Abstract
Healthcare delivery reorganization during the COVID-19 emergency may have had a significant impact on access to care for older adults with chronic conditions. We investigated such impact among all adults with chronic conditions aged ≥ 65 years, identified through the electronic health databases of two local health agencies—ATS Brianza and ATS Bergamo—from the Lombardy region, Italy. We considered hospitalizations for 2020 compared to the average 2017–2019 and quantified differences using rate ratios (RRs). Overall, in 2017–2019 there were a mean of 374,855 older adults with ≥ 1 chronic condition per year in the two ATS and 405,371 in 2020. Hospitalizations significantly decreased from 84,624 (225.8/1000) in 2017–2019 to 78,345 (193.3/1000) in 2020 (RR 0.86). Declines were reported in individuals with many chronic conditions and for most Major Diagnostic Categories, except for diseases of the respiratory system. The strongest reductions were observed in hospitalizations for individuals with active tumours, particularly for surgical ones. Hospitalization rates increased in individuals with diabetes, likely due to COVID-19-related diseases. Although determinants of the decrease in demand and supply for care among chronic older adults are to be further explored, this raises awareness on their impacts on chronic patients’ health in the medium and long run.
Subject terms: Cancer, Cardiovascular diseases, Diabetes
Introduction
Since the end of January 2020, COVID-19—a disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—started to spread around the globe, and on March 11, 2020 the World Health Organization (WHO) declared a global pandemic1,2. In Italy, COVID-19 was first registered on February 21, 2020 in Codogno, Lombardy region, and it rapidly spread mainly in Northern Italy3–5. The Lombardy region was particularly hit by the pandemic, as it represents the Italian area with the highest COVID-19 incidence and death rates. In order to control the spread of COVID-19, from March 9 until May 4, 2020 a strict lockdown was imposed to the Italian population which limited all unnecessary activities6. By the end of September 2020—due to a second wave of COVID-19 infection—new lockdowns were ordered, with curfew and several gradients of restriction7,8.
Due to the high infection rate of SARS-CoV-2, the COVID-19 epidemic has placed strong pressure on the health care system and service delivery in Italy, as in most other countries around the globe9,10. Regional health services were reorganized, reducing access to outpatient and inpatient care only to urgent and essential situations and concentrating in specific hospital hubs the provision of health services for patients whose treatments could not be postponed11,12. Such measures may have significantly impacted on the population health, particularly for older adults with chronic conditions. Indeed, besides direct short-term health risks associated with SARS-CoV-2 infection due to their higher vulnerability to COVID-19 morbidity and mortality13–17, old chronic patients have been also at a higher risk of impaired health care, due to the limitations in the access to territorial and hospital health services they need during the COVID-19 outbreaks18,19. A few earlier studies have shown that emergency visits and hospitalizations decreased during the first waves of the COVID-19 pandemic in Italy20,21. A study conducted in seven hospitals from Italy showed that cancer diagnosis fell by 49% in 2020 compared with the average records of 2018–201922. A retrospective study conducted in four hospitals from New York City during the pre, early, peak, and late COVID-19 epidemic found substantial decreases of non-COVID-19 hospitalizations in the peak COVID-19 period, the declines being observed across all diagnoses23. A retrospective analysis of national utilization data from Greece reported that hospital admissions and hospital surgical procedures significantly dropped by 17.3% and 24.8% respectively during the first 9 months of the epidemic compared to the average utilization rates of 2017–201924.
To date, however, data on hospitalization patterns in individuals with chronic conditions are still scant at national and international level. With the present study, we aim to investigate and quantify the impact of the COVID-19 pandemic on the access to hospital services of older adults with chronic conditions using real-world data from the public health informative system of two large local health agencies from the Lombardy region, Italy.
Results
Overall, there were an average of 374,855 individuals aged 65 years or more with a chronic condition per year in 2017–2019 and 405,371 in 2020. In 2020, 55.2% of individuals were women, mean age was 76.7 years (standard deviation 7.7), 46.9% of individuals were at low level of complexity and 5.4% at high level (Table 1). Most frequent chronic conditions were diabetes (10.2%), ischemic cardiopathy (7.4%), arrhythmic cardiomyopathy (5.7%), active tumours (5.7%), and heart failure (5.2%). Similar distributions were observed in 2017–2019. Moreover, the distribution of patients’ characteristics was comparable between the two ATS (Supplementary Table 1).
Table 1.
