital. Br. J. Midwifery. 2021;29(4):216–223. [Google Scholar]
- 53.Nespoli A., Ornaghi S., Borrelli S., Vergani P., Fumagalli S. Lived experiences of the partners of COVID-19 positive childbearing women: a qualitative study. Women Birth. 2022;35(3):289–297. doi: 10.1016/j.wombi.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jackson L., De Pascalis L., Harrold J.A., Fallon V., Silverio S.A. Postpartum women’s experiences of social and healthcare professional support during the COVID-19 pandemic: a recurrent cross-sectional thematic analysis. Women Birth. 2021 doi: 10.1016/j.wombi.2021.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Keating N.E., Dempsey B., Corcoran S., McAuliffe F.M., Lalor J., Higgins M.F. Women’s experience of pregnancy and birth during the COVID-19 pandemic: a qualitative study. Ir. J. Med. Sci. 2021:1–8. doi: 10.1007/s11845-021-02862-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Linden K., Domgren N., Zaigham M., Sengpiel V., Andersson M.E., Wessberg A. Being in the shadow of the unknown—Swedish women’s lived experiences of pregnancy during the COVID-19 pandemic, a phenomenological study. Women Birth. 2021 doi: 10.1016/j.wombi.2021.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sweet L., Wilson A.N., Bradfield Z., et al. Childbearing women’s experiences of the maternity care system in Australia during the first wave of the COVID-19 pandemic. Women Birth. 2022;35(3):223–231. doi: 10.1016/j.wombi.2021.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wilson A.N., Sweet L., Vasilevski V., et al. Australian women's experiences of receiving maternity care during the COVID‐19 pandemic: a cross‐sectional national survey. Birth. 2022;49(1):30–39. doi: 10.1111/birt.12569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Perez A., Panagiotopoulou E., Curtis P., Roberts R. Barriers and facilitators to mood and confidence in pregnancy and early parenthood during COVID-19 in the UK: mixed-methods synthesis survey. BJPsych Open. 2021;7(4) doi: 10.1192/bjo.2021.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Poulos N.S., García M.H., Bouchacourt L., Mackert M., Mandell D.J. Fatherhood during COVID-19: fathers' perspectives on pregnancy and prenatal care. J. Men. 'S. Health. 2022;18(2):40. [Google Scholar]
- 61.Esteban-Gonzalo S., Caballero-Galilea M., González-Pascual J.L., Álvaro-Navidad M., Esteban-Gonzalo L. Anxiety and worries among pregnant women during the COVID-19 pandemic: a multilevel analysis. Int. J. Environ. Res. Public Health. 2021;18(13):6875. doi: 10.3390/ijerph18136875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lambelet V., Ceulemans M., Nordeng H.M.E., et al. Impact of the covid-19 pandemic on swiss pregnant and breastfeeding women-a cross-sectional study covering the first pandemic wave. 2021; [DOI] [PubMed]
- 63.Broberg L., Rom A.L., de Wolff M.G., et al. Psychological well‐being and worries among pregnant women in the first trimester during the early phase of the COVID‐19 pandemic in Denmark compared with a historical group: a hospital‐based cross‐sectional study. Acta Obstet. Gynecol. Scand. 2022;101(2):232–240. doi: 10.1111/aogs.14303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McMillan I.F., Armstrong L.M., Langhinrichsen-Rohling J. Transitioning to parenthood during the pandemic: COVID-19 related stressors and first-time expectant mothers’ mental health. Couple Fam. Psychol.: Res. Pract. 2021;10(3):179. [Google Scholar]
- 65.Stacey T., Darwin Z., Keely A., Smith A., Farmer D., Heighway K. Experiences of maternity care during the COVID-19 pandemic in the North of England. Br. J. Midwifery. 2021;29(9):516–523. [Google Scholar]
- 66.Jafree S.R., Momina A., Muazzam A., Wajid R., Calib G. Factors affecting delivery health service satisfaction of women and fear of COVID− 19: implications for maternal and child health in Pakistan. Matern. Child Health J. 2021;25(6):881–891. doi: 10.1007/s10995-021-03140-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mollard E., Kupzyk K. Birth satisfaction during the early months of the Covid-19 pandemic in the United States. MCN Am. J. Matern. Child Nurs. 2022;47(1):6. doi: 10.1097/NMC.0000000000000777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schrøder K., Stokholm L., Rubin K.H., et al. Concerns about transmission, changed services and place of birth in the early COVID-19 pandemic: a national survey among Danish pregnant women. The COVIDPregDK study. BMC Pregnancy Childbirth. 2021;21(1):1–10. doi: 10.1186/s12884-021-04108-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kumari A., Ranjan P., Sharma K.A., et al. Impact of COVID‐19 on psychosocial functioning of peripartum women: a qualitative study comprising focus group discussions and in‐depth interviews. Int. J. Gynecol. Obstet. 2021;152(3):321–327. doi: 10.1002/ijgo.13524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu C.H., Koire A., Erdei C., Mittal L. Unexpected changes in birth experiences during the COVID-19 pandemic: implications for maternal mental health. Arch. Gynecol. Obstet. 2021:1–11. doi: 10.1007/s00404-021-06310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rice K.F., Williams S.A. Making good care essential: the impact of increased obstetric interventions and decreased services during the COVID-19 pandemic. Women Birth. 