Abstract
Background and objectives
The risk of emergence agitation (EA) is high in patients undergoing nasal surgery. The aim of the present study was to investigate the incidence of EA in adults undergoing septoplasty and the effect of ketamine on EA.
Methods
In this randomized study, a total of 102 ASA I–II patients who underwent septoplasty between July 2018 and April 2019 were divided into two groups: ketamine (Group-K, n = 52) and saline (Group-S, n = 50). After anesthesia induction, Group-K was intravenously administered 20 mL of saline containing 1 mg kg−1 ketamine, whereas Group-S was administered 20 mL of saline. Sedation and agitation scores at emergence from anesthesia, incidence of cough, emergence time, and response to verbal stimuli time were recorded. The sedation/agitation and pain levels were recorded for 30 minutes in the recovery unit.
Results
There was no significant difference between the groups in terms of the incidence of EA (Group-K: 15.4%, Group-S: 24%). The incidence of cough during emergence was higher in Group-S than in Group-K, but the response time to verbal stimuli and emergence time were shorter in Group-S. The sedation and agitation scores were similar after surgery. Pain scores were higher in Group-S at the time of admission to the recovery unit and were similar between groups in the other time points.
Conclusion
Administration of 1 mg kg−1 ketamine after anesthesia induction does not affect the incidence of EA in patients undergoing septoplasty, but it prolongs the emergence and response time to verbal stimuli and reduces the incidence of cough.
Keywords: Emergence agitation, General anesthesia, Ketamine, Septoplasty
Introduction
Postanesthesia emergence agitation (EA) is an important clinical problem that occurs during the early period of recovery from anesthesia, and it causes problems such as self-extubation, catheter removal, bleeding and injury to patients and healthcare personnel, and a prolonged hospital stay.1, 2 Although EA is commonly observed in children after inhalation anesthesia, its incidence has been reported to be high in adults after certain surgeries, particularly ear, nose and throat surgeries. The pathophysiology of EA is still unclear, but a sense of suffocation can be the cause of the increased incidence of emergence agitation after nasal surgeries.2
Various anesthetic and analgesic drugs are used in the treatment of EA. However, the potential respiratory depression effect of such drugs may pose a risk to patients during the recovery period. Therefore, the prevention of EA is safer and of greater priority than its treatment.3
While several studies have shown that ketamine, a NMDA receptor antagonist frequently used for anesthesia, may reduce the incidence of EA in children, studies investigating the effect of ketamine on EA in adults are limited.4, 5 Therefore, the aims of the present study were to evaluate the incidence of EA in adults undergoing septoplasty and to investigate the effect of the administration of ketamine on EA.
Methods
After approval for the study was obtained from the hospital's ethics committee (FSM EAH-KAEK 2018/35) and informed consent was obtained from the patients, a total of 102 ASA (American Society of Anesthesiologists) physical status I–II adults who underwent septoplasty between July 2018 and April 2019 were included in the study.
Patients with a history of ketamine allergy, hypertension, coronary artery disease, arrhythmia, seizure, obstructive sleep apnea, glaucoma, kidney disease, or liver disease, as well as those with a body mass index of > 30 kg m−2 or cognitive dysfunction were excluded from the study.
