Abstract
Background
The atherogenic index of plasma (AIP) is a predictor for cardiovascular diseases (CVD), while hyperuricemia is an independent risk factor for a variety of CVD. Apolipoprotein AI has been found to be a protective factor for CVD. However, the role of APO AI in the association between plasma uric acid and AIP among healthy Chinese people needs to be further explored.
Aims
To evaluate the relationship between blood uric acid and AIP level in healthy Chinese people. To evaluate the relationship between blood uric acid and Apolipoprotein AI in healthy Chinese people.
Method
A total of 3501 normal and healthy subjects who had physical examinations were divided into the hyperuricemia (HUA) group and the normouricemia (NUA) group.
Result
The AIP of HUA group was significantly higher than that of NUA group [0.17±0.30 vs. −0.08±0.29]. Apo AI (1.33 ± 0.21 vs. 1.47 ± 0.26 g/l) and HDL-c (1.12 ± 0.27 vs. 1.36 ± 0.33 mmol/l) were significantly lower in the HUA group than in the NUA group. LDL-C (2.81 ± 0.77 vs. 2.69 ± 0.73 mmol/l), Apo B (0.96 ± 0.20 vs. 0.89 ± 0.20 g/l), FBG (5.48 ± 0.48 vs. 5.36 ± 0.48 mmol/l) and HOMA-IR [2.75 (1.92–3.91) vs. 2.18 (1.50–3.12)] was significantly higher in HAU group than the NUA group. Increases in plasma UA were associated with increases in AIP (β = 0.307, p < 0.01) and decreases in Apo AI (β = − 0.236, p < 0.01).
Conclusion
Hyperuricemia is an independent risk factor for high AIP level. Inhibition of Apolipoprotein AI may be one of the mechanisms of UA which is involved in the progression of cardiovascular disease.
Keywords: Hyperuricemia, AIP, Apo AI
Introduction
A large number of studies have shown that hyperuricemia is closely related to cardiovascular disease. It is known that hyperuricemia is associated with a significant increased risk of hypertension, coronary heart disease (CHD), and congestive heart failure (CHF) [1–3]. Additionally, another study found that serum uric acid is an independent predictor for cardiovascular disease-related death, including chronic, acute, and subacute forms of CHF, CHD and stroke [4, 5]. These are all related to the deposition of urate crystals in the vascular endothelium and the dissolution of urate promotes lipid peroxidation, which increase oxidative stress and inflammatory response and lead to vascular endothelial dysfunction [6, 7].
Dyslipidemia is also an independent risk factor for cardiovascular disease. High-density lipoprotein cholesterol (HDL-C) is a cardiovascular protective factor [8]. Apolipoprotein(apo)A-I is the principal protein of HDL-C [9]. Previous studies found that hyperuricemia is closely related to HDL-C and Apo AI. Hyperuricemia is often accompanied by abnormal lipid metabolism, including low HDL-C level [10]. Moreover, it was found that the ratio of apolipoprotein-B to AI are strongly associated with serum uric acid levels in US people [10].
AIP was calculated as lg (TG (mmol)/L/HDL (mmol/L)), which was found to be a powerful indicator of CVD among different population [11–14]. Another study in Indonesia showed that low AIP predicted a decrease in all-cause mortality of hospitalized patients with acute myocardial infarction [15]. It has been proved that AIP is associated with smaller LDL particles [16] and increased esterification rate of HDL [17]. Recently, several studies have shown that AIP is related to other metabolic indexes besides Lipid metabolism. Akbas et al. [18] reported that plasma UA was independently positively correlated with AIP in patients with diabetes mellitus. However, the relationship between apolipoprotein, uric acid and AIP has not been confirmed in a large number of Chinese people.
Furthermore, although there are several studies which focus on the relationship between uric acid and lipid metabolism, the participants with hyperuricemia in most of the previous studies had comorbidities such as diabetes, hypertension, or cardiovascular diseases. There may be mutual interference between the diseases, which therefore makes clarifying the simple relationships a difficult task. In the present study, we examined the relationship between hyperuricemia and Apo AI and AIP in normal and healthy Chinese subjects.