2021 doi: 10.1016/j.wombi.2021.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cesano N., D’Ambrosi F., Cetera G.E., et al. Maternity ward management and COVID-19 pandemic: experience of a single center in Northern Italy during lockdown. Eur. J. Midwifery. 2021;5 doi: 10.18332/ejm/137605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Malik M., Prescott K., Khalid M., Hashmi A., Kiani A. Expectations and experiences of women regarding maternal healthcare services in Pakistan: challenges and lessons to be learnt. J. Pharm. Policy Pract. 2021;14(1):1–9. doi: 10.1186/s40545-021-00392-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stampini V., Monzani A., Caristia S., et al. The perception of Italian pregnant women and new mothers about their psychological wellbeing, lifestyle, delivery, and neonatal management experience during the COVID-19 pandemic lockdown: a web-based survey. BMC Pregnancy Childbirth. 2021;21(1):1–12. doi: 10.1186/s12884-021-03904-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kolker S., Biringer A., Bytautas J., Blumenfeld H., Kukan S., Carroll J.C. Pregnant during the COVID-19 pandemic: an exploration of patients’ lived experiences. BMC Pregnancy Childbirth. 2021;21(1):1–13. doi: 10.1186/s12884-021-04337-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vasilevski V., Sweet L., Bradfield Z., et al. Receiving maternity care during the COVID-19 pandemic: Experiences of women’s partners and support persons. Women Birth. 2022;35(3):298–306. doi: 10.1016/j.wombi.2021.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Smorti M., Ponti L., Ionio C., Gallese M., Andreol A., Bonassi L. Becoming a mother during the COVID‐19 national lockdown in Italy: Issues linked to the wellbeing of pregnant women. Int. J. Psychol. 2022;57(1):146–152. doi: 10.1002/ijop.12806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Panda S., O'Malley D., Barry P., Vallejo N., Smith V. Women's views and experiences of maternity care during COVID-19 in Ireland: a qualitative descriptive study. Midwifery. 2021;103 doi: 10.1016/j.midw.2021.103092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hui P., Ma G., Seto M.T., Cheung K. Effect of COVID-19 on delivery plans and postnatal depression scores of pregnant women. Hong. Kong Med. J. 2020;27(2):113–117. doi: 10.12809/hkmj208774. [DOI] [PubMed] [Google Scholar]
- 80.Folch Ayora A., Salas‐Medina P., Collado‐Boira E., Ropero‐Padilla C., Rodriguez‐Arrastia M., Bernat‐Adell M.D. Pregnancy during the COVID‐19 pandemic: a cross‐sectional observational descriptive study. Nurs. Open. 2021;8(6):3016–3023. doi: 10.1002/nop2.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Malhotra Y., Knight C., Patil U.P., et al. Impact of evolving practices on SARS-CoV-2 positive mothers and their newborns in the largest public healthcare system in America. J. Perinatol. 2021;41(5):970–980. doi: 10.1038/s41372-021-01023-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mayopoulos G.A., Ein-Dor T., Li K.G., Chan S.J., Dekel S. COVID-19 positivity associated with traumatic stress response to childbirth and no visitors and infant separation in the hospital. Sci. Rep. 2021;11(1):1–8. doi: 10.1038/s41598-021-92985-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fumagalli S., Ornaghi S., Borrelli S., Vergani P., Nespoli A. The experiences of childbearing women who tested positive to COVID-19 during the pandemic in northern Italy. Women Birth. 2022;35(3):242–253. doi: 10.1016/j.wombi.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gupta M., Agarwal N., Agrawal A.G. Impact of COVID-19 institutional isolation measures on postnatal women in level 3 COVID facility in Northern India. J. South Asian Fed. Obstet. Gynaecol. 2021;13(1):51. [Google Scholar]
- 85.Mollard E., Wittmaack A. Experiences of women who gave birth in US hospitals during the COVID-19 pandemic. J. Patient Exp. 2021;8 doi: 10.1177/2374373520981492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cojocaru C., Sundararajan G. An initiative to evaluate the safety of maternal bonding in patients with SARS-CoV-2 infection. J. Matern Neonatal Med [Internet] 2020 30:1–7. doi: 10.1080/14767058.2020.1828335. [DOI] [PubMed] [Google Scholar]
- 87.Peng S., Zhang Y., Liu H., et al. A multi-center survey on the postpartum mental health of mothers and attachment to their neonates during COVID-19 in Hubei Province of China. Ann. Transl. Med. 2021;9(5) doi: 10.21037/atm-20-6115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bender W.R., Srinivas S., Coutifaris P., Acker A., Hirshberg A. The psychological experience of obstetric patients and health care workers after implementation of universal SARS-CoV-2 testing. Am. J. Perinatol. 2020;37(12):1271–1279. doi: 10.1055/s-0040-1715505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Severinsen E.R., Kähler L.K., Thomassen S.E., et al. Mental health indicators in pregnant women compared with women in the general population during the coronavirus disease 2019 pandemic in Denmark. Acta Obstet. Gynecol. Scand. 2021;100(11):2009–2018. doi: 10.1111/aogs.14258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sweet L., Bradfield Z., Vasilevski V., et al. Becoming a mother in the ‘new’social world in Australia during the first wave of the COVID-19 pandemic. Midwifery. 2021;98 doi: 10.1016/j.midw.2021.102996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shaw D., Guise J.-M., Shah N., et al. Drivers of maternity care in high-income countries: can health systems support woman-centred care? Lancet. 2016;388(10057):2282–2295. doi: 10.1016/S0140-6736(16)31527-6. [DOI] [PubMed] [Google Scholar]