Characteristics of individuals aged 65 years or more with a chronic disease from ATS Brianza and ATS Bergamo combined in 2017–2019 and 2020. Lombardy, Italy.
| N. patients (%) | ||
|---|---|---|
| Average 2017–2019 |
2020 | |
| Total | 374,855 | 405,371 |
| Sex | ||
| Men | 166,486 (44.4) | 181,583 (44.8) |
| Women | 208,369 (55.6) | 223,788 (55.2) |
| Age (years) | ||
| 65–69 | 87,358 (23.3) | 84,279 (20.8) |
| 70–74 | 88,161 (23.5) | 96,162 (23.7) |
| 75–79 | 81,982 (21.9) | 78,824 (19.4) |
| 80–84 | 64,054 (17.1) | 75,154 (18.5) |
| ≥ 85 | 53,300 (14.2) | 70,952 (17.5) |
| Level of complexity | ||
| Low | 175,758 (46.9) | 190,222 (46.9) |
| Medium | 178,840 (47.7) | 193,274 (47.7) |
| High | 20,257 (5.4) | 21,875 (5.4) |
| Chronic conditions | ||
| Diabetes | 38,334 (10.2) | 41,406 (10.2) |
| Respiratory diseases | ||
| Asthma | 1500 (0.4) | 1755 (0.4) |
| COPD | 10,108 (2.7) | 10,790 (2.7) |
| Tumours | ||
| Tumours, active | 21,314 (5.7) | 23,192 (5.7) |
| Tumours, follow-up | 7079 (1.9) | 7679 (1.9) |
| Tumours, remission | 8356 (2.2) | 8956 (2.2) |
| Cardiovascular diseases | ||
| Ischemic cardiopathy | 27,960 (7.5) | 29,969 (7.4) |
| Valvular cardiopathy | 5531 (1.5) | 6123 (1.5) |
| Non-arrhythmic myocardiopathy | 13,829 (3.7) | 14,994 (3.7) |
| Arrhythmic myocardiopathy | 21,648 (5.8) | 23,202 (5.7) |
| Heart failure | 19,831 (5.3) | 21,082 (5.2) |
| Arterial vasculopathy | 9756 (2.6) | 10,323 (2.5) |
| Cerebral vasculopathy | 13,667 (3.6) | 14,304 (3.5) |
| Renal diseases | ||
| Chronic renal failure | 8454 (2.3) | 9411 (2.3) |
| Liver diseases | ||
| Hepatic cirrhosis | 2145 (0.6) | 2302 (0.6) |
| Chronic hepatitis | 5513 (1.5) | 6032 (1.5) |
| Rheumatoid arthritis | 2534 (0.7) | 3223 (0.8) |
| Digestive diseases | ||
| Ulcerative colitis/Crohn | 1322 (0.4) | 1474 (0.4) |
| Thyroid diseases | ||
| Hypothyroidism | 3810 (1.0) | 4649 (1.1) |
| Basedow’s disease/hyperthyroidism | 376 (0.1) | 464 (0.1) |
| Hashimoto thyroiditis | 745 (0.2) | 934 (0.2) |
COPD chronic obstructive pulmonary disease.
Number and rates of hospitalizations in older adults with chronic conditions from the two ATS combined in 2017–2019 and 2020 are presented in Table 2. Overall hospitalizations significantly decreased from 84,624 (225.8/1000) in 2017–2019 to 78,345 (193.3/1000) in 2020, with a RR of 0.86. The strongest decreases were observed in day-hospital (RR = 0.71) and in surgical hospitalizations (RR = 0.72). With reference to level of complexity of chronic conditions, significant decreases were observed in both medium (RR = 0.83) and high level (RR = 0.62) hospitalizations. Results were very similar in the two ATS (Supplementary Table 2). Considering non-chronic individuals, we observed even stronger reduction in hospitalizations in 2020 as compared to 2017–2019 (RR = 0.69; Supplementary Table 3).
Table 2.
