TABLE 3.
Organizational Readiness for Change Trajectories, by Clinic
| Trajectories | PHC Staff Experiences | Illustrative Quotes | |
| Clinic A |
 Intercept: 4.43* Time: 0.04 Time2: −0.01 |
Early engagement from the clinical champion set the stage for organization buy-in at the start and throughout the PHC implementation process. Continual communication between PHC staff and clinic staff enabled the organization to smoothly implement PHC. |
“Over the past several months our clinic staff meeting, which is not a research meeting but just a meeting of all the clinic providers and staff, I've been getting people excited and enthusiastic and trying to head off any concerns we may have as we roll into this.” (T1, Clinical Champion) “I think I speak for the entire project staff that we feel very supported by our leadership, by our clinic team […] and the clinic staff is as supportive as they can be without causing too much additional work for them because they're overworked and understaffed. […] But they're incredibly supportive.” (T5, Outreach Coordinator) |
| Clinic B |
 Intercept: 4.57* Time: −0.04 Time2: 0.00 |
“Road bumps” were noted at T2 because PHC research staff were grouped within the IT department, whose workflow is not integrated into that of the clinic or research department. At T7, staff noted a lack of confidence navigating some PHC implementation challenges, specifically those related to co-enrolment in other studies in the clinic, and therefore contacted the clinical champion for help. |
“I think for the position we're in, it's being implemented really smoothly, but I think a lot of the road bumps, or the bumps along the way, there's questions we've had to ask that would have been easier answered if we were in a different department.” (T2, Project/Outreach Coordinator) “We've been withdrawing some folks because they were getting to co-enrolled in another research program and we definitely had to go to (…) our PI, and some leadership and ask them to kind of step in and take over on that front because we didn't think we could do it.” (T7, Study Coordinator) |
| Clinic C |
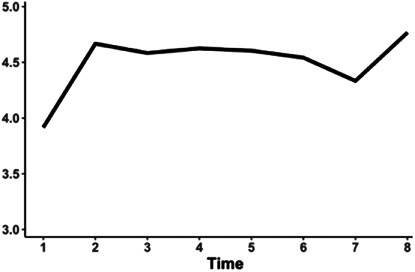 Intercept: 4.40* Time: 0.23 Time2: −0.03 |
Organizational readiness was high except at T1 and T7. This may have been because of frustrations around communication. At T1, PHC staff noted that physicians had not yet been fully introduced to PHC, which might have been a barrier to their fully supporting the intervention. At T7, PHC staff noted that the chain of communication for PHC staff is not direct. However, meetings helped clarify roles and expectations within the organization. |
“I think we've mentioned it at clinic meetings, and it'll be on our agenda for our next physician meeting, […] We'll be able to introduce it in a little bit more detail to the physicians, to let them know the study is going to be opening and that the types of patients that are going to be eligible for it.” (T7, Clinical Champion) “We'll set time at the end of the week to huddle, particularly when all the other changes, all of our staffing changes were happening. We were meeting a bit more frequently to go over what the expectations are, to understand what people's roles were, and to make sure everything was really clear.” (T7, Research Supervisor) |
| Clinic D |
 Intercept: 4.48* Time: 0.13 Time2: −0.02 |
Overall, staff felt that leadership displayed open communication and problem-solving abilities. At T7, staff felt less confident in their ability to successfully execute PHC because of organizational challenges, such as high clinical staff turnover. |
“PHC is definitely one of the main topics [discussed during the monthly clinic meeting] most of the time because it's the one study that requires the most coordination between providers and research. I think it's always being discussed, better ways of maintaining the study.” (T2, Study Coordinator) “You know, we end up doing a lot of heavy lifting by the PHC staff rather than involve the clinic staff, because we have a lot of staff turnover and is so true. So, (Data Manager) eg, and (Out reach Coordinator) now has been more involved to get the patient to come back for follow up.” (T6, Outreach Coordinator) |
Time refers to measurement time point, T1 to T8. The Time variable indicates how fast the outcome is increasing over time. The Time2 variable indicates how fast the outcome starts moving back to values from earlier in the study. The combination of these 2 effects describes the upside-down “u” shape of the trajectory over time.
P < 0.05 indicates a significant change over time.
