Abstract
Fracture-dislocations of the midfoot are relatively rare injuries. We present a case of a 20-year-old man presenting with navicular-cuneiform and calcaneal-cuboid fracture-dislocation of his right foot due to a crush injury during work. The patient's injury was treated by open reduction internal fixation.
Keywords: Case report, Midfoot injury, Chopart, ORIF
Introduction
Foot traumatic injuries are serious injuries that may disrupt the structural integrity of the midfoot. The resulting ligamentous, articular, and osseous damage commonly create diverse injury patterns sometimes involving both columns of the foot [1]. The first to describe those injuries patterns and the pathomechanism of fractures and fracture dislocations are the French surgeons François Chopart (1732–1795) and Jacques Lisfranc (1790–1847) bearing their names to the transverse tarsal (Chopart) joint, and the tarsometatarsal joint complex (Lisfranc) [2]. Dislocations patterns that occur at the level of the naviculocuneiform and calcaneocuboid joints simultaneously represent a rare innominate pattern of dislocation which according to our knowledge only 6 cases [3], [4], [5] have been described in the literature. Here we report our case of a 20-year-old man with this pattern of fracture-dislocation that was treated by open reduction and internal fixation (ORIF).
Case report
A 20-year-old man was transferred to our emergency department 24 h after sustaining a crush traumatic injury from a Forklift machine rolled on his right foot. In the ER, clinical examination showed a swollen foot but no neurovascular deficit or skin suffering. He had plantar ecchymosis which is a pathognomonic sign of midfoot injury [2], [6] (Fig. 1). No signs of foot compartment syndrome were noted.
Fig. 1.
Plantar ecchymosis (a) and skin condition (b).
Standard foot radiographs (Fig. 2) showed complex navicular–cuneiform joint dislocation, and a calcaneo-cuboid fracture dislocation. CT-scan of his foot was necessary to analyze his injury pattern and showed an important impaction of the cuboid facet associated with avulsion fracture of the anterior calcaneal process (Fig. 3). Attempts of closed reduction maneuvers in the ER department have been failed under sedation (morphine, ketamine).
Fig. 2.
Anteroposterior (a), oblique (b) and lateral (c) radiographs of the right foot showing the navicular-cuneiform and calcaneal-cuboid fracture-dislocation.
Fig. 3.
Sagittal and axial views of CT-scan of the right foot showing the o naviculocuneiform joint dislocation (a, b) and calcaneocuboid joint fracture dislocation (c, d).
As the skin wasn't tense and was in an acceptable level of edema, surgical treatment was decided on the same day by open reduction and internal fixation through two surgical approaches. The first one is a dorsomedial approach (Fig. 4) that was carried carefully through the subcutaneous tissues preserving the dorsal neurovascular bundle of the foot and superficial peroneal nerve. The tibialis anterior and extensor hallucis longus tendons were identified and protected throughout the procedure by using blunt retractors. Dissection was continued onto the dorsal aspects of the dislocated joint between the navicular and the cuneiforms [9]. After reducing these joints, we fixed the navicular bone (nav) to the first cuneiform (c1) by an LCP plate and 2.7 mm screws. The joint between first and the second cuneiforms (C1C2) was disrupted and fixed by a 2 mm K-wire. Another 2 mm K-wire was used to fix the navicular to the C2. A doubt on an additional Lisfranc injury noticed intra-operatively, insertion of a 2 mm k-wire going from the first (M1) to the fourth (M4) metatarsal bases was performed (Fig. 5). A second lateral calcaneal approach extending from the base of the fifth metatarsal toward the calcaneal tuberosity. We carefully incised all the soft tissues directly to the bone and care was taken to protect the sural nerve, peroneal tendons, and the short extensor digitarum as well [10]. We exposed the calcaneo-cuboid joint and the cuboid facet impaction. We did a mini cortical window proximal to the calcaneal fracture to elevate the articular surface, then we reduced the cuboid bone, and we fixed the calcaneocuboid joint using two 2 mm k-wires (Fig. 5). Skin closure was possible without difficulties and the patient was discharged day 3 post operatively without skin complications.
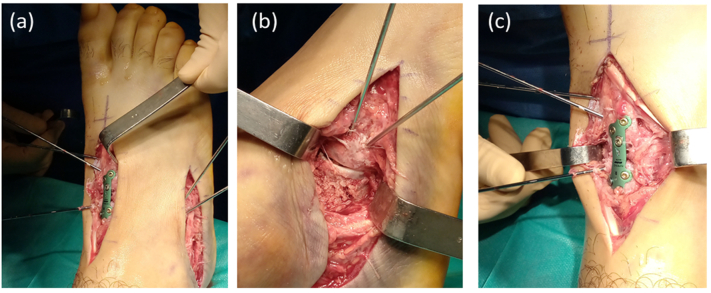
Fig. 4.