Number of hospitalizations and corresponding rates (per 1000) among individuals aged 65 years or more with at least a chronic disease from ATS Brianza and ATS Bergamo combined, overall and by hospital regimen, type of hospitalization and level of complexity, in 2017–2019 and 2020, and rate ratio for 2020 versus 2017–2019, Lombardy, Italy.
| Average 2017–2019 |
2020 | Rate ratio (95% CI) | |||
|---|---|---|---|---|---|
| N | Rate | N | Rate | ||
| Overall | 84,624 | 225.8 | 78,345 | 193.3 | 0.86 (0.85–0.86) |
| Hospital regimena | |||||
| Ordinary | 72,565 | 193.6 | 68,149 | 168.1 | 0.87 (0.86–0.88) |
| Day-hospital | 10,849 | 28.9 | 8357 | 20.6 | 0.71 (0.69–0.73) |
| Type of diagnosis-related group | |||||
| Medical | 43,702 | 116.6 | 46,641 | 115.1 | 0.99 (0.97–1.00) |
| Surgical | 40,912 | 109.1 | 31,704 | 78.2 | 0.72 (0.71–0.73) |
| Level of complexity | |||||
| Low | 24,662 | 65.8 | 27,552 | 68.0 | 1.03 (1.02–1.05) |
| Medium | 47,045 | 125.5 | 42,108 | 103.9 | 0.83 (0.82–0.84) |
| High | 12,916 | 34.5 | 8685 | 21.4 | 0.62 (0.60–0.64) |
95% CI 95% confidence interval.
aThis category does not include sub-acute hospitalizations, included in overall hospitalizations.
Hospitalizations significantly decreased between 2017–2019 and 2020 in older adults with active tumours (RR = 0.47), ischemic cardiopathy (RR = 0.90), valvular cardiopathy (RR = 0.69), heart failure (RR = 0.76), arterial vasculopathy (RR = 0.63), cerebral vasculopathy (RR = 0.53), and chronic renal failure (RR = 0.71; Table 3). On the contrary, hospitalizations significantly increase in individuals with diabetes (RR = 1.30), chronic obstructive pulmonary disease (COPD; RR = 1.24), cancers in follow-up (RR = 1.38) and in remission (RR = 1.41), non-arrhythmic myocardiopathy (RR = 1.18), while no meaningful changes were found in individuals with other chronic conditions. Again, findings were consistent in the two ATS (Supplementary Table 4).
Table 3.
Number of hospitalizations and corresponding rate (per 1000) among individuals aged 65 years or more with a chronic disease from ATS Brianza and ATS Bergamo by major chronic diseases in 2017–2019 and 2020, and rate ratio between the two periods. Lombardy, Italy.
| Average 2017–2019 |
2020 | Rate ratio (95% CI) | |||
|---|---|---|---|---|---|
| N | Rate | N | Rate | ||
| Diabetes | 5204 | 135.8 | 7337 | 177.2 | 1.30 (1.26–1.35) |
| Respiratory diseases | |||||
| Asthma | 169 | 112.7 | 200 | 114.0 | 1.01 (0.82–1.24) |
| COPD | 1643 | 162.5 | 2173 | 201.4 | 1.24 (1.16–1.32) |
| Tumours | |||||
| Tumours, active | 16,156 | 758.0 | 8217 | 354.3 | 0.47 (0.46–0.48) |
| Tumours, follow-up | 817 | 115.4 | 1227 | 159.8 | 1.38 (1.27–1.51) |
| Tumours, remission | 734 | 87.8 | 1110 | 123.9 | 1.41 (1.29–1.55) |
| Cardiovascular diseases | |||||
| Ischemic cardiopathy | 6637 | 237.4 | 6391 | 213.3 | 0.90 (0.87–0.93) |
| Valvular cardiopathy | 1724 | 311.7 | 1324 | 216.2 | 0.69 (0.65–0.75) |
| Non arrhythmic myocardiopathy | 1832 | 132.5 | 2345 | 156.4 | 1.18 (1.11–1.25) |
| Arrhythmic myocardiopathy | 4872 | 225.1 | 5080 | 218.9 | 0.97 (0.93–1.01) |
| Heart failure | 8052 | 406.0 | 6521 | 309.3 | 0.76 (0.74–0.79) |
| Arterial vasculopathy | 5689 | 583.1 | 3813 | 369.4 | 0.63 (0.61–0.66) |
| Cerebral vasculopathy | 5989 | 438.2 | 3328 | 232.7 | 0.53 (0.51–0.55) |