Methods
Design and participants
A total of 3501 healthy individuals aged over 20 years and under 80 years were enrolled in this study. All participants had undergone a routine physical examination at Beijing Chao-yang Hospital Affiliated to Capital Medical University from March 2012 to October 2014. Individuals with hypertension, diabetes, pre-diabetes, cancer, liver or renal function impairment, coronary artery disease, or systemic inflammatory disease were excluded. Participants who took lipid-lowering or uric-acid-lowering agents were also excluded. HUA was defined by the plasma UA level ≥ 420 mol/L in men and ≥ 360 mol/L in women [19]. We divided the participants into two groups: the NUA group (subjects without hyperuricemia) and the HUA group (subjects with hyperuricemia). The protocol of the study was approved by the Ethics Committee of Beijing Chao-yang Hospital Affiliated to Capital Medical University.
Physical and biochemical measurement
Height, weight, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were measured. BMI was calculated as weight (kg)/height (m)2.
Blood samples were collected from the vein after a 12-h fasting period. Each sample from participants was stored at − 80 °C. HDL-C and low-density lipoprotein cholesterol (LDL-c) were measured using the direct assay on an autoanalyzer (Hitachi 7170). The levels of Triglyceride (TG), total cholesterol (TC) and Serum uric acid (UA) were measured by glycerol lipase oxidase reaction, enzymatic cholesterol oxidase method on a Hitachi 7170 autoanalyzer and enzymatic assay, respectively. Immune turbidimetry was utilized to analyze the immune turbidimetry ApoAI and apolipoprotein B (Apo B). The concentration of fasting insulin (FINS) and fasting blood glucose (FBG) was measured at the central chemistry laboratory in Beijing Chao-yang Hospital.
AIP was calculated as lg (TG (mmol)/L/HDL (mmol/L)).
Homeostasis model assessment of β-cell function (HOMA-β) was calculated as 20*FIN/ (FBG-3.5).
Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as FINS (μIU/mL) * FBG (mmol/L)/22.5.
Statistical methods
All statistical analyses in this study were performed using SPSS version 21.0. Continuous variables with normal distributions were shown as a mean ± standard deviation (SD), while continuous variables with skewed distributions were expressed as a median with upper and lower quartiles. The Student t-test and non-parametric test were applied to analyze the differences between the groups. The continual variables of abnormal distribution were expressed as the median of upper and lower quartiles and analyzed by a nonparametric test. Discontinuous variables were given as percentages and analyzed by chi-square test. Pearson’s correlation analysis was performed to measure the linear correlation between the variables that was normally distributed. Linear regression and logistic regression analysis were elaborated to further explore the association between blood uric acid and Apolipoprotein AI level or other metabolism indexes. Statistical significance was defined as p < 0.05.
