Abstract
Background
Type 2 diabetes is considered one of the most psychologically demanding chronic conditions. Patients suffering from this disease often have poor psychological well-being due to emotional stress. Baduanjin exercises, a traditional Chinese mind-body exercise, are used in the management of type 2 diabetes, especially for mental health. However, the effect of Baduanjin exercises on psychological well-being of patients with type 2 diabetes maintains controversial. Therefore, this systematic review was conducted to evaluate the effects on psychological well-being of Baduanjin exercises for type 2 diabetes.
Methods
Six electronic databases were searched from their inception to March 2022 for randomized controlled trials of Baduanjin exercises for type 2 diabetes. Two reviewers independently extracted data and assessed methodological quality based on PEDro scale. The subgroup analysis was conducted based on different control interventions. The Cochran Q statistic and I2 were applied to assess the heterogeneity.
Results
Twenty-seven studies between 2005 and 2019 were included in our review. Most of them exceeded the cutoff score 6 based on the PEDro scale. In psychological well-being, the aggregated results indicated that Baduanjin exercises showed positive effects in psychological well-being (SMD, 0.96; 95% CI, 0.57 to 1.36; p < 0.00001), depression (SMD, 1.03; 95% CI, 0.08 to 1.97; p = 0.03), anxiety (SMD, 0.88; 95% CI, 0.30 to 1.46; p = 0.003), and mental health (SMD, 0.72; 95% CI, 0.42 to 1.02; p < 0.00001). In glycemic control, Baduanjin exercises showed better improvements in FBG (SMD, 0.53; 95% CI, 0.34 to 0.72; p < 0.00001), HbA1c (SMD, 0.58; 95% CI, 0.41 to 0.75; p < 0.00001), and 2-hPBG (SMD, 0.56; 95% CI, 0.08 to 1.03; p = 0.02) compared with usual care/education. However, Baduanjin exercises only showed better improvements in HbA1c when compared with other exercises.
Conclusions
The traditional Chinese mind-body exercise-Baduanjin is a beneficial comprehensive therapy for type 2 diabetes, especially in promoting psychological well-being.
Systematic review registration
https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=110034.
Keywords: mind-body exercises, Baduanjin, type 2 diabetes, psychological well-being, mental health
Introduction
The increasing prevalence of type 2 diabetes has become a global public health concern that results in a substantial socioeconomic and healthcare burden (1). In China, the prevalence of diabetes is as high as 10.9% with many people remaining undiagnosed (2). Diabetes can cause health complications such as cardiovascular disease, nephropathy, and retinopathy. Furthermore, diabetes and its complications have a huge impact on the patients' psychological well-being (3). Type 2 diabetes is one of the most psychologically demanding chronic conditions, and patients often have poor psychological well-being due to emotional stress (4). Depression was associated with poorer glycemic control and the management of its complications in patients with type 2 diabetes (5).
Exercise has generally been recommended in the management of diabetes to reduce the risk factors associated with diabetes such as obesity, sedentary lifestyle, and a high fat diet (6). Low-to-moderate daily exercises are recognized to contribute to glycemic control, psychological well-being, and the management of the complications of type 2 diabetes (7). In China, Baduanjin exercises usually are used as the complementary therapy by the patients with type 2 diabetes, which include eight movements: “holding the hands high with palms up to regulate the internal organs,” “posing as an archer shooting both left- and right-handed,” “holding one arm aloft to regulate the functions of the spleen and stomach,” “looking backwards to prevent sickness and strain,” “swinging the head lowering the body to relieve stress,” “moving the hands down the back and legs and touching the feet to strengthen the kidneys,” “thrusting the fists and making the eyes glare to enhance strength,” and “raising and lowering the heels to cure diseases.” Compared with conventional exercises, Baduanjin exercises, as the traditional Chinese mind-body exercises, emphasize breathing regulation, musculoskeletal relaxation, and relaxing mindfulness for maximizing both physical and psychological well-being of patients with chronic illnesses.
The previous review indicated that Baduanjin exercises plus conventional drug treatments have positive effects in glycemic control of the patients with type 2 diabetes (8). However, there was no systematic review focusing on psychological well-being of Baduanjin exercises for type 2 diabetes. Good psychological well-being could contribute to glycemic control. Several studies have shown beneficial effects in improving depression and anxiety of patients with type 2 diabetes (9–12), but the evidence on the effects of Baduanjin exercises in improving psychological well-being of patients with type 2 diabetes is still insufficient.
Therefore, the current systematic review evaluated the effects of traditional Chinese mind-body exercise-Baduanjin for patients with type 2 diabetes. It provided evidence-based information for the clinical application of Baduanjin exercises for type 2 diabetes, especially for improving psychological well-being.
Methods
Trial registration
This systematic review was prospectively registered in PROSPERO with the number CRD42018110034.
Search strategy
The following electronic databases were searched from their inceptions to March 2022: PubMed, EMBASE, Cochrane Library, China Knowledge Resource Integrated Database (CNKI), Weipu Database for Chinese Technical Periodicals, and Wanfang Data Information. The search terms were diabetes, Baduanjin, eight-brocade exercises, eight-treasured exercises, and eight section brocades. The literature was obtained from other sources: the reference lists of the related reviews, unpublished dissertations, and manual searching at the library of Shanghai University of Traditional Chinese Medicine. There were no restrictions on language or publication status.
Study selection
In this review, the eligibility criteria for included studies were: (a) randomized clinical trials (RCTs). (b) participants diagnosed with type 2 diabetes, there were no limitations on age, gender, or nationality. (c) Baduanjin exercises were used as a complementary therapy for type 2 diabetes, and all participants received the conventional drugs of type 2 diabetes. The control interventions included usual care, education, and any complementary and alternative therapies without Baduanjin exercises. (d) the primary outcomes included psychological well-being assessed by the Global well-being schedule (GWB) and WHO-5 well-being index (WHO-5); depression assessed by Hamilton depression scale (HAMD), Montgomery Asberg depression rating scale (MADRS), and Self-rating depression scale (SDS), and anxiety assessed by Hamilton anxiety scale (HAMA), and Self-rating anxiety scale (SAS). The secondary outcomes were fasting blood glucose (FBG), glycosylated hemoglobin (HbA1c), 2-h postprandial blood glucose (2-hPBG), and quality of life assessed by 36-Item short-form health survey (SF-36), Diabetes specific quality of life (DSQL), and European quality of life 5-dimensions (EQ-5D). The selection of studies was independently conducted by two reviewers (JR and SF) with good agreement (k = 0.86, 95% CI 0.54 to 1.00). Any disagreements were discussed by all reviewers.