| Renal diseases | |||||
| Chronic renal failure | 4211 | 498.1 | 3326 | 353.4 | 0.71 (0.68–0.74) |
| Liver diseases | |||||
| Hepatic cirrhosis | 681 | 317.5 | 731 | 317.5 | 1.00 (0.90–1.11) |
| Chronic hepatitis | 578 | 104.8 | 807 | 133.8 | 1.28 (1.15–1.42) |
| Rheumatoid arthritis | 381 | 150.4 | 530 | 164.4 | 1.09 (0.96–1.25) |
| Digestive diseases | |||||
| Ulcerative colitis/Crohn | 200 | 151.3 | 224 | 152.0 | 1.00 (0.83–1.22) |
| Thyroid diseases | |||||
| Hypothyroidism | 340 | 89.2 | 404 | 86.9 | 0.97 (0.84–1.13) |
| Basedow’s disease/hyperthyroidism | 24 | 63.8 | 36 | 77.6 | 1.22 (0.73–2.04) |
| Hashimoto thyroiditis | 48 | 64.4 | 88 | 94.2 | 1.46 (1.03–2.08) |
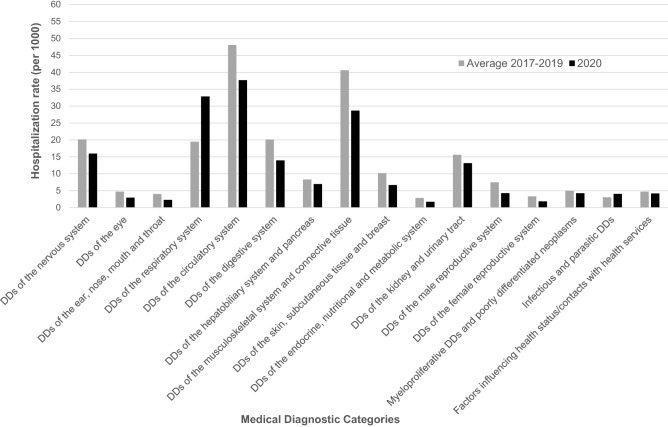
When we analysed hospitalizations for individuals with active tumours according to type of hospitalization, we found that the reductions were greater for surgical (490.9/1000 vs 160.1/1000, RR = 0.33, 95% CI 0.31–0.34) than for medical hospitalizations (267.0/1000 vs 151.0/1000, RR = 0.57, 95% CI 0.54–0.59; data not shown). Hospitalization rates declined between 2017–2019 and 2020 for most MDCs, with the exception of diseases of the respiratory system, for which rates significantly increased (from 19.7/1000 to 34.3/1000, RR = 1.75; Fig. 1). Consistent patterns were found in ATS Brianza (Supplementary Fig. 1A) and ATS Bergamo (Supplementary Fig. 1B).
Figure 1.
Hospitalization rates (per 1000) among individuals aged 65 years or more with a chronic disease from ATS Monza-Brianza and ATS Bergamo combined according to Major Diagnostic Categories in 2017–2019 and 2020. DD diseases and disorders.
Considering individuals with diabetes, we found significant decreases for diseases of the musculoskeletal system and connective tissue (from 35.7/1000 to 27.0/1000, RR = 0.76, in ATS Brianza and from 43.1/1000 to 29.9/1000, RR = 0.69, in ATS Bergamo), while there were significant increases for other diseases, including in particular those of the nervous (from 6.8/1000 to 14.6/1000, RR = 2.15, and from 10.8/1000 to 16.1/1000, RR = 1.49), respiratory (from 9.3/1000 to 32.2/1000, RR = 3.46, and from 8.9 to 32.4/1000, RR = 3.64), and circulatory system (from 15.1/1000 to 31.5/1000, RR = 2.093, and from 16.5/1000 to 30.3/1000, RR = 1.84; Supplementary Fig. 2A,B). As a consequence, although the top most MDCs responsible for hospital admission among individuals with diabetes were similar in the two calendar periods, diseases of the respiratory system ranked 1° in 2020 in the two ATS compared to 5° in ATS Brianza and 6° in ATS Bergamo in 2017–2019 (Supplementary Table 5).
Among individuals with an active tumour, we found significant decreases for most MDCs, including in particular those of the skin, subcutaneous tissue, and breast (MDC 09), from 108.7/1000 to 16.0/1000, RR = 0.15 in ATS Brianza and from 156.8 to 22.7/1000, RR = 0.14 in ATS Bergamo) (Supplementary Fig. 3A,B). Among those individuals, diseases of the respiratory system ranked 1° in 2020 (they were 4° in ATS Brianza and 6° in ATS Bergamo in 2017–2019), while diseases of the skin, subcutaneous tissue, and breast ranked 9° and 7° respectively in ATS Brianza and ATS Bergamo in 2020, while they were 2° and 1° in 2017–2019; Supplementary Table 6).