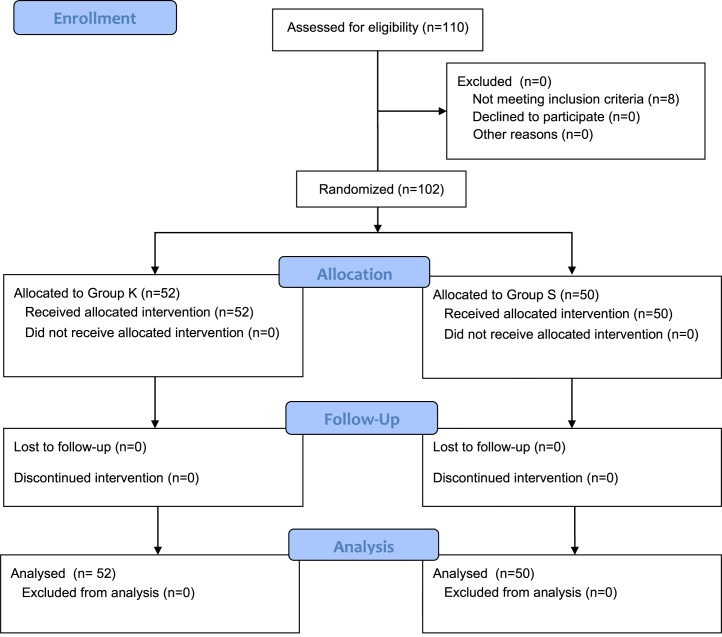
The sealed envelope technique was used for randomization, and each randomization result was written on paper and kept in an opaque sealed envelope that was labeled with a serial number. The sealed envelope was opened once the patient consented to participate in the study. Therefore, the patients were randomly divided into two groups: ketamine (Group-K) and saline (Group-S) (Figure 1). The patients were not informed about the group to which they were assigned. Their demographic data were recorded. The patients were taken to the operating room without premedication. After monitoring the peripheral capillary oxygen saturation level, noninvasive blood pressure, heart rate (HR), and Bispectral Index (BIS), anesthesia was induced with 2.5 mg kg−1 propofol, 2 mcg kg−1 fentanyl, and 0.6 mg kg−1 rocuronium, and the patients were intubated. Anesthesia was maintained by administering a mixture of 50% oxygen and 5–7% desflurane in air at a flow rate of 2 L min−1 with 0.05–0.5 mcg kg−1 min−1 remifentanil infusion such that the BIS remained between 40 and 60. The ventilator parameters were adjusted at a tidal volume of 7–8 mL kg−1 and a respiratory rate of 10–12 breaths.min−1 so that the end-tidal CO2 level remained between 30 and 35. Immediately after anesthesia was induced, 20 mL of normal saline containing 1 mg kg−1 ketamine was intravenously administered to Group-K in 10 minutes, whereas 20 mL of normal saline was intravenously administered to Group-S in 10 minutes. The solutions were prepared according to the relevant envelope containing the randomization result for each patient that was provided by a specialist physician who participated in the study randomization process but was not involved in the follow-up. The perioperative follow-up of the patients was performed by an anesthesiologist blinded to the administered drug. The oxygen saturation level (SPO2), mean arterial pressure (MAP), and HR were recorded every 15 minutes while the patient was under anesthesia. At 20 minutes before the end of the surgery, 1000 mg paracetamol and 1 mg kg−1 tramadol were intravenously administered. The total surgical duration was recorded after integral airway nasal packing was placed at the end of the surgery and inhalation anesthesia was discontinued. The patients were ventilated with 80% oxygen at a flow rate of 6 L min−1, and 0.03–0.05 mg kg−1 neostigmine and 0.02 mg.kg−1 atropine were intravenously administered to reverse the neuromuscular block. Patients who met the extubation criteria were extubated. The period between the discontinuation of inhalation anesthesia and 3 minutes after extubation was considered the emergence period, and this time was recorded. The agitation/sedation level during the emergence period was evaluated and recorded using the Riker Sedation/Agitation Scale (SAS) (Table 1), and patients with a SAS score ≥ 5 were considered agitated. Patients with an agitation score of 7 were intravenously administered 0.4 mg kg−1 propofol. The incidence of cough during emergence was scored as follows: 0, no cough; 1, a single cough; 2, nonpersistent cough lasting ≤ 5 s; and 3, persistent cough lasting > 5 s. The response time to verbal stimuli (the response to the question “how are you?”) was also recorded.
Figure 1.
CONSORT flow diagram.
Table 1.
Riker Sedation/Agitation Scale (SAS).
| Score | Term | Descriptor |
|---|---|---|
| 7 | Severely agitated | Remove endotracheal tubes, attempt to remove catheters, climb over bedrail, attack staff, thrash sideways |
| 6 | Very agitated | Do not calm down despite frequent verbal reminders of limits, require physical restraints, bite endotracheal tubes |
| 5 | Agitated | Display anxiety or mild agitated, attempt to sit up, calm down on verbal instructions |
| 4 | Calm, cooperative | Calm, easily arousable, follow verbal instructions |
| 3 | Sedated | Difficult to arouse, awaken to verbal stimuli or gentle shaking but drifts off again, follow simple verbal instructions |
| 2 | Highly sedated | Arouse to physical stimuli but do not communicate or follow verbal instructions, may move spontaneously |
| 1 | Unarousable | Minimal or no response to noxious stimuli, do not communicate or follow verbal instructions |
In the postanesthesia care unit (PACU), the sedation/agitation levels were evaluated with the SAS, whereas the pain scores were evaluated with the visual analogue scale (VAS) at 0, 10, 20 and 30 minutes. The SpO2, MAP, and HR were recorded at the same time points. The patients were also evaluated for nausea and other side effects. Patients with nausea and/or vomiting during the PACU follow-up were intravenously administered 0.1 mg kg−1 ondansetron. Patients with a modified Aldrete score of ≥ 9, 30 minutes after emergence were transferred to wards.