Data extraction
According to the pre-defined criteria, data extraction was independently performed by two reviewers (LK and XZ) with good agreement (k = 0.847, 95% CI 0.66 to 1.00). The following information was extracted: first author, year, and country; sample size; duration of disease; mean age; main outcomes; interventions of Baduanjin exercises group; and interventions of the control group. Only the first phase data were extracted in the crossover studies. Any discrepancies were discussed by all reviewers.
Quality assessment
Two reviewers (LK and XZ) independently assessed the methodological quality of the included studies using the Physiotherapy Evidence Database (PEDro) scale, which was reported to have a fair to good reliability for RCTs of the physiotherapy in systematic reviews. The PEDro scale includes (a) study eligibility criteria specified, (b) random allocation of subjects, (c) concealed allocation, (d) measure of similarity between groups at baseline, (e) subject blinding, (f) therapist blinding, (g) assessor blinding, (h) <15% dropouts, (i) intention-to-treat analysis, (j) between-group statistical comparisons, and (k) point measures and variability data. The PEDro score was calculated by criteria (b) to (k) according to meeting the criteria or not. The previous studies reported that a cut point of 6 using the PEDro scale indicated high-quality studies (13). Any disagreement was resolved by discussion between the reviewers.
Data synthesis and analysis
The meta-analysis was performed using the Review Manager Version 5.3 software. For continuous data, the changes from baseline were used in the meta-analysis. The standardized mean difference (SMD) and 95% confidence intervals (CIs) were calculated. A random effects model was used for the better clinical heterogeneity. The Cochran Q statistic (considered to be statistically significant when p < 0.10) and I2 (where I2 > 30% indicates moderate heterogeneity; I2 > 50% substantial heterogeneity; and > 75% considerable heterogeneity) were used to assess the heterogeneity. A sensitivity analysis was conducted to explore possible source of heterogeneity when > 75% considerable heterogeneity. The subgroup analysis was conducted based on different control interventions. The risk of publication bias was assessed if more than ten trials were included in the meta-analysis. The p < 0.05 was considered to be statistically significant.
Results
Search and selection
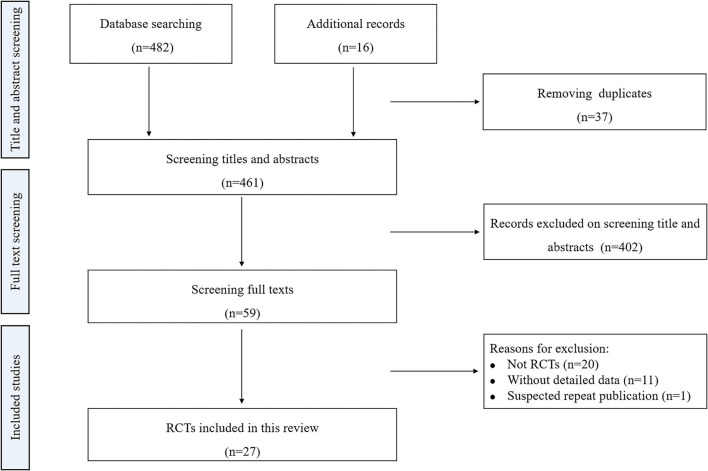
The literature search identified 498 records. After removing duplications, 461 potentially relevant studies were identified. A total of 402 studies were excluded after screening the titles and abstracts. We examined 59 full texts for inclusion in our review. After screening the full texts, 32 studies were excluded. Finally, 27 studies were included in our review (10–12, 14–37). The detailed process is summarized in Figure 1.
Figure 1.
Flow chart for the meta-analysis. RCTs: randomized controlled trials.
Characteristics of the included studies
Twenty-seven studies assessed the effects of Baduanjin exercises, as a complementary therapy, for type 2 diabetes. All studies were conducted in China between 2005 and 2019. A total of 2,048 participants with the mean age of 56.86 ± 6.29 were included in the eligible studies. The diseases duration was 7.53 ± 3.44 years, and control interventions included usual care, education, walking, Tai Chi, and aerobic exercises. The duration of the Baduanjin exercises ranged from 4 to 48 weeks, and almost half of the participants experienced 24 weeks of Banduanjin exercises. The frequency ranged from 2 to 12 sessions per week, and 59% of the studies used 7 sessions per week. The time of each session ranged from 20 to 90 min (43.20 ± 17.77). None assessed the follow-up effect of Baduanjin exercises for type 2 diabetes. The characteristics of the included studies are summarized in Table 1.
Table 1.
Randomized controlled trials assessing the effect of Baduanjin exercises for type 2 diabetes.