Results
Clinical characteristics of the HUA and NUA group
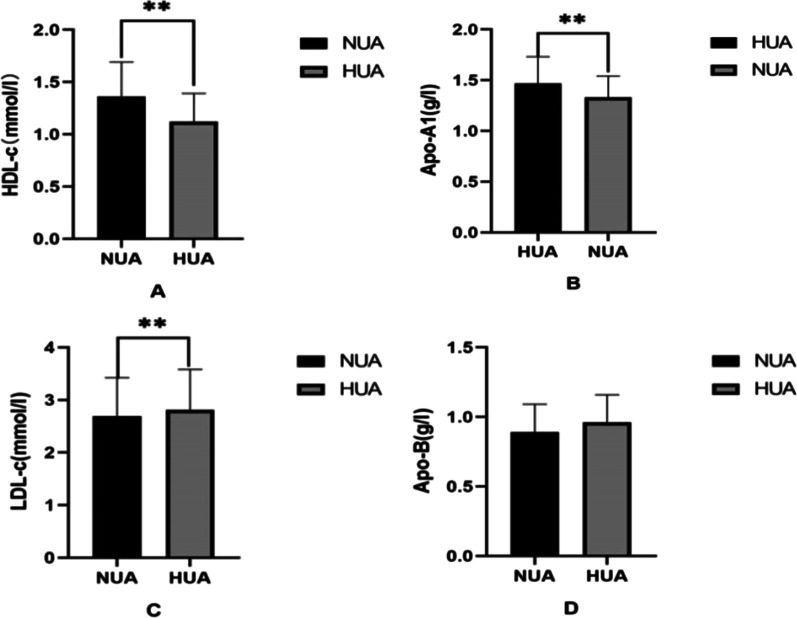
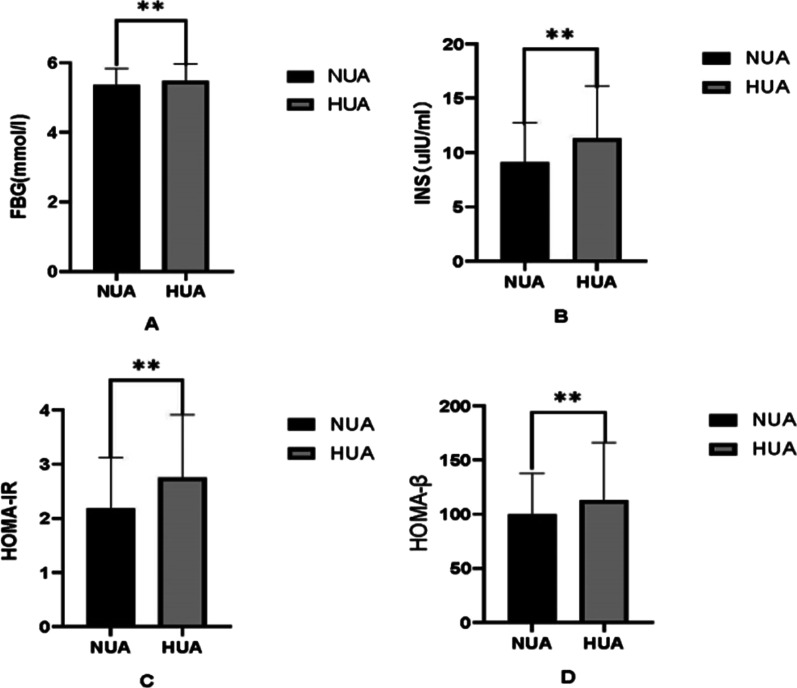
The clinical characteristics of HUA group and NUA group are shown in Table 1, from which it can be seen that there were 2868 subjects in NUA group and 633 subjects in HUA group. The proportion of males in the HUA group was significantly higher than that in the NUA group. BMI, SBP and DBP increased significantly in the HUA groups, more than the NUA groups (p<0.01). The level of AIP was found to be significantly higher in the HUA group than in the NUA group. For lipid metabolism comparison, TG, LDL-c and Apo B were significantly increased in HUA participants, and HDL-C and Apo AI were lower than those in the NUA group (p < 0.01) (Fig. 1). Furthermore, FBG and FIN concentrations were significantly higher in the HUA group compared with the HUA group due to higher HOMA-β and HOMA-IR (p < 0.01) (Fig. 2). AIP was found at higher values in the HUA group than the NUA group.
Table 1.
Comparison of Characteristics between NUA and HUA
| Parameters | NUA group (n = 2868) | HUA group (n = 633) | p Value |
|---|---|---|---|
| Age, y | 45.2 ± 11.6 | 41.5 ± 11.9 | < 0.01 |
| Gender, male% | 41.00 | 95.10 | < 0.01 |
| BMI, kg/m2 | 23.49 ± 2.85 | 25.42 ± 2.47 | < 0.01 |
| SBP, mmHg | 118.4 ± 11.9 | 122.7 ± 10.6 | < 0.01 |
| DBP, mmHg | 71.5 ± 8.8 | 75.0 ± 8.5 | < 0.01 |
| TG, mmol/l | 1.05 (0.76–1.51) | 1.57 (1.12–2.32) | < 0.01 |
| LDL-C, mmol/l | 2.69 ± 0.73 | 2.81 ± 0.77 | < 0.01 |
| HDL-C, mmol/l | 1.36 ± 0.33 | 1.12 ± 0.27 | < 0.01 |
| FBG, mmol/l | 5.36 ± 0.48 | 5.48 ± 0.48 | < 0.01 |
| FINS, uIU/ml | 9.11 (6.41–12.74) | 11.31 (8.01–16.12) | < 0.01 |
| UA, umol/l | 300.88 ± 64.71 | 474.13 ± 55.47 | < 0.01 |
| CRE, umol/l | 61.73 ± 12.62 | 76.65 ± 10.82 | < 0.01 |
| AIP | − 0.08 ± 0.29 | 0.17 ± 0.30 | < 0.01 |
BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, UA uric acid, TG triglyceride, HDL-c high-density lipoprotein cholesterol, LDL-c low-density lipoprotein cholesterol, FBG fasting blood glucose, FINS fasting insulin, CRE creatinine, AIP atherogenic index of plasma
Fig. 1.
Comparison of lipid metabolism indices between HUA and NUA group. Bar graph of Lipid metabolism indices (A HDL-c; B Apo AI; C LDL-c; D Apo-B) mean value with SD intervals between NUA and HUA groups. *p < 0.05, **p < 0.01. UA uric acid, HDL-c high-density lipoprotein cholesterol, Apo AI apolipoprotein A1, LDL-c low-density lipoprotein cholesterol, Apo B apolipoprotein B
Fig. 2.