Statistical analysis
Continuous variables are presented as the mean ± standard deviation or the median (minimum-maximum), and categorical variables are presented as the frequency and percentage. The Shapiro–Wilk test was used to test the normality of the data. Continuous variables were compared using Student's t-test when the data were normally distributed and the Mann-Whitney U test when the data were non-normally distributed. For the response times to verbal stimuli at the different time points, the percent change values were calculated according to the baseline measurements. These percent change values were compared using the Mann-Whitney U test for the two groups. The Friedman test was used to assess the overall change in the variables. Post hoc analysis with the Wilcoxon signed-rank test was performed with Bonferroni's correction. Categorical variables were compared using Pearson's chi-squared test and Fisher's exact test. McNemar's test was used for the dependent categorical data. All statistical analyses were performed using IBM SPSS (v 23.0; IBM Corp. Released 2015; IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.).
The primary study outcome was the incidence of EA. Yu et al reported the incidence of EA to be 55.4% after ear, nose and throat surgeries.6 In a study conducted with nefopam, another NMDA antagonist, the authors accepted a significant decrease by 50% at this previously reported incidence.7 After performing a power analysis, we found that a sample size of 49 patients was needed in each group to detect a 50% reduction in the incidence of EA, with a power of 80% and an alpha value of 0.05. We enrolled 52 patients in Group-K and 50 in Group-S after considering that patients may drop out from the study.
Results
A total of 102 patients (Group-K: 52, Group-S: 50) were included in the present study. The patient demographics and surgical durations are summarized in Table 2.
Table 2.
Comparison of patient demographics and surgical duration.
| Group K (n = 52) | Group S (n = 50) | p | |
|---|---|---|---|
| Age, years (mean ± SD) | 33.54 ± 10.71 | 32.80 ± 10.35 | 0.724a |
| Female sex, n (%) | 15 (28.8%) | 18 (36.0%) | 0.440b |
| BMI, kg.m−2(mean ± SD) | 24.33 ± 3.30 | 24.08 ± 3.58 | 0.717a |
| ASA, n (%) | 0.422b | ||
| I | 41 (78.8%) | 36 (72.0%) | |
| II | 11 (21.2%) | 14 (28.0%) | |
| Surgical duration, minutes (median [min–max]) | 64.00 (27–210) | 55.00 (20–121) | 0.136c |
t-test.
Pearson's Chi-Squared test.
Mann-Whitney U-test, p < 0.05 was considered statistically significant.
The intraoperative and postoperative SpO2 values were similar between the two groups. In both groups, the intraoperative MAP and HR were significantly lower than the baseline measurements. At 45 minutes, the decrease in MAP compared with the baseline measurement was significantly higher in Group-K than in Group-S (p = 0.024); the MAP values were similar between the two groups at the other time points. The intraoperative HR was similar between the two groups at all time points.
The incidence of EA was similar between the two groups (Group-K: 15.4%, Group-S: 24%; p = 0.273). The patients’ age, ASA score and sex had no effect on the incidence of EA (p = 0.195, 1.000, and 0.064, respectively). The incidence of cough during emergence was higher in Group-S than in Group-K, whereas the emergence and response to verbal stimuli times were longer in Group-K (Table 3).
Table 3.
Riker Sedation/Agitation Scale (SAS) scores at emergence from anesthesia, incidence of cough and response time to verbal stimuli.
|
Group K (n = 52) |
Group S (n = 50) |
p | ||
|---|---|---|---|---|
| n (%) | n (%) | |||
| Emergence SAS | Agitated | 8 (15.4%) | 12 (24.0%) | 0.273a |
| Calm/Sedated | 44 (84.6%) | 38 (76.0%) | ||
| Cough incidence | None | 41 (78.8%) | 26 (52.0%) | 0.036a |
| Present | 11 (21.2%) | 24 (48.0%) | ||
| Emergence time (min) | Mean (SD) | 11.79 (4.65) | 7.54 (3.21) | <0.001b |
| Response to verbal stimuli time (min) | Mean (SD) | 13.48 (4.90) | 9.22(3.45) | <0.001b |
Agitated, SAS score of 5/6/7; Calm/Sedated, SAS score of 1/2/3/4; Cough classification, (0) – none; (1 to 3) – present.
Pearson Chi-Square test.
t-test, p < 0.05 was considered statistically significant.