| Study | Sample size | Mean age (year) | Duration of disease (year) |
Follow-up (months) |
Main outcomes | Baduanjin group intervention | Control group intervention |
|---|---|---|---|---|---|---|---|
| Zhang et al. (14) | 25 20 |
58.4 ± 8.18 58 ± 7.02 |
10.9 ± 6.84 6.2 ± 6.84 |
— | FBG, HbA1c, SCL-90, SF-36 | Baduanjin (60 min, 3/week, 8 weeks) |
Usual care |
| Wang et al. (15) | 40 39 |
57.8 ± 7.5 56.5 ± 6.9 |
NR | — | FBG, HbA1c | Baduanjin (60 min, 7/week, 24 weeks) |
Usual care |
| Pan et al. (16) | 24 24 |
47 ± 7 45 ± 9 |
2.5 ± 1.1 2.6 ± 0.8 |
— | FBG, HbA1c, BMI, WHR | Baduanjin (45 min, 5/week, 24 weeks) |
Usual care |
| Huang et al. (17) | 30 30 |
57.8 ± 7.5 56.5 ± 6.9 |
3–10 | — | FBG, HbA1c | Baduanjin (60 min, 7/week, 24 weeks) |
Usual care |
| Zhang et al. (10) | 15 15 |
54.9 | NR | — | FBG, HbA1c, 2-hPBG, MARDS, HAMA | Baduanjin (60 min, 7/week, 24 weeks) |
Usual care |
| Zhou et al. (18) | 63 63 |
67.4 ± 9.23 68.13 ± 10.64 |
7.98 ± 1.09 7.87 ± 1.78 |
— | FBG, HbA1c, 2-hPBG, BMI, WHR | Baduanjin (30 min, 7/week, 12 weeks) |
Aerobic exercises (30 min, 3–5/week, 12 weeks) |
| Duan et al. (19) | 100 100 |
45 Saturday, July 9, 2022 11:12 am± 9 47 ± 7 |
2.6 ± 0.8 2.5 ± 1.1 |
— | FBG, HbA1c, BMI, WHR | Baduanjin (20 min, 7/week, 8 weeks) |
Aerobic exercises (30 min, 7/week, 8 weeks) |
| Guan et al. (11) | 40 40 |
59.20 ± 8.80 58.70 ± 8.30 |
3–18 2–17 |
— | FBG, HbA1c, 2-hPBG, SAS, SDS | Baduanjin (60 min, 7/week, 24 weeks) |
Usual care |
| Ji et al. (12) | 32 30 |
60.31 ± 7.23 60.26 ± 7.15 |
NR | — | FBG, HbA1c, 2-hPBG, SAS, SDS, GWB | Baduanjin (45 min, 7/week, 8 weeks) |
Education |
| Liu et al. (20) | 33 36 |
62.64 ± 5.98 65.64 ± 8.38 |
6.85 ± 5.9 8.25 ± 5.94 |
— | HbA1c, SDS, SF-36 | Baduanjin (40 min, 3–5/week, 12 weeks) |
Education (30 min, 1/2 weeks, 12 weeks) |
| Li et al. (21) | 54 54 54 54 |
54.21 ± 9.47 50.42 ± 9.68 51.62 ± 7.83 52.69 ± 8.37 |
6.95 ± 3.63 6.02 ± 3.29 6.31 ± 3.53 7.22 ± 4.14 |
— | FBG, HbA1c, BMI, SF-36 | Baduanjin (30 min, 7/week, 36 weeks) |
• Aerobic exercise (30 min, 7/week, 36 weeks) • Tai Chi (30 min, 7/week, 36 weeks) • Usual care |
| Lin et al. (22) | 19 19 |
64.5 ± 11.5 60.8 ± 12.2 |
2–12 2–9 |
— | FBG, HbA1c | Baduanjin (90 min, 7/week, 24 weeks) |
Usual care |
| Chen et al. (23) | 10 10 10 |
60.00 ± 5.23 63.70 ± 5.40 63.33 ± 7.78 |
NR | — | FBG, HbA1c, 2-hPBG, SF-36 | Baduanjin (5/ week, 24 weeks) |
• Walking (30 min, 14/ week, 24 weeks) • Education |
| Li et al. (24) | 20 20 |
53.6 ± 8.7 51.4 ± 9.2 |
7.6 ± 3.6 7.7 ± 3.9 |
— | FBG, HbA1c, 2-hPBG, PSQI | Baduanjin (30 min, 7/week, 4 weeks) |
Usual care |
| Liu et al. (25) | 20 20 |
57 ± 7 55 ± 9 |
5.5 ± 1.1 5.6 ± 0.8 |
— | HbA1c SAS | Baduanjin (30 min, 5/week, 24 weeks) |
Usual care |
| Ren et al. (26) | 10 9 9 |
60.38 ± 4.81 63.12 ± 7.2 60.38 ± 5.81 |
NR | — | FBG, HbA1c, 2-hPBG, SF-36, BMI, WHR | Baduanjin (5/week, 24 weeks) |
• Walking (30 min, 5/week, 24 weeks) • Education |
| Wei et al. (27) | 20 20 20 |
63.9 ± 7.6 64.8 ± 5.8 65.3 ± 6.0 |
NR | — | SF-36 | Baduanjin (30 min, 5–7/week, 12 weeks) |
• Walking (30 min, 5–7/week, 12 weeks) • Usual care |
| Zhou et al. (28) | 13 12 |
51-72 58-80 |
0.5–25 1–24 |
— | FBG, HbA1c, SDS | Baduanjin (30 min, 7/week, 12 weeks) |
Usual care |
| Peng et al. (29) | 71 70 |
NR | NR | — | FBG, SAS, SCL-90 | Baduanjin (60 min, 7/week, 24 weeks) |
Usual care |
| Sun et al. (30) | 33 32 |
46.1 ± 11.8 | NR | — | FBG, HbA1c, 2-hPBG, SAS, SDS | Baduanjin (60 min, 2/week, 24 weeks) |
Aerobic exercises (60 min, 2/week, 24 weeks) |
| Wang et al. (31) | 30 30 |
61.7 ± 6.9 61.3 ± 8.4 |
10.6 ± 4.1 10.2 ± 3.6 |
— | FBG, HbA1c | Baduanjin (20 min, 5/week, 6 weeks) |
Usual care |
| Zhang et al. (32) | 45 45 18 |
57 ± 2.4 55.4 ± 1.70 58.2 ± 1.00 |
15 ± 0.6 14.5 ± 0.7 14.2 ± 0.5 |
— | FBG, HbA1c | Baduanjin (30 min, 7/week, 100 days) |
• Aerobic exercises (30 min, 7/week, 100 days) • Usual care |
| Yang et al. (33) | 55 55 |
52.40 ± 2.30 50.30 ± 3.40 |
11.20 ± 2.10 10.80 ± 1.90 |
— | HbA1c, HAMD, DSQL | Baduanjin (60 min, 7/week, 12 weeks) |
Education (30 min, 6 sessions, 12 weeks) |
| He et al. (34) | 30 28 30 |
49.63 ± 12.97 52.04 ± 10.60 51.03 ± 11.73 |
4.29 ± 3.96 4.99 ± 4 4.82 ± 4.05 |
— | EQ-5D, WHO-5 | Baduanjin (20–60 min, 3–7/week, 48 weeks) |
• Walking (20-60 min, 3–7/week, 48 weeks) • Education |
| Liu et al. (35) | 45 45 |
45.01 ± 3.14 43.98 ± 2.81 |
3.12 ± 1.51 3.26 ± 0.95 |
— | DSQL | Baduanjin (20 min, 10/week, 12 weeks) |
Usual care |
| Miao et al. (36) | 40 40 |
53.96 ± 5,94 55.56 ± 5.96 |
NR | — | SF-36 | Baduanjin (20 min, 12/week, 12 weeks) |
Usual care |
| Guo et al. (37) | 15 15 |
57.77 ± 6.89 57.53 ± 6.14 |
10.27 ± 7.63 11.60 ± 6.24 |
— | FBG, HbA1c, 2-hPBG, BMI, SDSCA | Baduanjin (40–60 min, 4/week, 12 weeks) |
Usual care |
BMI, Body mass index; FBG, Fasting blood glucose; DSQL, Diabetes specific quality of life; EQ-5D, European quality of life 5-dimensions; GWB, Globle well-being schedule; HAMA, Hamilton anxiety scale; HAMD, Hamilton depression scale; HbA1c, Gglycosylated haemoglobin; 2-hPBG, 2-h postprandial blood glucose; MADRS, Montgomery asberg depression rating scale; NR, Not reported; PSQI, Pittsburgh sleep quality index; SAS, Self-rating anxiety scale; SDS, Self-rating depression scale; SDSCA, Summary of diabetes self care activities; SCL-90, Symptom checklist 90; SF-36, 36-Item short form health survey; WHO-5, WHO-5 well-being index.