Comparison of glucose metabolism indices between HUA and NUA group. Bar graph of glucose metabolism indices (A FBG; B INS; C HOMA-IR; D HOMA-β) mean value with SD intervals or median with quartiles between NUA and HUA groups. *p < 0.05, **p < 0.01. FBG Fasting blood glucose, INS insulin, HOMA-IR homeostasis model assessment of insulin resistance, HOMA-β homeostasis model assessment of β-cell function
Correlation between UA and AIP
UA was positively correlated with AIP, after applying linear correlation analysis (r = 0.439, p < 0.01) (Fig. 3). To further examine the correlation between UA and AIP, multiple linear regression analysis was performed. After adjustment for age, BMI, SBP, and FBG, there was still a significant relationship between the increase in UA and the increase in AIP value (β = 0.307, p < 0.01).
Fig. 3.
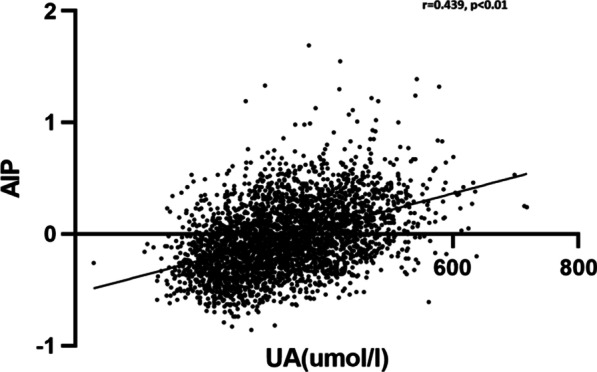
The correlation between plasma UA and AIP. Correlation analysis was used to prove the linear relationship between plasma UA and AIP. Plasma UA was positively correlated with AIP
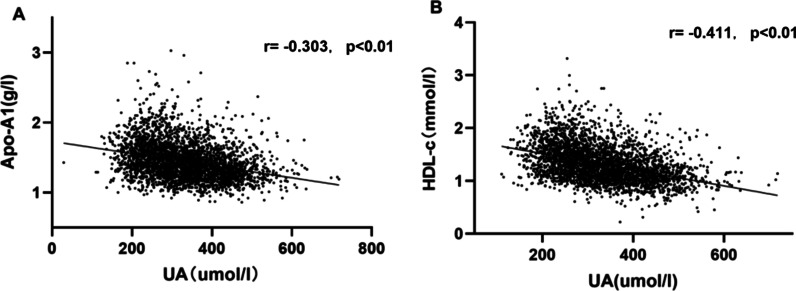
Correlation between UA and Apo AI or other metabolic indexes
UA was inversely correlated with Apo AI and HDL-c, after applying linear correlation analysis (Apo AI: r = −0.303, p < 0.01; HDL-c: r = −0.411, p < 0.01) (Figure 4). Multiple linear regression analysis was used to further prove the correlation between UA and other metabolic indexes. After adjusting for age, BMI and SBP, FBG was positively associated with UA (r = 0.046, p < 0.05) and Apo AI was inversely associated with UA significantly (r = −0.236, p < 0.01). Also, it was found that HDL-C was inversely associated with UA (β = −0.289, p < 0.01)
Fig. 4.
Correlation between plasma UA and the levels of Apo AI and HDL-c. Correlation analysis was used to prove the linear relationship between plasma UA and the levels of Apo AI (A) and HDL-c (B). Plasma UA was negatively correlated with Apo AI and HDL-C
To study whether HDL participates in the relationship between Apo AI and UA, another multivariate logic analysis model was set up. UA was used as dependent variable. Age, Gender, BMI, SBP, AIP, FBG, CRE, Apo AI and Apo B were used as independent variables. In this model, AIP was positively associated with UA [odds ratio (OR): 5.449; 95% confidence interval (CI): 3.408–8.714)]. Apo AI has no significant correlation with UA (p > 0.05) (Table2).
Table 2.
