Figure 1.
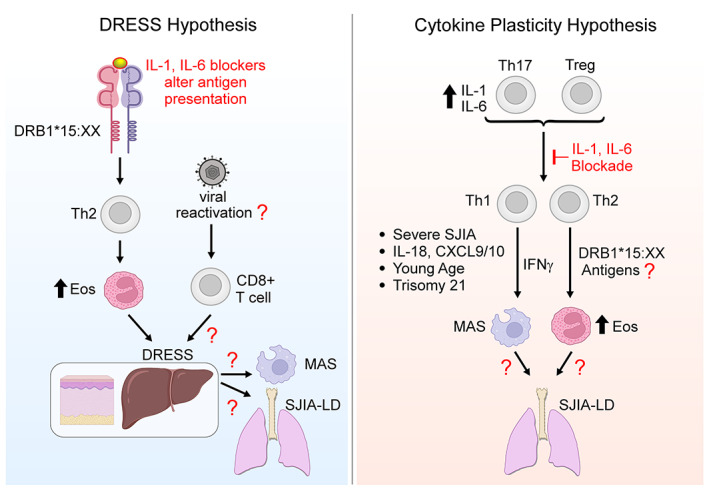
Two hypotheses regarding the relationship between systemic juvenile idiopathic arthritis (SJIA), major histocompatibility complex (MHC) class II, and adverse outcomes after interleukin‐1 (IL‐1) and IL‐6 blockade. In the drug reaction with eosinophilia and systemic symptoms (DRESS) hypothesis, IL‐1 and IL‐6 antagonists alter antigen presentation by MHC class II to CD4+ T cells, leading to Th2‐dominated DRESS. Many DRESS reactions involve herpesvirus reactivation and thus CD8+ T cell activation, factors yet to be studied in systemic JIA. DRESS may then predispose to macrophage activation syndrome (MAS) and/or systemic JIA–associated lung disease (SJIA‐LD) through pathways still to be defined. Under the cytokine plasticity hypothesis, elevated IL‐1 and IL‐6 levels in systemic JIA lead to Th17 skewing in CD4+ Th and Treg cells. Blocking IL‐1 or IL‐6 converts these cells to interferon‐γ (IFNγ)–producing Th1 cells and/or IL‐4–producing Th2 cells, in particular CD4+ T cells recognizing HLA–DRB1*15:XX–presented antigens (exogenous or endogenous). Some patients may undergo analogous transitions without exposure to therapeutics. The resulting clones lead to DRESS‐like reactions and/or SJIA‐LD through pathways still to be defined. Risk factors include severe systemic JIA; increased levels of IL‐18, CXCL9, and CXCL10; young age; and trisomy 21. The critical difference between these hypotheses is the contribution of the IL‐1 and IL‐6 blocking agents. Eos = eosinophils. Created in part using BioRender.