Methodological quality
Most studies (89%) of Baduanjin exercises for type 2 diabetes exceeded the PEDro cutoff score of 6. The greatest potential bias was associated with blinding and concealed allocation. Only two studies performed assessor blinding (11, 29) and five studies did not use the intention-to-treat analysis (11, 26, 32, 33, 37). Other items were scored positive in the included studies. The detailed scores were shown in Table 2.
Table 2.
PEDro scale of quality for the included trials.
| Study | Eligibility criteria | Random allocation | Concealed allocation | Similar at baseline | Subjects blinded | Therapists blinded | Assessors blinded | <15% dropouts | Intention-to-treat analysis | Between-group comparisons | Point measures and variability data | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhang et al. (14) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Wang et al. (15) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Pan et al. (16) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Huang et al. (17) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Zhang et al. (10) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Zhou et al. (18) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Duan et al. (19) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Guan et al. (11) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Ji et al. (12) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Liu et al. (20) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Li et al. (21) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Lin et al. (22) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Chen et al. (23) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Li et al. (24) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Liu et al. (25) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Ren et al. (26) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Wei et al. (27) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Zhou et al. (28) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Peng et al. (29) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Sun et al. (30) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Wang et al. (31) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Zhang et al. (32) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Yang et al. (33) | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 |
| He et al. (34) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Liu et al. (35) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Miao et al. (36) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Guo et al. (37) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
Criteria (2–11) were used to calculate the total PEDro score. Each criterion was scored as either 1 or 0 according to whether the criteria was met or not, respectively.
Synthesis of the results
Psychological well-being
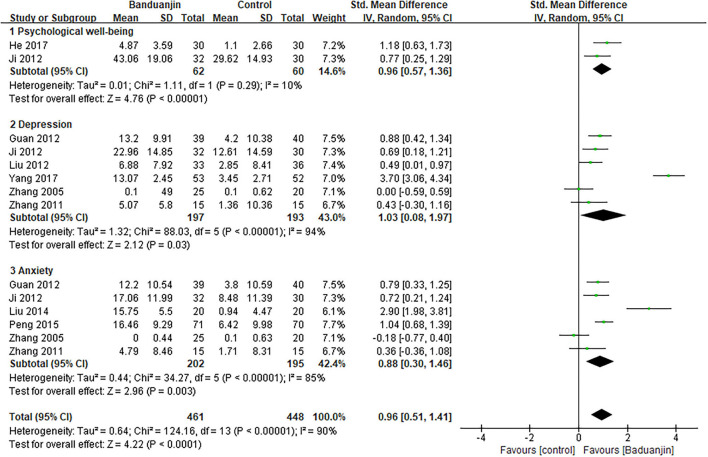
The aggregated result in the meta-analysis showed that Baduanjin exercises significantly improved the psychological well-being of patients with type 2 diabetes (SMD, 0.96; 95% CI, 0.51 to 1.41; p < 0.0001, Figure 2). In the subgroup analysis, the aggregated results indicated that Baduanjin exercises showed better improvements in psychological well-being (SMD, 0.96; 95% CI, 0.57 to 1.36; p < 0.00001, Figure 2), depression (SMD, 1.03; 95% CI, 0.08 to 1.97; p = 0.03, Figure 2) and anxiety (SMD, 0.88; 95% CI, 0.30 to 1.46; p = 0.003, Figure 2) compared with usual care/education. Sun also reported that 6 months of Baduanjin exercise showed better improvements in depression and anxiety in patients with type 2 diabetes compared with aerobic exercises (30). Sensitivity analyses yielded similar and non-significant differences for the above-mentioned outcomes.
Figure 2.
Forest plot of the effects of Baduanjin exercises on psychological well-being.
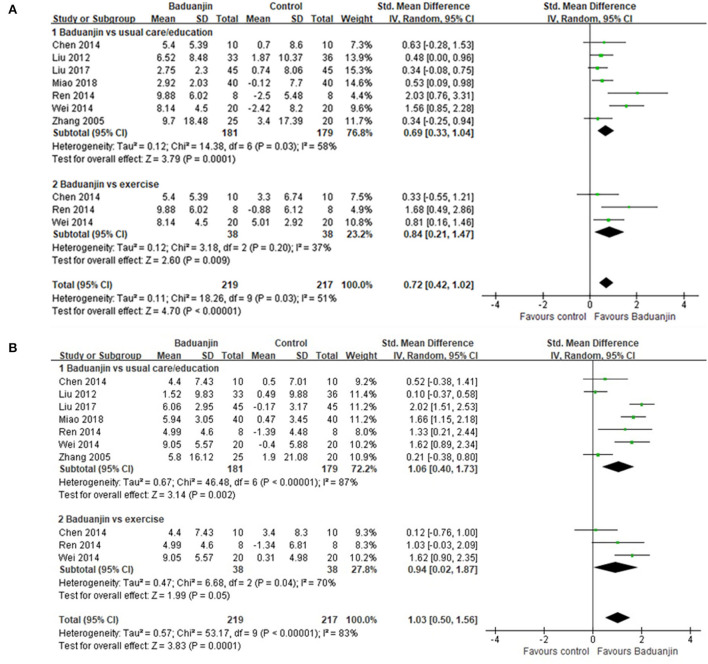
Quality of life
In mental component scores, the aggregated result demonstrated that Baduanjin exercises also significantly improved mental health of the patients with type 2 diabetes (SMD, 0.72; 95% CI, 0.42 to 1.02; p < 0.00001, Figure 3A). In the subgroup analysis, Baduanjin exercises showed better improvements in mental health compared with usual care/education (SMD, 0.69; 95% CI, 0.33 to 1.04; p = 0.0001, Figure 3A) and other exercises (SMD, 0.84; 95% CI, 0.21 to 1.47; p = 0.009, Figure 3A). In physical component scores, Baduanjin exercises showed better improvements in physical health compared with usual care/education (SMD, 1.06; 95% CI, 0.40 to 1.73; p = 0.002, Figure 3B), but not compared with other exercises (SMD, 0.94; 95% CI, 0.02 to 1.87; p = 0.05, Figure 3B). Sensitivity analyses yielded similar and non-significant differences for the above-mentioned outcomes.