Discussion
In our study, we found that in Lombardy—one of the most heavily areas hit by COVID-19 pandemic in Italy, probably on account of its elderly population and the fact that was the first area to be reached by COVID-19 outside China—hospitalizations in older chronic patients have decreased by about 14% compared to the three previous years a consequence of the pressure the COVID-19 pandemic posed on health services. Such decreases were observed mainly for day-hospital hospitalizations and those involving surgical procedures. Consistent reductions in hospitalizations were found in individuals with many chronic conditions, but they were stronger in those with active tumours (by 53%), particularly when necessitating surgery (by 67%). We observed a decrease in hospitalizations for most MDCs, with the exception of those of the respiratory system, which are likely related to COVID-19. Considering the fact that we did not exclude hospitalizations due to COVID-19-related diagnoses, the reductions in hospital access during the 2020 COVID-19 pandemic could have been even larger in these populations. This notwithstanding, the declines in hospitalizations for chronic patients were more limited than those observed in non-chronic individuals.
Studies on the impact of COVID-19 emergency on hospitalization patterns in individuals with chronic conditions are scanty. A few earlier studies investigated hospitalization for acute (mainly cardiovascular) conditions and access to emergency departments, reporting significant reductions in hospitalization for acute myocardial infarction, stroke, heart failure, and other cardiovascular diseases20,21,23,25–31.
Consistently, in our study we found that individuals with various cardiovascular conditions, including ischemic and valvular cardiopathy, heart failure, and arterial and cerebral vasculopathy, had a reduced access to hospital during 2020. This notwithstanding the fact that individuals with cardiovascular diseases—as those with many other chronic conditions—may have been at an increased risk of hospitalization for COVID-1915,17.
To the best of our knowledge no study investigated the impact of COVID-19 in individuals with diabetes32. We found an approximately 30% increase in hospitalizations for individuals with diabetes. This appears to be largely due to the rises in hospitalizations due to diseases of the nervous, respiratory, and circulatory system, which are likely attributable to COVID-19. Patients diabetes have indeed been reported to be among those at a high risk of more severe SARS-CoV-2 infection requiring hospitalization, due to the frequent presence of other concomitant disease15,17. The significant reduction in hospitalizations for diseases of the skin, musculoskeletal and connective tissue, on the contrary, can be due to a more frequent treatment at home during the COVID-19 emergency of diabetes-related complications included in MDC 09.
A few previous studies, mainly conducted in a single centre and on specific cancer sites, reported a reduction in hospital access in cancer patients during 202030. Our study confirms that hospitalizations for individuals with an active tumour, particularly those involving surgery, were strongly reduced during the COVID-19 pandemic in 2020. In cancer patients, hospitalizations declined particularly for diseases in MDC 09 which include malignancies of the breast. Our data underline the difficulty in providing optimal health care in cancer patients, that appear to be among those that suffered the most for the lack of necessary cure during the COVID-19 crisis33. The reduction in hospitalizations for cancer patients may have significant long-term effects on morbidity and mortality in those patients. It has indeed been estimated that even modest delays in surgery for cancer will determine a significant impact on survival34, and a few studies already reported an increase in out-of-hospital mortality mainly driven by deaths for neoplasms, cardiovascular and endocrine diseases20, although there will need some more time to quantify the exact extent of such impact.
With reference to respiratory diseases, we found an increase in hospitalizations for COPD but not for asthma. The increases in hospitalization of patients with COPD are likely due to the higher frequency of severe relapse of the illness and also of potentially COVID-19-related diseases, which have been shown to be at increased risk of SARS-CoV-2 infection15,17. However, a few previous studies which could analyse non-COVID-19 related hospitalizations for acute asthma and other respiratory diseases reported significant reductions, which have been partly attributed to a reduced exposure to air pollutants and other respiratory infections during the COVID-19 lockdowns23,26,28,30.
Among other chronic conditions, we reported a reduction by 30% in hospitalizations among patients with chronic renal failure. This is consistent with findings from a recent meta-analysis indicating that the COVID-19 pandemic led to reductions in access to kidney transplantation, dialysis, and in-person nephrology care, with an overall a 50% reduction in nephrology-related hospital admissions reported in four studies on a total of 4873 patients35.