During the PACU follow-up period, the patients had similar agitation incidence. Compared with Group-K, Group-S had a higher VAS score at the time of admission to the PACU (postoperative 0 min), but the pain level was similar at the other time points (Table 4). The MAP and HR values were similar between the groups in the postoperative follow-up.
Table 4.
Riker Sedation/Agitation Scale (SAS) and Visual Analogue Pain Scale (VAS) scores after surgery.
| Postoperative time (min) |
Group K (n = 52) |
Group S (n = 50) |
p | ||
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| SAS | 0 | Agitated | 0 (0.0%) | 1 (2.0%) | 0.490a |
| Calm/Sedated | 52 (100%) | 49 (98%) | |||
| 10 | Agitated | 0 (0.0%) | 0 (0.0%) | – | |
| Calm/Sedated | 52 (100%) | 50 (100%) | |||
| 20 | Agitated | 1 (1.9%) | 0 (0.0%) | 1.000a | |
| Calm/Sedated | 51 (98.1%) | 50 (100%) | |||
| 30 | Agitated | 1 (1.9%) | 0 (0.0%) | 1.000a | |
| Calm | 51 (98.1%) | 50 (100%) | |||
| VAS | 0 | Median (min–max) | 0 (0–5) | 1 (0–8) | 0.001b |
| 10 | Median (min–max) | 0 (-1–5) | 0 (-2–3) | 0.108b | |
| 20 | Median (min–max) | 0 (-2–6) | 0 (-2–5) | 0.213b | |
| 30 | Median (min–max) | 0 (-2–6) | 0 (-5–5) | 0.181b |
Agitated, SAS score of 5/6/7; Calm/Sedated, SAS score of 1/2/3/4.
Fisher's exact test.
Mann-Whitney U-test, p < 0.05 was considered statistically significant.
During the postoperative follow-up period, nausea was observed in 2 patients (3.8%) in Group-K and 5 (10%) in Group-S (p = 0.265). Bleeding was observed in 1 patient (1.9%) in Group-K, hallucination was observed in 1 patient (1.9%) in Group-K, and cough was observed in 3 patients (6%) in Group-S. The complication rates were similar between the two groups (p = 0.145).
Discussion
In this study, we investigated the effect of ketamine on EA in adults undergoing septoplasty and found that the incidence of EA was 24% in Group-S and that ketamine did not reduce the incidence of EA. Group-K had a lower incidence of cough during emergence but longer emergence and response to verbal stimuli times than Group-S.
Although the mechanism underlying the occurrence of EA has not been fully elucidated, several factors are known to trigger its occurrence. One such factor is the sense of suffocation caused by nasal packing placed after nasal surgery.6 Practices such as those not involving the use of nasal packing or the use of integral airway nasal packing may reduce the risk of EA. Studies have reported that the incidence of EA after nasal surgery may be > 50%.3, 6 In our study, the incidence of EA was found to be 24%; this discrepancy may be due to the use of integral airway nasal packing in our study, which reduced the sense of suffocation experienced by the patients. Furthermore, to the best of our knowledge, the present study is the first to investigate the effect of ketamine on EA in adults undergoing septoplasty. The fact that only patients who underwent septoplasty were included in this study, rather than all patients who underwent any type of nasal surgery, might have been a factor that reduced the sense of suffocation experienced by the patients and led to a low incidence of EA because this subset of patients is more used to, or familiar with, experiencing chronic nasal obstruction.
Although EA may occur after painless procedures, pain has been defined as one of the most important factors causing EA. In their study examining EA after nasal surgery, Kim et al reported that an NRS of ≥ 5 was an independent risk factor for EA.8 Some studies have reported that the use of drugs with analgesic properties, such as nefopam, dexmedetomidine, and opioids, reduces the risk of EA.4, 7, 9 In a study that investigated rhinoplasties, it was reported that severe postoperative pain was an important risk factor for the development of EA and that the use of ketamine at subanesthetic doses was useful in reducing the incidence of EA.3 In another study, nefopam, an NMDA antagonist, was reported to reduce EA after nasal surgery.7 Pediatric studies have also reported that ketamine can reduce the incidence of EA.4, 5 In a previous study, it was reported that the administration of ketamine was not effective in preventing the occurrence of EA after inhalation anesthesia in children subjected to caudal blocks and that pain is the primary factor in the development of EA.10 In our study, the pain score was found to be low in both groups. The VAS score was higher in Group-S than in Group-K at the time of admission to the PACU (postoperative 0 min). The terminal plasma half-life of ketamine after intravenous administration is reportedly 186 minutes.11 A low VAS score at the time of admission to the PACU may be due to the analgesic effect of ketamine. However, although the VAS score of Group-S was significantly higher than that of Group-K, the median VAS score of Group-S was 1 (0–8). Therefore, the absence of a difference between the groups in terms of the incidence of EA can be attributed to the low postoperative pain levels in both groups. A young age, the male sex, and a high ASA score were reported to be factors that increase the incidence of EA.8 In our study, the patients’ age, ASA score and sex did not have an effect on the incidence of EA. Furthermore, the age and sex distributions were similar between the two groups. Hence, it is concluded that the incidence of EA was not affected by demographic factors.