Figure 3.
Forest plot of the effects of Baduanjin exercises on quality of life. (A) mental component scores, (B) physical component scores.
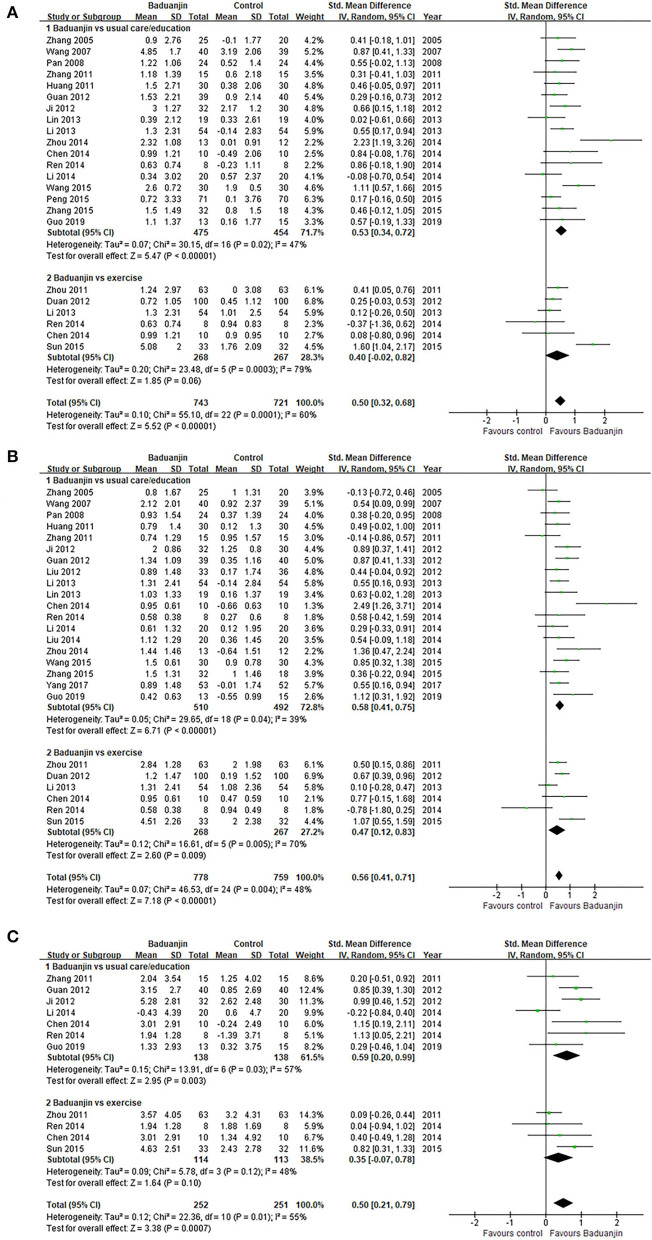
Glycemic control
Compared with usual care/education, Baduanjin exercises showed better improvements in FBG (SMD, 0.53; 95% CI, 0.34 to 0.72; p < 0.00001, Figure 4A), HbA1c (SMD, 0.58; 95% CI, 0.41 to 0.75; p < 0.00001, Figure 4B), and 2-hPBG (SMD, 0.59; 95% CI, 0.20 to 0.99; p = 0.003, Figure 4C). However, the aggregated result indicated that the Baduanjin exercises only showed better improvements in HbA1c (SMD, 0.47; 95% CI, 0.12 to 0.83; p = 0.009, Figure 4B) compared with other exercises. Baduanjin exercises did not get better gains in FBG (SMD, 0.40; 95% CI, −0.02 to 0.82; p = 0.06, Figure 4A) or 2-hPBG (SMD, 0.35; 95% CI, −0.07 to 0.78; p = 0.10, Figure 4C) compared with other exercises. Sensitivity analyses yielded similar and non-significant differences for the above-mentioned outcomes.
Figure 4.
Forest plot of the effects of Baduanjin exercises on Glycemic control. (A) fasting blood glucose, (B) glycosylated hemoglobin, (C) 2-h postprandial blood glucose.
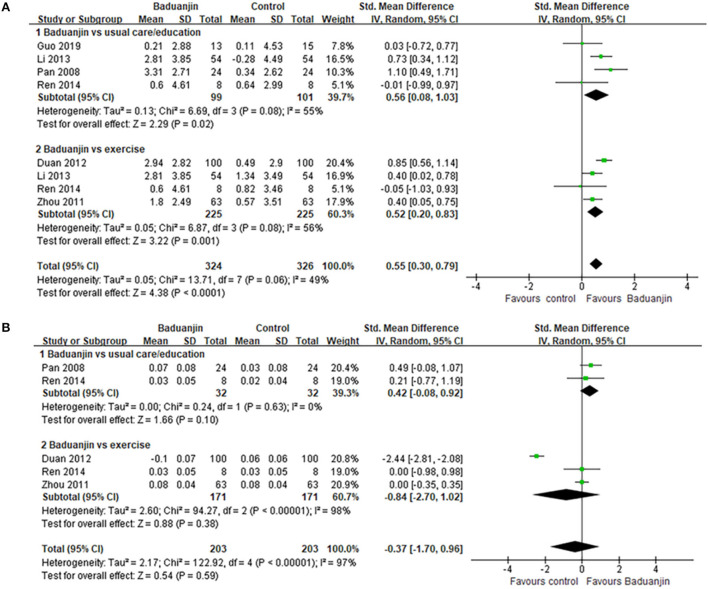
Body fat control
The aggregated result also showed that Baduanjin exercises got better gains on body mass index compared with usual care/education (SMD, 0.56; 95% CI, 0.08 to 1.03; p = 0.02, Figure 5A) and other exercises (SMD, 0.52; 95% CI, 0.20 to 0.83; p = 0.001, Figure 5A). However, Baduanjin exercises did not show better improvements in wait–hip ratio of patients compared with usual care/education (SMD, 0.42; 95% CI, −0.08 to 0.92; p = 0.10, Figure 5B) or other exercises (SMD, −0.84; 95% CI, −2.70 to 1.02; p = 0.38, Figure 5B). Sensitivity analyses yielded similar and non-significant differences for the above-mentioned outcomes.