Multivariate logistic regression analyzed factors associated with UA
| OR | 95%CI | p Value | |
|---|---|---|---|
| Age | 0.967 | 0.956–0.978 | < 0.001 |
| SBP | 1.006 | 0.995–1.017 | 0.298 |
| BMI | 1.095 | 1.042–1.150 | < 0.001 |
| Male | 6.232 | 3.841–10.112 | < 0.001 |
| Apo B | 3.074 | 1.605–5.888 | 0.001 |
| Apo AI | 0.980 | 0.538–1.785 | 0.946 |
| FBG | 0.984 | 0.769–1.259 | 0.899 |
| CRE | 1.056 | 1.043–1.069 | < 0.001 |
| AIP | 5.449 | 3.408–8.714 | < 0.001 |
Compared to non hyperuricemia. Variables included in the model were Age, male, BMI, SBP, AIP, FBG, CRE, Apo AI and Apo B. The Pseudo R2 (McFadden R2) was 0.316. The p value of likelihood ratio test was < 0.01
BMI body mass index, FBG fasting blood glucose, SBP systolic blood pressure, CRE creatinine, AIP atherogenic index of plasma, Apo AI apolipoprotein A1, cholesterol, Apo B apolipoprotein B, FBG fasting blood glucose
Discussion
Presently, many studies have found that HUA is closely related to cardiovascular disease. For example, it can affect vascular endothelium, increase the risk of hypertension [20, 21], heart failure [22], increase the risk of cardiovascular disease, including coronary heart disease [23], and myocardial infarction [5, 24]. Although many studies on the mechanism partly explain the relationship between UA and cardiovascular disease, it is not completely clear. Moreover, hyperuricemia is often accompanied by other diseases. At present, among a large number of people engaged in the research on uric acid and metabolic or cardiovascular diseases, there are often other metabolic or cardiovascular comorbidities or even metabolic syndrome. It is difficult to purely study the relationship between UA and specific risk factors, or protective factors of cardiovascular disease. This study is characterized by the fact that it is conducted in a healthy population without diabetes, hypertension, or metabolic syndrome, and to clarify the relationship between UA and AIP and Apo AI. The result plays a certain role in the occurrence and development mechanism of UA in cardiovascular disease.
The present study explored the association between UA and Apo AI in healthy people without diabetes, hypertension or metabolic syndrome. Apo AI is one of the cardiovascular protective factors [25]. We found that the Apo AI and HDL-C in the HUA group were lower than that in the NUA group. In further analysis, HUA was found to be independently associated with decreased plasma Apolipoprotein AI and HDL-C. The results may suggest that hyperuricemia may promote the progress of the cardiovascular disease by reducing the levels of Apo AI and HDL-C. Other previous studies are similar to our study [26]. Kuwabara et al. [21] conducted a prospective study on Japanese patients with hyperuricemia but without typical symptoms and other complications. The study found that after a five-year follow-up the incidence of cardiovascular related metabolic disorders, such as abnormal lipid metabolism and hypertension, in the asymptomatic HUA group was significantly higher than that in the normal UA group. A sub-analysis of the NHANES III study also found that triglycerides to HDL-C and Apo-B to Apo AI were linearly positively associated with uric acid levels. However, in contrast with our study, the participants included patients with diabetes, hypertension and other complications, and no significant correlation between Apo AI and UA after adjusting for related factors [10].
Presently, the mechanism of the interaction between uric acid with HDL-C and Apo AI is not completely clear. Animal studies have found that high uric acid can reduce the level of phospholipids of HDL subclasses. Also induce the increase of fractional catabolic rate (FCR) significantly, resulting in decreased HDL-C and Apo AI levels [27, 28]. Other studies have found that high UA is also closely related to small and dense HDL-C. At the same time, HDL-C volume is negatively correlated with fibrinogen concentration [29], and HUA was negatively correlated with a large HDL-C level [23], which may present a mechanism that contributes to arteriosclerosis. There are different relationships between HUA and different subclasses of HDL-C [30], HUA and HDL2, which are associated with alcohol consumption [31], waist circumference, smoking, and exercise had a negative correlation. However, HUA and HDL3 which only associated with alcohol consumption had a positive correlation. Furthermore, most studies only studied the relationship between HDL and UA; the mechanism of the interaction between Apo AI and UA needs to be further explored.
Additionally, results from this study suggested that other metabolic parameters, including FBG and HOMA-IR, were associated with UA rather than lipoprotein. Comparable with this study, many studies have found that HUA is closely related to insulin resistance and hyperglycemia [32–34]. Long term follow-up studies confirmed that hyperuricemia is an indicator for predicting abnormal glucose metabolism. Krishnan et al. [35] conducted a 15-year follow-up study on young people without diabetes. They found that the risk of developing diabetes, insulin resistance (IR) and prediabetes in the HUA group was significantly higher than that in the non-hyperuricemia group. A 5.3-year follow-up study of the Chinese population also confirmed that HUA and is closely related to the development of hypertension [36]. The mechanisms are complex; uric acid can reduce IR by promoting mitochondrial oxidative stress and NO bioavailability [37, 38]. However, hypouricemic drugs such as Allopurinol can reduce uric acid, improve insulin resistance, and systemic inflammation in patients with hyperuricemia [39]. Adversely, IR can induce hyperuricemia by inhibiting uric acid excretion through increasing renal tubular sodium reabsorption [40].