The dose and time of administration tend to differ among studies investigating the effect of ketamine on the incidence of EA. In some studies, ketamine was administered after anesthesia induction or before the end of surgery.4, 12 In a study conducted in children, it was reported that ketamine administered at a dose of 0.25 mg kg−1 10 minutes before the end of surgery decreased the incidence of EA without affecting the recovery period.9 It was reported that the administration of a 1 mg kg−1 bolus and 1 mg kg−1.h−1 ketamine decreased the incidence of EA in children, but it delayed their mental orientation.4 Demir et al administered 0.5 mg kg−1 ketamine 20-minutes before the end of surgery to adults undergoing rhinoplasty and reported that the duration of anesthesia was longer in this group than that in the control group.3 In our study, the infusion of 1 mg kg−1 ketamine for 10 minutes after anesthesia induction was preferred, and the emergence and response to verbal stimuli times were found to be longer in Group-K than in Group-S. This effect might not have been observed if lower doses of ketamine had been administered.
The incidence of EA during extubation in the operating room is reportedly higher than that of EA in the PACU.13 In our study, all patients were followed for 30 minutes during the postoperative period, and EA was evaluated during emergence and in the PACU. After surgery, the SAS score distribution was found to be similar between the two groups, and the number of agitated patients was lower in the PACU as compared to the emergence from anesthesia.
Reducing the incidence of cough during emergence after nasal surgery is important for preventing bleeding at the surgical site. Studies have reported that ketamine reduces fentanyl-induced cough.14, 15 In our study, the incidence of cough during emergence was found to be lower in Group-K than in Group-S. We believe that the administration of a low dose of ketamine is a good alternative method for preventing bleeding complications in surgeries wherein cough prevention is important, such as nasal and endoscopic sinus surgery.
In a study conducted in adults, it was reported that ketamine had no effect on the incidence of nausea and vomiting after rhinoplasty.3 In another study conducted on children, a placebo and different doses of ketamine (0.2 and 0.5 mg kg−1) were used, and the rates of postoperative nausea and vomiting were found to be similar across all groups.12 In our study, no difference was found between the groups in terms of the occurrence of nausea/vomiting and other complications during the PACU follow-up period.
In nasal surgery, controlled hypotension is important for preventing bleeding, facilitating the application of surgical techniques, and reducing the surgical duration. Ketamine leads to central sympathetic activation by preventing neuronal catecholamine reuptake and stimulating norepinephrine, dopamine, and serotonin release from noradrenergic neurons, which in turn increases the individual's blood pressure and HR.16 In our study, the intraoperative MAP and HR decreased in both groups compared with the baseline measurements. The vital signs during the postoperative period were similar between the two groups. Therefore, the administration of a low dose of ketamine did not have any negative hemodynamic effects in patients undergoing septoplasty.
The present study has some limitations. In the postoperative period, all patients were followed only until discharge from the PACU. Therefore, a significant difference might have been observed in the pain scores between the groups, if the patients were followed over a longer period of time after surgery. Furthermore 102 patients were included in the study; although the number of patients included in the study was not small, a larger sample size might have revealed a difference between the groups in terms of the incidence of EA.