Figure 5.
Forest plot of the effects of Baduanjin exercises on (A) body mass index and (B) wait-hip ratio.
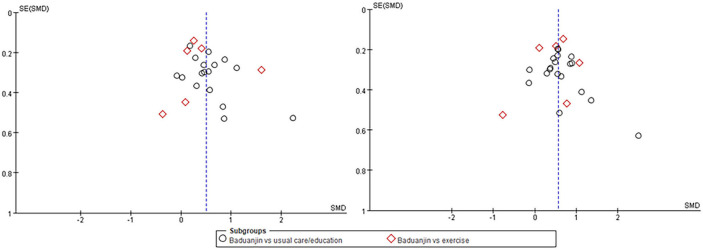
Publication bias
The funnel plots for Badunjin exercises for type 2 diabetes in FBG and HbA1c including 20 RCTs, respectively, are shown in Figure 6. The publication bias was small because the spots were substantially symmetric.
Figure 6.
The funnel plots for Badunjin exercises for type 2 diabetes in fasting blood glucose (left) and glycosylated hemoglobin (right).
Adverse events
None of the included studies reported whether there were adverse events or not.
Discussion
To our knowledge, the current study is the first systematic review that attempts to summarize and examines the effects on the psychological well-being of Baduanjin exercises, as the complementary therapy, for type 2 diabetes. The current results demonstrate that Baduanjin exercises can significantly improve the psychological well-being of patients with type 2 diabetes such as depression, anxiety, mental health, and global well-being. In glycemic control, Baduanjin exercises showed better improvements than usual care/education, but not other exercises. However, there was insufficient evidence on the long-term effects of Baduanjin exercises for type 2 diabetes.
The previous review reported that evidence from meta-analysis suggested that Baduanjin exercises plus conventional therapy have positive effects on the type 2 diabetes (8). In the included studies, conventional therapy included training, regular drug treatment, relaxation exercises, and regular healthcare. The control interventions included regular healthcare, regular drug treatment, and aerobics. However, the detailed subgroup analysis was not conducted based on different conventional therapy and control intervention. Furthermore, the effects on the psychological well-being of Baduanjin exercises for type 2 diabetes were not focused on the previous review. Baduanjin exercises, as the traditional Chinese mind-body exercises, have positive effects on anxiety and depression of patients with type 2 diabetes (10–12). Good psychological well-being could contribute to glycemic control. In our review, the study of Baduanjin exercises plus other exercises was not included. The detailed subgroup analysis was conducted based on different control interventions. And the current review showed the evidence of the effects on the psychological well-being of Baduanjin exercises, as the complementary therapy, for type 2 diabetes. Therefore, there was more powerful evidence on glycemic control and promoting psychological well-being of Baduanjin exercises for type 2 diabetes in our review.
Most included studies reported the beneficial effect on the quality of life and psychological well-being of Baduanjin exercises for type 2 diabetes. The results also supported the positive effects of Baduanjin exercises on improving depression, anxiety, mental health, and global well-being of patients with type 2 diabetes. Baduanjin exercises can effectively ameliorate the symptoms of depression and blood glucose levels of patients with type 2 diabetes possibly by regulating the dysregulated expression of lncRNA, mRNA, and circRNA (38). Compared with the conventional exercises focusing on strengthening physical health, Baduanjin exercises, as a traditional Chinese mind-body exercise, emphasize breathing regulation, an empty state of mindfulness, and musculoskeletal relaxation in order to maximize both physical and psychological well-being. These mindfulness-based elements are very important in reducing anxiety and depression (39). The rhythmic breathing regulation has a calming effect on stress-related behaviors (40). The previous study indicated that the effect in reducing depression of Baduanjin exercises was associated with increased levels of plasma adiponectin, which has an antidepressant-like function (41). The previous review also indicated positive effects in the quality of life and mental health of Baduanjin exercises for college students, elderly, and patients with chronic physical illnesses and mental problems (42). Li et al. (24) reported that Baduanjin exercises improved the sleep quality of type 2 diabetes that may promote psychological well-being.
In glycemic control, Baduanjin exercises, as a complementary therapy, showed better effects in FBG, HbA1c, and 2-hPBG than usual care/education. Based on the theories of traditional Chinese medicine, Baduanjin exercises could dredge meridians and collaterals, facilitate blood circulation, and regulate the internal organs to enhance one's health. The review also reported that Baduanjin exercises could modulate the blood lipid profile by decreasing total cholesterol, triglyceride, and low density lipoprotein cholesterol levels, and increasing high density lipoprotein cholesterol levels (43). However, the potential mechanism of Baduanjin exercises in modulating the blood glucose and lipid is unclear.
Compared with other exercises, Baduanjin exercises only showed better improvements in HbA1c, not in FBG or 2-hPBG. It may be associated with the low intensity and speed of Baduanjin exercises. As a mind-body exercise, Baduanjin practitioners pay more attention to unifying movements, breathing, and mindfulness for maximizing mind-body well-being. Therefore, the appropriate exercise intensity may get better health benefits from Baduanjin exercises. However, there were obvious differences in exercise time and frequency of Baduanjin exercises in the included studies. The long-term Baduanjin exercise may get more benefits for type 2 diabetes because 55% included studies had more than 24 weeks exercises. In the further, detailed dose-effect study of Baduanjin exercises for type 2 diabetes is warranted.