There are two major explanations of the observed decrease in hospitalizations for many chronic patients, the first linked the reduction of health service offer, due to the restrictions in hospital services, with the reallocation of several hospital departments and personnel to the care of COVID-19 patients and the consequent cancellations of elective, routine, and non-urgent treatments, and the second related to the limited patients’ access, due to the patient’s fear of SARS-CoV-2 infection which kept them away from hospital, as well as from other health care services26,31,35. It is also possible that underlining trends in hospitalization explain some of our findings, although we did not find any meaningful trends in hospitalizations for chronic patients over the four calendar years considered.
Our study has the strength to be a large real-world, population-based study conducted on all older adults with chronic diseases in the study areas (including over 2.3 million older adults and 400,000 chronic patients), while most previous studies were conducted in single or few centres, and were focused on specific conditions. Most previous studies, moreover, were conducted on acute conditions, while very few analysed accesses to hospital among chronic patients. Furthermore, we could compare two populations from northern Italy—both particularly hit by COVID-19 during the first and second waves—which provided extremely consistent results. Among the major limitations of the study, there is the fact that we could not distinguish COVID-19-related hospitalizations, since at the time of our analyses we had no information on hospitalizations for this cause. Considering that hospitalizations primarily due to COVID-19 have subsequently been estimated to be approximatively 7% in our population, the reductions in hospital access during the 2020 COVID-19 pandemic could have been even larger. Moreover, we could not analyse other outcomes, as cause-specific mortality rates, because no data on cause of death were available in our data.
In conclusion, the present study provides evidence of a significantly reduced hospital care for older adults with chronic conditions during the COVID-19 pandemic. This was noted in particular for those with cancer and necessitating surgery, suggesting that those patients may not have been receiving adequate health services and treatments since the pandemic began, with likely detrimental health consequences on the medium and long run. However, the declines in hospitalization rates were more modest than those observed in non-chronic patients, indicating that during the outbreaks of COVID-19 in 2020 there some attempt to foster the cure for these more vulnerable individuals.
Methods
We conducted an observational study on all older adults with chronic conditions identified from the electronic health databases of ATS (Agenzia per la Tutela della Salute) Brianza and ATS Bergamo, Lombardy, Italy. Each ATS has a central role in programming, paying, and evaluating health services to approximately 2.3 million residents, including about 400,000 individuals with chronic conditions.
Health data available in the two ATS include the following information for all residents: demographic data (age, sex, area of residence, and vital status); exemptions from payment for specific diseases, including chronic ones; and detailed discharge information from public and private accredited hospitals (date of admission and discharge, main diagnosis and five secondary diagnoses, date and type of intervention, and costs associated with hospitalization on the basis of the weight of Diagnosis-Related Group—DRG—system)36,37. The information available for each individual in the various databases are identified by the same unique code and were subsequently linked with a deterministic process in order to identify individuals of interest and their related information.
The study population consisted of all adults aged 65 or more living in the two areas covered by ATS Brianza and ATS Bergamo over the years between 2017 and 2020, and who had at least one chronic disease. For all inhabitants in Lombardy, it was searched evidence for chronic conditions on the basis of data from various databases of the Health Informative System. On a hierarchical basis, individuals were classified according to their primary chronic condition using algorithms defined by the Lombardy region for the year 201738. The conditions were then classified into nine major disease categories, i.e., diabetes mellitus, respiratory diseases, tumours, cardiovascular diseases, renal diseases, liver diseases, rheumatoid arthritis, digestive diseases, and thyroid diseases. Tumours were also considered in three into separate group, i.e., active (less than 1 year since diagnosis), in follow-up (1–5 years), and in remission (more than 5 years).
The study was conducted in accordance with the Declaration of Helsinki and its protocol was approved by the Ethical Committees of the two ATS (Comitato Etico Brianza, Protocol N. 3599, and Comitato Etico della Provincia di Bergamo, Protocol N. 3599 69/21). The Ethical Committees waived the requirement for informed consent for the collection, analysis, and publication of the retrospectively and anonymized data used in this study. Personnel of the two ATS had the had the appropriate permissions to access patient data from the databases.