Compared to other lipid metabolism indexes, AIP was proven as the strongest predictor for coronary artery disease [11]. A recent study has found that AIP is independently related to the rapid progress of plaque in coronary artery of patients with CAD, thus affecting the progress rate of CAD [41]. Our result showed that UA was positively correlated with AIP in multiple linear regression analysis, which was similar to the research in the population of Northeast China conducted by Chang et al. [42]. However, the research included diabetes, cardiovascular disease and other complications of the crowd, and did not measure or analyze lipoproteins level in detail. Another study in India found AIP was positively associated with serum UA, TG, and HDL-C [43]. Which differed from the present study, females were not incorporated and APO AI was not measured. In the current study, the relationships among uric acid and AIP and Apo AI were analyzed. We hypothesize that decreased levels of Apo AI and HDL is one of the mechanisms involved in the deterioration of AIP caused by hyperuricemia.
The limitations of our study include that fact that this is a cross-sectional study, and it is impossible to determine the causal relationship. A prospective study can be carried out next to further explore the relationship between UA, Apo AI and cardiovascular disease. This study is calculated upon the data of a small number of subjects who received health examinations, which had selection bias, and larger scale studies will be carried out in the future.
Conclusion
In conclusion, hyperuricemia was an independent risk for increased AIP levels and associated with decreased plasma Apolipoprotein AI independently. Inhibition of Apolipoprotein AI may be one of the mechanisms of UA involved in the progression of cardiovascular disease.
Acknowledgements
Not applicable.
Author contributions
JL and GW are responsible for the design of the study. YA, XD and XC are responsible for data collection. YD and JL are responsible for data analysis and drafting of the manuscript. Both authors read and approved the final manuscript.
Funding
This work was supported by grants from the Beijing Talents foundation [2018-12] and DMRFP-I-05 from SHMHDF to JL. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The protocol of this study was approved by the Ethics Committee of the Beijing Chao-yang Hospital Affiliated to Capital Medical University. The authors confirmed that all methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects.
Consent for publication
Participants were informed of data sharing with their name and identity hidden per consent.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Anesthesiology NJSO. Serum uric acid and cardiovascular mortality: the NHANES I epidemiologic follow-up study, 1971–1992. Surv Anesthesiol. 2001;45(2):121–122. doi: 10.1097/00132586-200104000-00057. [DOI] [Google Scholar]
- 2.Holme I, et al. Uric acid and risk of myocardial infarction, stroke and congestive heart failure in 417,734 men and women in the Apolipoprotein MOrtality RISk study (AMORIS) J Intern Med. 2009;266(6):558–570. doi: 10.1111/j.1365-2796.2009.02133.x. [DOI] [PubMed] [Google Scholar]
- 3.Culleton BF, et al. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med. 1999;131:7–13. doi: 10.7326/0003-4819-131-1-199907060-00003. [DOI] [PubMed] [Google Scholar]
- 4.Strasak AM, et al. Serum uric acid is an independent predictor for all major forms of cardiovascular death in 28,613 elderly women: a prospective 21-year follow-up study. Int J Cardiol. 2008;125(2):232–239. doi: 10.1016/j.ijcard.2007.11.094. [DOI] [PubMed] [Google Scholar]
- 5.Casiglia E, et al. Serum uric acid and fatal myocardial infarction: detection of prognostic cut-off values. J Hypertens. 2019;38(3):1. doi: 10.1097/HJH.0000000000002287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gjin NJCCA. Uric acid and cardiovascular disease. Clin Chim Acta. 2018;484:150. doi: 10.1016/j.cca.2018.05.046. [DOI] [PubMed] [Google Scholar]
- 7.Borghi C, et al. Serum uric acid and the risk of cardiovascular and renal disease. J Hypertens. 2015;33(9):1729–1741. doi: 10.1097/HJH.0000000000000701. [DOI] [PubMed] [Google Scholar]