Limitations
In our review, some limitations should be considered. There were no restrictions in publication languages, but all of the included studies were published in Chinese. Therefore, Baduanjin exercises are not popular worldwide, and more studies and reports of Baduanjin exercises for type 2 diabetes are warranted. The methodological limitations of the eligible RCTs may also exaggerate the current results because the majority of the studies did not use concealed allocation and blinding. The blinding of therapists and participants is difficult for the studies of complementary and alternative therapies, such as Baduanjin exercises, but concealed allocation and blinding of assessors should be performed. In addition, there was high heterogeneity in some meta-analyses. Sensitivity analyses yielded similar and non-significant differences for the results. No clear source of heterogeneity was found. It may be due to the different frequency, duration, and session of Baduanjin exercises. In the included studies, the duration of Baduanjin exercises ranged from 4 to 48 weeks, the frequency ranging from 2 to 12 sessions per week, and the time of each session ranging from 20 to 90 min. Finally, no studies reported adverse effects of Baduanjin exercises for type 2 diabetes; but we could not confirm its safety.
Conclusions
The current review demonstrates that Baduanjin exercises can significantly improve psychological well-being of the patients with type 2 diabetes. There was beneficial evidence on glycemic control of Baduanjin exercises for type 2 diabetes. There was insufficient evidence on the long-term effects of Baduanjin exercises for type 2 diabetes; but traditional Chinese mind-body exercise-Baduanjin should be considered as a beneficial comprehensive therapy for type 2 diabetes, especially in promoting psychological well-being. Possible effective Baduanjin exercises are 30 min/day during 24 consecutive weeks based on the characteristics of the included studies.
There is further need of studies to assess the long-term effects of Baduanjin exercises for type 2 diabetes. Future research should explore the potential mechanisms by which Baduanjin exercises improve psychological well-being and glycemic control for type 2 diabetes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LK, JR, XZ, and MF conserved, designed the study, and wrote the draft manuscript. TH and JR performed the literature search. JR and SF identified and selected the studies. LK and XZ assessed the methodological quality and extracted data. XZ and MF performed data synthesis and analysis. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Shanghai Pujiang Program (21PJD071), Talent development program in Shanghai (2019048), and Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (ZYYCXTD-C-202008).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. (2015) 33:811–31. 10.1007/s40273-015-0268-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu C, Jia W. Diabetes in China: epidemiology and genetic risk factors and their clinical utility in personalized medication. Diabetes. (2018) 67:3–11. 10.2337/dbi17-0013 [DOI] [PubMed] [Google Scholar]
- 3.Confederation N. Investing in Emotional and Psychological Wellbeing for Patients With Long-Term Conditions. London, UK: NHS Confederation Mental Health Network; (2012). [Google Scholar]
- 4.Habtewold TD, Islam MA., Radie YT, Tegegne BS. Comorbidity of depression and diabetes: an application of biopsychosocial model. Int J Ment Health Syst. (2016) 10:74. 10.1186/s13033-016-0106-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. (2004) 27:2154–60. 10.2337/diacare.27.9.2154 [DOI] [PubMed] [Google Scholar]
- 6.Cheng AY. Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. Introduction. Can J Diabetes. (2013) 37:S1–3. 10.1016/j.jcjd.2013.04.005 [DOI] [PubMed] [Google Scholar]
- 7.Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American college of sports medicine and the American diabetes association: joint position statement executive summary. Diabetes Care. (2010) 33:2692–6. 10.2337/dc10-9990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wen J, Lin T, Cai Y, Chen Q, Chen Y, Ren Y, et al. baduanjin exercise for type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2017) 2017:8378219. 10.1155/2017/8378219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li M, Fang Q, Li J, et al. The effect of Chinese traditional exercise-baduanjin on physical and psychological well-being of college students: a randomized controlled trial. PLoS ONE. (2015) 10:e0130544. 10.1371/journal.pone.0130544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang X. Primary research of function on type 2 diabetic patients by gymnastic Qigong Baduanjin (dissertation/master's thesis). Beijing University of Chinese Medicine, Beijing, China; (2011). [Google Scholar]
- 11.Guan YX, Wang SS, Ma MN. Effect of Baduanjin-based exercise intervention on related parameters in type 2 diabetes patients. J Nurs Sci. (2012) 27:23–4. 10.3870/hlxzz.2012.19.02323507836 [DOI] [Google Scholar]
- 12.Ji X, Wang Q, Fang C. Effect of exercise therapy on anxiety and depression in the patients with diabetes mellitus. Pract Geriatr. (2012) 26:331–3. 10.3969/j.issn.1003-9198.2012.04.023 [DOI] [Google Scholar]
- 13.Macedo LG, Elkins MR, Maher CG, Moseley AM, Herbert RD, Sherrington C. There was evidence of convergent and construct validity of physiotherapy evidence database quality scale for physiotherapy trials. J Clin Epidemiol. (2010) 63:920–5. 10.1016/j.jclinepi.2009.10.005 [DOI] [PubMed] [Google Scholar]
- 14.Zhang L. Baduanjin for type 2 diabetes on psychological and physiological conditions (dissertation/master's thesis). China Academy of Chinese Medical Sciences, Beijing, China; (2006). [Google Scholar]
- 15.Wang YG, Liu LJ, Kou ZJ, Wang T. Baduanjin exercise as a complementary therapy for type 2 diabetes. Chin J Sports Med. (2007) 2:208–10. 10.16038/j.1000-6710.2007.02.019 [DOI] [Google Scholar]