As indicators of access to health care, we considered numbers and rates of hospitalization; these were provided overall, by hospital regimen (ordinary, day-hospital), type of DRG (medical, surgical), level of complexity (low, 1 comorbidity; medium, 2–3 comorbidities; high, ≥ 3 comorbidities), individuals’ chronic conditions, and Major Diagnostic Category (MDC)37. Rates were computed as the ratio between number of hospital discharges over 1 year divided by the referent population multiplied by 1000. Numbers and rates of hospitalization are presented for the average period 2017–2019 and the year 2020. Differences in hospitalization between the two periods were compared using the rate ratios (RRs) and their corresponding 95% confidence intervals (CIs). For a comparative purpose, hospitalizations among non-chronic individuals were also assessed. A yearly ranking system has been defined based on the MDC prevalence for individuals with diabetes (with and without complications) and for individuals with active tumours39.
Data analyses were performed using the software SAS, version 9.4 (SAS Institute, North Carolina, USA) and Stata, version 17 (StataCorp, College Station, Texas 77845, USA).
Supplementary Information
Author contributions
C.B. and S.G. conceptualized the study. L.C.D.O. and A.Z. contributed in the study conceptualization. C.B. drafted the manuscript. M.R., R.C., L.P., and M.S. performed data extraction and statistical analyses. A.A., L.I., S.G., A.O., and D.S. contributed in reviewing and finalizing the paper. All authors approved the final version of the manuscript.
Funding
The work was supported by a research grant of the DG-Welfare of The Lombardy region (Call: Progetti di Ricerca in Ambito Sanitario Connessi all’Emergenza COVID 19; DGR n. XI/3017) and by a grant of the AXA (AXA Research Fund—Call for Proposals Covid-19).
Data availability
Data that support the findings of this study and materials are available from the corresponding author upon request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Cristina Bosetti, Email: cristina.bosetti@marionegri.it.
Lost in Lombardia Project Investigators:
Cristina Bosetti, Silvano Gallus, Carlotta Micaela Jarach, Alessandra Lugo, Chiara Stival, Andrea Amerio, Mario Amore, Gianluca Serafini, Roberto De Sena, Simone Ghislandi, David Stuckler, Yuxi Wang, Marialaura Bonaccio, Francesco Gianfagna, Licia Iacoviello, Giansanto Mosconi, Anna Odone, Carlo Signorelli, Giacomo Vigezzi, Luca Cavalieri d’Oro, Luca Paroni, Marco Sala, Magda Rognoni, Roberta Ciampichini, and Alberto Zucchi
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-17941-2.
References
- 1.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA. 2020;323:1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 4.Remuzzi A, Remuzzi G. COVID-19 and Italy: What next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romagnani P, et al. The COVID-19 infection: Lessons from the Italian experience. J. Public Health Policy. 2020;41:238–244. doi: 10.1057/s41271-020-00229-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Presidenza del Consiglio dei Ministri. DPCM 9 March 2020. https://www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg
- 7.Paroni L, et al. The traffic light approach: Indicators and algorithms to identify Covid-19 epidemic risk across Italian regions. Front. Public Health. 2021;9:650243. doi: 10.3389/fpubh.2021.650243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bontempi E. The Europe second wave of COVID-19 infection and the Italy “strange” situation. Environ. Res. 2021;193:110476. doi: 10.1016/j.envres.2020.110476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19—Implications for the health care system. N. Engl. J. Med. 2020;383:1483–1488. doi: 10.1056/NEJMsb2021088. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. COVID-19 continues to disrupt essential health services in 90% of countries. https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries
- 11.Moynihan R, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open. 2021;11:e045343. doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmer K, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: Consequences for healthy ageing. Aging Clin. Exp. Res. 2020;32:1189–1194. doi: 10.1007/s40520-020-01601-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matenge S, et al. Ensuring the continuation of routine primary care during the COVID-19 pandemic: A review of the international literature. Fam. Pract. 2021 doi: 10.1093/fampra/cmab115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 15.Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: A systematic review and meta-analysis. Arch. Acad. Emerg. Med. 2020;8:e35. [PMC free article] [PubMed] [Google Scholar]