- 8.Franceschini G. Epidemiologic evidence for high-density lipoprotein cholesterol as a risk factor for coronary artery disease. Am J Cardiol. 2001;88(12A):9–13. doi: 10.1016/S0002-9149(01)02146-4. [DOI] [PubMed] [Google Scholar]
- 9.Yokoyama S. Assembly of high-density lipoprotein. Arterioscler Thromb Vasc Biol. 2006;26(1):20–27. doi: 10.1161/01.ATV.0000195789.39418.e8. [DOI] [PubMed] [Google Scholar]
- 10.Peng T-C, et al. Relationship between hyperuricemia and lipid profiles in US adults. Biomed Res Int. 2015;2015:1–7. doi: 10.1155/2015/127596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cai G, et al. The atherogenic index of plasma is a strong and independent predictor for coronary artery disease in the Chinese Han population. Medicine. 2017;96(37):e8058. doi: 10.1097/MD.0000000000008058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nwagha UI, et al. Atherogenic index of plasma as useful predictor of cardiovascular risk among postmenopausal women in Enugu. Nigeria. 2010;10(3):248–252. [PMC free article] [PubMed] [Google Scholar]
- 13.Niroumand S, et al. Atherogenic Index of Plasma (AIP): a marker of cardiovascular disease. Med J Islam Repub Iran. 2015;29(1):240–240. [PMC free article] [PubMed] [Google Scholar]
- 14.Ji SN, et al. Association between atherogenic index of plasma and coronary artery calcification progression in Korean adults. Lipids Health Dis. 2020;19(1):1–7. doi: 10.1186/s12944-019-1182-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hartopo AB, Arso IA, Setianto BY. Low plasma atherogenic index associated with poor prognosis in hospitalized patients with acute myocardial infarction. Acta Med Indones. 2016;48(2):106. [PubMed] [Google Scholar]
- 16.Onat A, et al. "Atherogenic index of plasma" (log10 triglyceride/high-density lipoproteincholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol. 2010;4(2):89–98. doi: 10.1016/j.jacl.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Dobiásová M, et al. Cholesterol esterification and atherogenic index of plasma correlate with lipoprotein size and findings on coronary angiography. J Lipid Res. 2011;52(3):566–571. doi: 10.1194/jlr.P011668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akbas EM, et al. Association of uric acid, Atherogenic index of plasma and albuminuria in diabetes mellitus. Int J Clin Exp Med. 2014;7(12):5737. [PMC free article] [PubMed] [Google Scholar]
- 19.Vekic J, et al. High serum uric acid and low-grade inflammation are associated with smaller LDL and HDL particles. Atherosclerosis. 2009;203:236–242. doi: 10.1016/j.atherosclerosis.2008.05.047. [DOI] [PubMed] [Google Scholar]
- 20.Tsan Y, et al. Uric acid concentration as a risk marker for blood pressure progression and incident hypertension: a Chinese cohort study. Metabolism. 2012;61:1747–1755. doi: 10.1016/j.metabol.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Kuwabara M, et al. Asymptomatic hyperuricemia without comorbidities predicts cardiometabolic diseases. Hypertension. 2017;69(6):1036–1044. doi: 10.1161/HYPERTENSIONAHA.116.08998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spieker LE, et al. The management of hyperuricemia and gout in patients with heart failure. Eur J Heart Fail. 2014;4(4):403–410. doi: 10.1016/S1388-9842(02)00086-7. [DOI] [PubMed] [Google Scholar]
- 23.Yan Z, et al. Lipoprotein subfractions partly mediate the association between serum uric acid and coronary artery disease. Clin Chim Acta. 2015;441:109–114. doi: 10.1016/j.cca.2014.12.030. [DOI] [PubMed] [Google Scholar]
- 24.Ndrepepa G, et al. Uric acid and prognosis in angiography-proven coronary artery disease. Eur J Clin Investig. 2013;43(3):256–266. doi: 10.1111/eci.12039. [DOI] [PubMed] [Google Scholar]
- 25.Thompson A, Danesh J. Associations between apolipoprotein B, apolipoprotein AI, the apolipoprotein B/AI ratio and coronary heart disease: a literature-based meta-analysis of prospective studies. J Inter Med. 2010;259(5):481–492. doi: 10.1111/j.1365-2796.2006.01644.x. [DOI] [PubMed] [Google Scholar]