- 92.Finlayson K., Downe S. Why do women not use antenatal services in low-and middle-income countries? A meta-synthesis of qualitative studies. PLOS Med. 2013;10(1) doi: 10.1371/journal.pmed.1001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lalor J., Ayers S., Celleja Agius J., et al. Balancing restrictions and access to maternity care for women and birthing partners during the COVID‐19 pandemic: the psychosocial impact of suboptimal care. BJOG: Int. J. Obstet. Gynaecol. 2021;128(11):1720–1725. doi: 10.1111/1471-0528.16844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Asefa A., Semaan A., Delvaux T., et al. The impact of COVID-19 on the provision of respectful maternity care: findings from a global survey of health workers. Women Birth. 2021 doi: 10.1016/j.wombi.2021.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cohen J., van der Meulen Rodgers Y. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev. Med. 2020;141 doi: 10.1016/j.ypmed.2020.106263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.McMahon D.E., Peters G.A., Ivers L.C., Freeman E.E. Global resource shortages during COVID-19: Bad news for low-income countries. PLOS Negl. Trop. Dis. 2020;14(7) doi: 10.1371/journal.pntd.0008412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Schmitt N., Mattern E., Cignacco E., et al. Effects of the Covid-19 pandemic on maternity staff in 2020–a scoping review. BMC Health Serv. Res. 2021;21(1):1–25. doi: 10.1186/s12913-021-07377-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yuill C., McCourt C., Cheyne H., Leister N. Women’s experiences of decision-making and informed choice about pregnancy and birth care: a systematic review and meta-synthesis of qualitative research. BMC Pregnancy Childbirth. 2020;20(1):1–21. doi: 10.1186/s12884-020-03023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Organization W.H. World Health Organization,; 2018. WHO Recommendations Non-clinical Interventions to Reduce Unnecessary Caesarean Sections. [PubMed] [Google Scholar]
- 100.Javaid S., Barringer S., Compton S.D., Kaselitz E., Muzik M., Moyer C.A. The impact of COVID-19 on prenatal care in the United States: Qualitative analysis from a survey of 2519 pregnant women. Midwifery. 2021;98 doi: 10.1016/j.midw.2021.102991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84(2):191. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 102.McDougall L. Maternal health: an executive summary for the Lancet's series-2016. Lancet. 2016 [Google Scholar]
- 103.Perez-Botella M., Downe S., Magistretti C.M., Lindstrom B., Berg M. The use of salutogenesis theory in empirical studies of maternity care for healthy mothers and babies. Sex. Reprod. Healthc. 2015;6(1):33–39. doi: 10.1016/j.srhc.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 104.Heinonen K. Strengthening antenatal care towards a salutogenic approach: a meta-ethnography. Int. J. Environ. Res. Public Health. 2021;18(10):5168. doi: 10.3390/ijerph18105168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shorey S., Ng E.D. Application of the salutogenic theory in the perinatal period: a systematic mixed studies review. Int. J. Nurs. Stud. 2020;101 doi: 10.1016/j.ijnurstu.2019.103398. [DOI] [PubMed] [Google Scholar]
- 106.Antoniou E., Stamoulou P., Tzanoulinou M.-D., Orovou E. Perinatal mental health; the role and the effect of the partner: a systematic review. MDPI. 2021:1572. doi: 10.3390/healthcare9111572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Battulga B., Benjamin M.R., Chen H., Bat-Enkh E. The impact of social support and pregnancy on subjective well-being: a systematic review. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.710858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bedaso A., Adams J., Peng W., Sibbritt D. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod. Health. 2021;18(1):162. doi: 10.1186/s12978-021-01209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Luo Y., Zhang K., Huang M., Qiu C. Risk factors for depression and anxiety in pregnant women during the COVID-19 pandemic: Evidence from meta-analysis. PLOS One. 2022;17(3) doi: 10.1371/journal.pone.0265021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yamada A., Isumi A., Fujiwara T. Association between lack of social support from partner or others and postpartum depression among Japanese mothers: a population-based cross-sectional study. Int. J. Environ. Res. Public Health. 2020;17(12):4270. doi: 10.3390/ijerph17124270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Burke L. The impact of maternal depression on familial relationships. Int. Rev. Psychiatry. 2003;15(3):243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- 112.Walker A.L., Peters P.H., de Rooij S.R., et al. The long-term impact of maternal anxiety and depression postpartum and in early childhood on child and paternal mental health at 11–12 years follow-up. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.562237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material