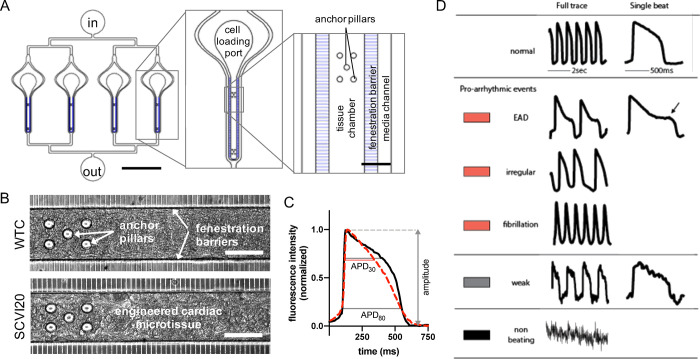
Figure 1.
Design and function of the cardiac MPS. (A) Layout of a multiplexed cardiac MPS device comprising four parallel tissue chambers with individual cell loading ports and a common media inlet (in) and outlet (out). The media channels run parallel to each tissue chamber, and the fenestration barrier provides protection from fluid shear stress while allowing for exchange of media via diffusion. Anchor pillars located at both extremities of the tissue chamber provide attachment points to keep the cardiac muscle elongated and prevent collapsing. Scale bars represent 2000 μm in the full device (left panel) and 100 μm in the close up (right panel). (B) Phase contrast images of the MPS with cardiac tissues formed using WTC (top) and SCVI20 (bottom) cells. Scale bars represent 100 μm. (C) Fluorescent voltage traces (black and dashed red curves) are analyzed for action potential duration at 80 and 30% signal amplitude (APD80 and APD30, respectively). The beat shape metric triangulation is calculated as (APD80 – APD30)/APD80. A higher triangulation value (dashed red curve) is associated with increased arrhythmia risk. Importantly, normalizing to the APD80 decouples the triangulation value from other electrophysiological changes such as beat rate or peak width. (D) Classification of beat shape quality: representative voltage fluorescence traces of a normal beat shape, three types of arrhythmia-like events (early afterdepolarization (EAD); irregular beat pattern; fast spikes without discernable baseline), a weak and noisy trace for which the beat features could not be analyzed, and a trace of a non-beating tissue. The colored rectangles represent the color code used in the bar charts throughout the article.