- 26.Sarmah D, Sharma B. A correlative study of uric acid with lipid profile. Asian J Med Sci. 2014;4(2):8–14. doi: 10.3126/ajms.v4i2.7893. [DOI] [Google Scholar]
- 27.Carreón-Torres E, et al. Pioglitazone increases the fractional catabolic and production rates of high-density lipoproteins apo AI in the New Zealand White Rabbit. Atherosclerosis. 2005;181(2):233–240. doi: 10.1016/j.atherosclerosis.2004.12.047. [DOI] [PubMed] [Google Scholar]
- 28.Martínez-Ramírez M, et al. Hyperuricemia is associated with increased apo AI fractional catabolic rates and dysfunctional HDL in New Zealand rabbits. Lipids. 2017;52:999–1006. doi: 10.1007/s11745-017-4301-y. [DOI] [PubMed] [Google Scholar]
- 29.Vekic J, et al. High serum uric acid and low-grade inflammation are associated with smaller LDL and HDL particles. Atherosclerosis. 2009;203(1):236–242. doi: 10.1016/j.atherosclerosis.2008.05.047. [DOI] [PubMed] [Google Scholar]
- 30.Kengo MJH. Evaluation, and Promotion, HDL cholesterol subclasses are associated with serum uric acid in Japanese men. Health Eval Promot. 2018;45(4):563–568. doi: 10.7143/jhep.45.563. [DOI] [Google Scholar]
- 31.Kengo M, et al. Relationships of high-density lipoprotein 2 and 3 cholesterols with lifestyle habit factors in Japanese adults. Ningen Dock Int. 2014;1:54–62. [Google Scholar]
- 32.Vuorinen-Markkola H, Yki-Järvinen H. Hyperuricemia and insulin resistance. J Clin Endocrinol Metabol. 1994;1:25–29. doi: 10.1210/jcem.78.1.8288709. [DOI] [PubMed] [Google Scholar]
- 33.Yoo TW, et al. Relationship between serum uric acid concentration and insulin resistance and metabolic syndrome. Circul J. 2005;69(8):928. doi: 10.1253/circj.69.928. [DOI] [PubMed] [Google Scholar]
- 34.Abreu E, Fonseca MJ, Santos AC. Association between hyperuricemia and insulin resistance. Acta Méd Port. 2011;24(Suppl 2):565–574. [PubMed] [Google Scholar]
- 35.Krishnan E, Pandya BJ, Chung L, Hariri A. Epidemiology, Hyperuricemia in young adults and risk of insulin resistance, prediabetes, and diabetes: a 15-year follow-up study. Am J Epidemiol. 2012;176(2):108. doi: 10.1093/aje/kws002. [DOI] [PubMed] [Google Scholar]
- 36.Han T, et al. Temporal relationship between hyperuricemia and insulin resistance and its impact on future risk of hypertension. Hypertension. 2017;70:703. doi: 10.1161/HYPERTENSIONAHA.117.09508. [DOI] [PubMed] [Google Scholar]
- 37.Lanaspa MA, et al. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress: potential role in fructose-dependent and -independent fatty liver. J Biol Chem. 2012;287(48):40732. doi: 10.1074/jbc.M112.399899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sánchez-Lozada L, et al. Uric acid-induced endothelial dysfunction is associated with mitochondrial alterations and decreased intracellular ATP concentrations. Nephron Exp Nephrol. 2012;121(3–4):e71. doi: 10.1159/000345509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Takir M, et al. Lowering uric acid with allopurinol improves insulin resistance and systemic inflammation in asymptomatic hyperuricemia. J Investig Med. 2015;63(8):924–929. doi: 10.1097/JIM.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 40.Elza M, et al. Effect of insulin on renal sodium and uric acid handling in essential hypertension. Am J Hypertens. 1996;9(8):746–752. doi: 10.1016/0895-7061(96)00098-2. [DOI] [PubMed] [Google Scholar]
- 41.Won KB, et al. Atherogenic index of plasma and the risk of rapid progression of coronary atherosclerosis beyond traditional risk factors. Atherosclerosis. 2021;324(2):46–51. doi: 10.1016/j.atherosclerosis.2021.03.009. [DOI] [PubMed] [Google Scholar]
- 42.Chang Y, et al. Atherogenic index of plasma predicts hyperuricemia in rural population: a cross-sectional study from Northeast China. Int J Environ Res Public Health. 2016;13(9):879. doi: 10.3390/ijerph13090879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baliarsingh S, et al. Serum uric acid: marker for atherosclerosis as it is positively associated with "atherogenic index of plasma". Arch Physiol Biochem. 2013;119(1):27. doi: 10.3109/13813455.2012.732580. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.