- 16.Signorelli C, Odone A. Age-specific COVID-19 case-fatality rate: No evidence of changes over time. Int. J. Public Health. 2020;65:1435–1436. doi: 10.1007/s00038-020-01486-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alyammahi SK, et al. The dynamic association between COVID-19 and chronic disorders: An updated insight into prevalence, mechanisms and therapeutic modalities. Infect. Genet. Evol. 2021;87:104647. doi: 10.1016/j.meegid.2020.104647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chudasama YV, et al. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab. Syndr. 2020;14:965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. COVID-19 significantly impacts health services for noncommunicable diseases. https://www.who.int/news-room/detail/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases
- 20.Santi L, et al. Non-COVID-19 patients in times of pandemic: Emergency department visits, hospitalizations and cause-specific mortality in Northern Italy. PLoS One. 2021;16:e0248995. doi: 10.1371/journal.pone.0248995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campo G, et al. In- and out-of-hospital mortality for myocardial infarction during the first wave of the COVID-19 pandemic in Emilia-Romagna, Italy: A population-based observational study. Lancet Reg. Health Eur. 2021;3:100055. doi: 10.1016/j.lanepe.2021.100055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrara G, et al. Cancer diagnostic delay in Northern and Central Italy during the 2020 lockdown due to the coronavirus disease 2019 pandemic. Am. J. Clin. Pathol. 2021;155:64–68. doi: 10.1093/ajcp/aqaa177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blecker S, et al. Hospitalizations for chronic disease and acute conditions in the time of COVID-19. JAMA Intern. Med. 2021;181:269–271. doi: 10.1001/jamainternmed.2020.3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kondilis E, Tarantilis F, Benos A. Essential public healthcare services utilization and excess non-COVID-19 mortality in Greece. Public Health. 2021;198:85–88. doi: 10.1016/j.puhe.2021.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Filippo O, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N. Engl. J. Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Papafaklis MI, et al. “Missing” acute coronary syndrome hospitalizations during the COVID-19 era in Greece: Medical care avoidance combined with a true reduction in incidence? Clin. Cardiol. 2020;43:1142–1149. doi: 10.1002/clc.23424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mesnier J, et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: A registry study. Lancet Public Health. 2020;5:e536–e542. doi: 10.1016/S2468-2667(20)30188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rennert-May E, et al. The impact of COVID-19 on hospital admissions and emergency department visits: A population-based study. PLoS One. 2021;16:e0252441. doi: 10.1371/journal.pone.0252441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhambhvani HP, Rodrigues AJ, Yu JS, Carr JB, II, HaydenGephart M. Hospital volumes of 5 medical emergencies in the COVID-19 pandemic in 2 US medical centers. JAMA Intern. Med. 2021;181:272–274. doi: 10.1001/jamainternmed.2020.3982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bodilsen J, et al. Hospital admission and mortality rates for non-covid diseases in Denmark during covid-19 pandemic: Nationwide population based cohort study. BMJ. 2021;373:n1135. doi: 10.1136/bmj.n1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kendzerska T, et al. The effects of the health system response to the COVID-19 pandemic on chronic disease management: A narrative review. Risk Manag. Healthc. Policy. 2021;14:575–584. doi: 10.2147/RMHP.S293471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Odone A, et al. The runaway science: A bibliometric analysis of the COVID-19 scientific literature. Acta Biomed. 2020;91:34–39. doi: 10.23750/abm.v91i9-S.10121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Quteimat OM, Amer AM. The impact of the COVID-19 pandemic on cancer patients. Am. J. Clin. Oncol. 2020;43:452–455. doi: 10.1097/COC.0000000000000712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sud A, et al. Collateral damage: The impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann. Oncol. 2020;31:1065–1074. doi: 10.1016/j.annonc.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deng D, Liang A, Chui JN, Wong G, Cooper TE. The COVID-19 pandemic and access to health care in people with chronic kidney disease: A systematic review and meta-analysis. Nephrology (Carlton) 2021 doi: 10.1111/nep.14016. [DOI] [PubMed] [Google Scholar]
- 36.Tulchinsky, T. & Varavikova, E. The New Public Health 3rd edn, 771–819. https://www.sciencedirect.com/topics/medicine-and-dentistry/diagnosis-related-group
- 37.ICD-10 MS-DRG V38.0. https://icdlist.com/icd-10/drg/
- 38.Regione Lombardia. D.r.g. 30 Gennaio 2017—n. X/6164—Governo della domanda: avvio della presa in carico di pazienti cronici e fragili. https://www.regione.lombardia.it/wps/wcm/connect/f2ec5853-447c-4fc2-b4d4-e36d651ebbfb/delibera+6164_300117.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-f2ec5853-447c-4fc2-b4d4-e36d651ebbfb-m3lXCz3
- 39.Harvey L. Neiman Health Policy Institute. ICE-T Inpatient Cost Evaluation Tool. https://www.neimanhpi.org/ice-t/ranking-drgs/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data that support the findings of this study and materials are available from the corresponding author upon request.