- 16.Pan H, Feng Y. Experimental research of Baduanjin on rehabilitation of type 2 diabetes mellitus patients. J Guangzhou Univ Tradit Chin Med. (2008) 25:196–9. 10.13359/j.cnki.gzxbtcm.2008.03.026 [DOI] [Google Scholar]
- 17.Huang R. Deng X. Treatment of type 2 diabetes with Baduanjin. Hebei J Tradit Chin Med. (2011) 33:1828–9. [Google Scholar]
- 18.Zhou LB, Zhang JQ, Zhao XL. Baduanjin for in-home type 2 diabetes. Liaoning J Tradit Chin Med. (2011) 38:1564–5. 10.13192/j.1jtcm.2011.08.95.zhoulb.087 [DOI] [Google Scholar]
- 19.Duan JH, Li ZB, Li J. Baduanjin for the treatment of type 2 diabetes sufferers. Chin Commun Doc. (2012) 14:218–9. 10.3969/j.issn.1007-614x.2012.14.206 [DOI] [Google Scholar]
- 20.Liu Y, Huo R, Lai Y, et al. Community-based study on effects of Chinese Qigong-Baduanjin on depression symptoms and life quality of patients with type 2 diabetes mellitus. Chin J Sports Med. (2012) 31:212–7. 10.16038/j.1000-6710.2012.03.007 [DOI] [Google Scholar]
- 21.Li Z, Qi L, Zhao L, Liu H. Study on advantages of treating type 2 diabetes mellitus with Baduanjin for aerobic exercise. Liaoning J Tradit Chin Med. (2013) 40:1858–60. 10.13192/j.issn.1000-1719.2013.09.087 [DOI] [Google Scholar]
- 22.Lin Y, Wei J. Study of the intervention effect of health Qigong “Baduanjin” on type 2 diabetes. J Longyan Univ. (2013) 31:59–63. 10.16813/j.cnki.cn35-1286/g4.2013.02.014 [DOI] [Google Scholar]
- 23.Chen XY. The dose-effect relationship of Baduanjin assisted interventions in type 2 diabetes and explore the mechanism of inquiry (dissertation/master's thesis). Nanjing University of Chinese Medicine, Nanjing, China; (2014). [Google Scholar]
- 24.Li L, Wang N. Research progress of Baduanjin in the freament of insomnia patients with type 2 diabetes. Neimenggu J Tradit Chin Med. (2014) 33:86–7. 10.16040/j.cnki.cn15-1101.2014.27.281 [DOI] [Google Scholar]
- 25.Liu H, Chen Y, Yi X, et al. Effects of Baduanjin exercise prescription on physical and mental regulation in type 2 diabetes patients with anxiety. Hunan J TCM. (2014) 30:16–8. 10.16808/j.cnki.issn1003-7705.2014.07.007 [DOI] [Google Scholar]
- 26.Ren JQ. (2014) Clinical research on method of Qigong Baduanjin in patients with pre-diabetes (dissertation/master's thesis). Nanjing University of Chinese Medicine, Nanjing, China. [Google Scholar]
- 27.Wei Q, Wu Y. Clinical study of Baduanjin on health status in patients with type 2 diabetes. J Liaoning Univ Tradit Chin Med. (2014) 16:103–5. 10.13194/j.issn.1673-842x.2014.01.037 [DOI] [Google Scholar]
- 28.Zhou T. The effects of Baduanjin for 25 patients with diabetes on blood glucose and psychology. Neimenggu J Tradit Chin Med. (2014) 33:70. 10.16040/j.cnki.cn15-1101.2014.24.285 [DOI] [Google Scholar]
- 29.Peng D, Liu Y, Sheng Y, et al. Influence of Baduanjin on the anxiety state of type 2 diabetes mellitus. Henan Tradit Chin Med. (2015) 35:774–5. 10.16367/j.issn.1003-5028.2015.04.0327 [DOI] [Google Scholar]
- 30.Sun YQ. The effects of Baduanjin in the management of patients with diabetes and emotional disorders. Chin Rural Health Service Adm. (2015) 35:357–9. [Google Scholar]
- 31.Wang C, Zhang H. Influence of Baduanjin combined with routine treatment on blood glucose level in type 2 diabetic patients. China Med Pharm. (2015) 5:49–52. [Google Scholar]
- 32.Zhang S, Liu H, Li Z, et al. Observation of Baduanjin exercise on the improvement of type 2 diabetic peripheral neuropathy. Hebei J Tradit Chin Med. (2015) 37:1473–84. 10.3969/j.issn.1002-2619.2015.10.010 [DOI] [Google Scholar]
- 33.Yang Q, Huang R. Effects of Baduanjin on psychology and life quality of type 2 diabetes patients accompanied with depression. Chin Med Modern Dist Educ China. (2017) 15:52–4. 10.3969/j.issn.1672-2779.2017.12.023 [DOI] [Google Scholar]
- 34.He K, Zhu L, Lu X. Clinical study of Baduanjin on health status in patients with type 2 diabetes. Chin Gen Pract. (2017) 20:447–9. [Google Scholar]
- 35.Liu M. Effects of Baduanjin for type 2 diabetes on quality of life. Nurs Pract Res. (2017) 14:148–9. [Google Scholar]
- 36.Miao H. The effect on quality of life of Baduanjin for type 2 diabetes. Cardiovascular disease. J Integr Tradit Chin West Med. (2018) 6:173–4. 10.16282/j.cnki.cn11-9336/r.2018.09.124 [DOI] [Google Scholar]
- 37.Guo Q. Short-term observation of Baduanjin on self-efficacy and self-management ability of type 2 diabetes patients (dissertation/master's thesis). Capital University of Physical Education and Sprots, Beijing, China; (2019). [Google Scholar]
- 38.An T, He ZC, Zhang XQ, Li J, Chen AL, Ta F, et al. Baduanjin exerts anti-diabetic and anti-depression effects by regulating the expression of mRNA, lncRNA, and circRNA. Chin Med. (2019) 14:3. 10.1186/s13020-019-0225-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zou L, Yeung A, Quan X, Chu SSC, Hu X, Chan JMS, et al. Mindfulness-based Baduanjin Exercise for depression and anxiety in people with physical or mental illnesses: a systematic review and meta-analysis. Int J Environ Res Public Health. (2018) 15:321. 10.3390/ijerph15020321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yackle K, Schwarz LA, Kam K, Sorokin JM, Huguenard JR, Feldman JL, et al. Breathing control center neurons that promote arousal in mice. Science. (2017) 355:1411–5. 10.1126/science.aai7984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chan JS, Li A, Ng SM, Xu A, Yao TJ, Wang XM, et al. Adiponectin potentially contributes to the antidepressive effects of Baduanjin Qigong exercise in women with chronic fatigue syndrome-like illness. Cell Transplant. (2017) 26:493–501. 10.3727/096368916X694238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng FK. Effects of Baduanjin on mental health: a comprehensive review. J Bodyw Mov Ther. (2015) 19:138–49. 10.1016/j.jbmt.2014.11.001 [DOI] [PubMed] [Google Scholar]
- 43.Mei L, Chen Q, Ge L, Zheng G, Chen J. Systematic review of chinese traditional exercise baduanjin modulating the blood lipid metabolism. Evid Based Complement Altern Med. (2012) 2012:282131. 10.1155/2012/282131 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.