Photographs showing the two midfoot surgical approaches (a): Dorsomedial (b) and lateral calcaneal (c) approaches.
Fig. 5.
Anteroposterior and lateral radiographs post-op views of the right foot showing internal fixation with a plate and screws of N-C1 and 2 mm k wires fixing C1-C2, M1-M4 and the calcaneocuboid joints with congruous articular surfaces.
In the post-operative management, a short leg cast was applied for two months, sutures removed at 3 weeks post-operatively, wounds healed properly, with reactive skin changes to the underlying materials on the posteromedial incision but no signs of infection, k wires removed after three months without difficulty or complications. Once the cast removed at 2 months post-op, passive and active immobilization started subsequently with the aid of a physiotherapist. Weight bearing was advanced gradually as tolerated.
At one year follow-up, the patient is complaining from discomfort and intermittent pain upon walking. He also complained of stiffness and blocking sensations in the medial side of his ankle and foot. On the physical exam the skin is in a satisfying healed process and the range of motion of his ankle joint was within the normal parameters. Removal of the rest of the osteosynthesis material is previewed in the following months to relieve the patients' symptoms. Fig. 7 shows x-rays at one year follow-up.
Fig. 7.
Oblique (A), lateral(B), and Anteroposterior (C) radiographs of the right foot after one year follow-up.
Discussion
Fracture-dislocations of the midfoot are relatively rare injuries [11]. Due to its high congruence and its powerful dorsal and plantar ligamentous support, the majority of those rare injuries affect mainly the tarsometatarsal (Lisfranc) and by the midtarsal (Chopart) joints [8], [12]. We reported the case of an unusual Chopart fracture dislocation, where the calcaneocuboid joint was affected, but not the talonavicular joint. The deforming force went through the naviculocuneiform joint. We suppose that longitudinal forces were transmitted along the metatarsal rays compressing the navicular-cuneiform joint and producing dorsal dislocation of the navicular bone. This implies that rupture of the dorsal ligaments in addition to divergent disruptive forces have led to lateral cuneiform dislocation. In the lateral column, due to hyper plantar flexion and inversion forces applied to the midfoot, a calcaneocuboid joint fracture-dislocation has occurred in which the cuboid facet got impacted. An associated occult Lisfranc injury has occurred due to proximity of this joint [3], [13], [14].
Most midfoot Injuries are due to crush injuries or high-energy trauma and treated either by closed reduction with percutaneous k-wiring, open reduction internal fixation, or one-time immediate arthrodesis [15]. Nondisplaced stable injuries are treated orthopedically usually by casting [12]. In this case, we decided to perform an open reduction with internal fixation as Richter did in Chopart injuries with good functional outcomes [16]. Addressing first the medial column is essential because of its importance not only in maintaining the arch of the foot, but also because of the stronger ligaments of the navicular–cuneiform joint that restricts midfoot instability more than the calcaneal–cuboid joint which is fixed at a later step as foot surgeons recommend [7], [8].
The choice between ORIF and primary arthrodesis is controversial regarding traumatic injuries of the midfoot [17]. Limited data is available in the literature concerning outcomes after acute arthrodesis for Chopart injuries. Rammelt and Schepers described significantly worse results with primary fusion compared to ORIF while Grambart described two cases of naviculocuneiform dislocations with good outcome after primary arthrodesis [18], [19]. However, given the patient's age and the quality of articular surfaces, we decided to save the midfoot joints by choosing ORIF. Patient follow-up in the outpatient clinic at regular intervals for dressings and cast removal. A CT-scan at 2 months was done for control and showed satisfying reduction and articular congruency (Fig. 6).
Fig. 6.
Sagittal and axial views of CT of the right foot 2 month post ORIF showing the congruous articular surfaces.
Conclusion
Navicular-cuneiform and calcaneal-cuboid fracture-dislocation is uncommon injuries. We presented a rare case which was treated by ORIF with a good functional outcome at one year of follow up. There is a lack of consensus regarding the treatment choice of midfoot injuries, thus larger multi centric studies are needed to determine the best treatment option and its surgical indications.
Declarations
-
i.
No funding
-
ii.
No conflict of interest
-
iii.
Oral consent taken from the patient to publish data.
Contributor Information
Ali Fares, Email: md.alifares@gmail.com.
Benoit Orfeuvre, Email: borfeuvre@chu-grenoble.fr.
Régis Pailhe, Email: rpailhe@chu-grenoble.fr.