Conclusion
The intraoperative administration of ketamine does not reduce the incidence of EA following septoplasty, but it is effective in reducing the incidence of cough during emergence. In surgery wherein hypotensive anesthesia is performed, the administration of 1 mg kg−1, ketamine does not have any negative effects on hemodynamics.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Kim Y.S., Chae Y.K., Choi Y.S., et al. A comparative study of emergence agitation between sevoflurane and propofol anesthesia in adults after closed reduction of nasal bone fracture. Korean J Anesthesiol. 2012;63:48–53. doi: 10.4097/kjae.2012.63.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee S.J., Choi S.J., In C.B., Sung T.Y. Effects of tramadol on emergence agitation after general anesthesia for nasal surgery: A retrospective cohort study. Medicine. 2019;98:e14763. doi: 10.1097/MD.0000000000014763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demir C.Y., Yuzkat N. Prevention of emergence agitation with ketamine in rhinoplasty. Aesthetic Plast Surg. 2018;42:847–853. doi: 10.1007/s00266-018-1103-4. [DOI] [PubMed] [Google Scholar]
- 4.Chen J.Y., Jia J.E., Liu T.J., Qin M.J., Li W.X. Comparison of the effects of dexmedetomidine, ketamine, and placebo on emergence agitation after strabismus surgery in children. Can J Anaesth. 2013;60:385–392. doi: 10.1007/s12630-013-9886-x. [DOI] [PubMed] [Google Scholar]
- 5.Abu-Shahwan I., Chowdary K. Ketamine is effective in decreasing the incidence of emergence agitation in children undergoing dental repair under sevoflurane general anesthesia. Paediatr Anaesth. 2007;17:846–850. doi: 10.1111/j.1460-9592.2007.02298.x. [DOI] [PubMed] [Google Scholar]
- 6.Yu D., Chai W., Sun X., Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anaesth. 2010;57:843–848. doi: 10.1007/s12630-010-9338-9. [DOI] [PubMed] [Google Scholar]
- 7.Jee Y.S., You H.J., Sung T.Y., Cho C.K. Effects of nefopam on emergence agitation after general anesthesia for nasal surgery: A prospective, randomized, and controlled trial. Medicine. 2017;96:e8843. doi: 10.1097/MD.0000000000008843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim H.J., Kim D.K., Kim H.Y., Kim J.K., Choi S.W. Risk factors of emergence agitation in adults undergoing general anesthesia for nasal surgery. Clin Exp Otorhinolaryngol. 2015;8:46–51. doi: 10.3342/ceo.2015.8.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polat R., Peker K., Baran I., Bumin Aydın G., Topçu Gülöksüz Ç., Dönmez A. Comparison between dexmedetomidine and remifentanil infusion in emergence agitation during recovery after nasal surgery: A randomized double-blind trial. Anaesthesist. 2015;64:740–746. doi: 10.1007/s00101-015-0077-8. [DOI] [PubMed] [Google Scholar]
- 10.Ozcan A., Kaya A.G., Ozcan N., et al. Effects of ketamine and midazolam on emergence agitation after sevoflurane anaesthesia in children receiving caudal block: a randomized trial. Rev Bras Anestesiol. 2014;64:377–381. doi: 10.1016/j.bjan.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Zanos P., Moaddel R., Morris P.J., et al. Ketamine and Ketamine Metabolite Pharmacology: Insights into Therapeutic Mechanisms. Pharmacol Rev. 2018;70:621–660. doi: 10.1124/pr.117.015198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee Y.S., Kim W.Y., Choi J.H., Son J.H., Kim J.H., Park Y.C. The effect of ketamine on the incidence of emergence agitation in children undergoing tonsillectomy and adenoidectomy under sevoflurane general anesthesia. Korean J Anesthesiol. 2010;58:440–445. doi: 10.4097/kjae.2010.58.5.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munk L., Andersen G., Møller A.M. Post-anaesthetic emergence delirium in adults: incidence, predictors and consequences. Acta Anaesthesiol Scand. 2016;60:1059–1066. doi: 10.1111/aas.12717. [DOI] [PubMed] [Google Scholar]
- 14.Saleh A.J., Zhang L., Hadi S.M., Ouyang W. A priming dose of intravenous ketamine-dexmedetomidine suppresses fentanyl-induced coughing: a double-blind, randomized, controlled study. Ups J Med Sci. 2014;119:333–337. doi: 10.3109/03009734.2014.968270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guler G., Aksu R., Bicer C., Tosun Z., Boyacı A. Comparison of the effects of ketamine or lidocaine on fentanyl-induced cough in patients undergoing surgery: A prospective, double-blind, randomized, placebo-controlled study. Curr Ther Res Clin Exp. 2010;71:289–297. doi: 10.1016/j.curtheres.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peltoniemi M.A., Hagelberg N.M., Olkkola K.T., Saari T.I. Ketamine: a review of clinical pharmacokinetics and pharmacodynamics in anesthesia and pain therapy. Clin Pharmacokinet. 2016;55:1059–1077. doi: 10.1007/s40262-016-0383-6. [DOI] [PubMed] [Google Scholar]