References
- 1.Steven M., Lawrence J. Midfoot trauma, bony and ligamentous: evaluation and treatment. Opin. Orthop. 2002;1399–106:99–100. ©2002 Lippincott Williams Wilkins, Inc. [Google Scholar]
- 2.Rammelt S., Zwipp H. Focus on midfoot injuries. Eur. J. Trauma Emerg. Surg. Jun. 2010;36:3. doi: 10.1007/s00068-010-9004-5. [DOI] [PubMed] [Google Scholar]
- 3.Cheng Y., Yang H., Sun Z., Ni L., Zhang H. A rare midfoot injury pattern: navicular—cuneiform and calcaneal—cuboid fracture—dislocation. J. Int. Med. Res. Apr. 2012;40:2. doi: 10.1177/147323001204000250. [DOI] [PubMed] [Google Scholar]
- 4.Kummer A., Crevoisier X., Eudier A., Di Cesare P.E. Calcaneocuboid and naviculocuneiform dislocation: an unusual injury of the midfoot. Case Rep. Orthop. Sep. 2020;2020 doi: 10.1155/2020/8818823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choudry Q., Akhtar S., Kumar R. Calcaneocuboid and naviculocunieform dislocation: an unusual pattern of injury. Foot Ankle Surg. Jan. 2007;13:1. doi: 10.1016/j.fas.2006.06.003. [DOI] [Google Scholar]
- 6.Ross G., Cronin R., Hauzenblas J., Juliano P. Plantar ecchymosis sign: a clinical aid to diagnosis of occult Lisfranc tarsometatarsal injuries. J. Orthop. Trauma. Feb. 1996;10:2. doi: 10.1097/00005131-199602000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Klaue K. Treatment of Chopart fracture-dislocations. Eur. J. Trauma Emerg. Surg. Jun. 2010;36:3. doi: 10.1007/s00068-010-1047-0. [DOI] [PubMed] [Google Scholar]
- 8.M. E. M. M. S. A. A. M. C. B. J. M. Stephen P.A.C.M., Benirschke K. Fractures and dislocations of the midfoot: Lisfranc and Chopart injuries. Am. Acad. Orthop. Surg. Jul. 2012;94:1326–1336. doi: 10.2106/JBJS.L00413. [DOI] [PubMed] [Google Scholar]
- 9.Schildhauer T.A., Nork S.E., Sangeorzan B.J. Temporary bridge plating of the medial column in severe midfoot injuries. J. Orthop. Trauma. Aug. 2003;17:7. doi: 10.1097/00005131-200308000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Sands A.K., Tansey J.P. Lateral column lengthening. Foot Ankle Clin. Jun. 2007;12:2. doi: 10.1016/j.fcl.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Main B.J., Jowett R.L. Injuries of the midtarsal joint. J. Bone Joint Surg. Br. Feb. 1975;57-B(1) doi: 10.1302/0301-620X.57B1.89. [DOI] [PubMed] [Google Scholar]
- 12.Ponkilainen V.T., Laine H.-J., Mäenpää H.M., Mattila V.M., Haapasalo H.H. Incidence and characteristics of midfoot injuries. Foot Ankle Int. Jan. 2019;40:1. doi: 10.1177/1071100718799741. [DOI] [PubMed] [Google Scholar]
- 13.Miersch D., Wild M., Jungbluth P., Betsch M., Windolf J., Hakimi M. A transcuneiform fracture-dislocation of the midfoot. Foot. Mar. 2011;21:1. doi: 10.1016/j.foot.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Richter M., et al. Plantar impact causing midfoot fractures result in higher forces in Chopart's joint than in the ankle joint. J. Orthop. Res. Mar. 2002;20:2. doi: 10.1016/S0736-0266(01)00096-1. [DOI] [PubMed] [Google Scholar]
- 15.Pylawka T., Andersen L.B. Midfoot trauma. Curr. Orthop. Pract. May 2008;19:3. doi: 10.1097/BCO.0b013e3282f52c0a. [DOI] [Google Scholar]
- 16.Richter M., Thermann H., Huefner T., Schmidt U., Goesling T., Krettek C. Chopart joint fracture-dislocation: initial open reduction provides better outcome than closed reduction. Foot Ankle Int. 2004;25(5):340–348. doi: 10.1177/107110070402500512. [DOI] [PubMed] [Google Scholar]
- 17.Barnds B., et al. Cost comparison and complication rate of Lisfranc injuries treated with open reduction internal fixation versus primary arthrodesis. Injury. Dec. 2018;49:12. doi: 10.1016/j.injury.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Rammelt S., Schepers T. Chopart injuries. Foot Ankle Clin. Mar. 2017;22:1. doi: 10.1016/j.fcl.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Grambart S., Patel S., Schuberth J.M. Naviculocuneiform dislocations treated with immediate arthrodesis: a report of 2 cases. J. Foot Ankle Surg. May 2005;44:3. doi: 10.1053/j.jfas.2005.05.005. [DOI] [PubMed] [Google Scholar]