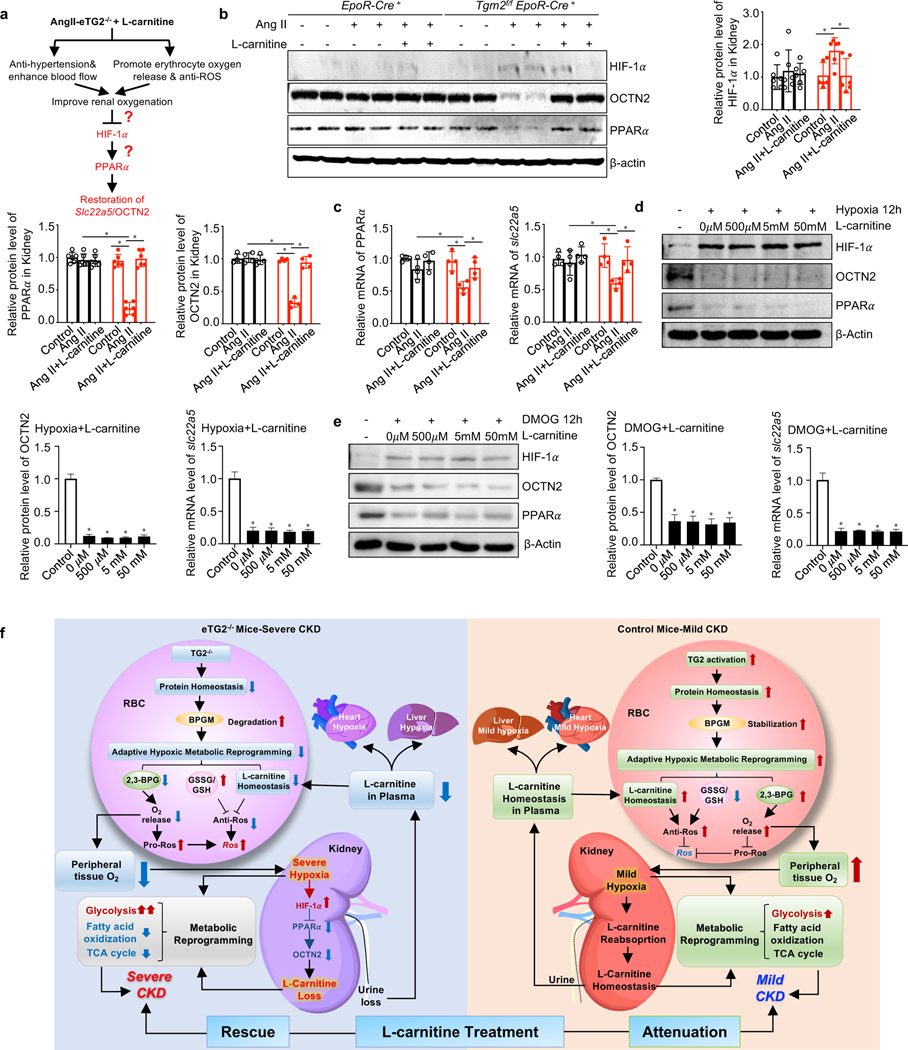
Figure 7. Restoration of renal OCTN2 underlies the improvement in CKD by carnitine supplementation in Ang II-infused eTG2−/− mice.
a. Hypothesis: L-carnitine supplementation has dual therapeutic effects to lower renal hypoxia including reducing hypertension and increasing O2 offload.
b. Protein levels of HIF-1α, OCTN2 and PPARα were detected by Western blot in kidney tissues from EpoR-Cre+ and Tgm2f/fEpoR-Cre+ mice with or without L-carnitine treatment. Protein bands were normalized to the control group. *P < 0.05, (n=4–6).
c. qRT-PCR analyses of Slc22a5 and PPARα mRNA levels from the same groups in b. *P < 0.05, n=4.
d-e. The protein levels of HIF-1α, OCTN2 and PPARα and the mRNA levels of Slc22a5 in isolated kidney organ cultures were detected after hypoxia (d) or DMOG (e) in the presence or absence of various dosages of L-carnitine. *P < 0.05, n=3.
f. Working model: eTG2 deletion impairs protein homeostasis, leading to BPGM protein degradation, in turn impairing adaptive hypoxic metabolic reprograming in erythrocytes and peripheral tissues. As for erythrocytes, decreased adaptive hypoxic metabolic reprograming is associated with reduced L-carnitine and acyl-carnitine, increased GSSG/GSH ratio and reduced 2,3-BPG production, all of which contributes to intracellular ROS increase. As for kidneys, both hypoxia and L-carnitine loss led to impaired adaptive hypoxic metabolic reprograming, increased glycolysis, reduced fatty acid oxidation and TCA activity. Hypoxia-mediated downregulation of OCTN2 via HIF-1α-PPARα axis is a key molecular link of eTG2 ablation to Ang II-induced carnitine loss, renal damage and severe CKD. As for heart and liver, insufficient L-carnitine and oxygen adaptive hypoxic metabolic reprograming leads to fibrosis. L-carnitine supplementation exhibited dual therapeutic effects including reduced hypertension and increased O2 delivery and reduced ROS in erythrocytes in eTG2−/− mice. As such, improved renal oxygenation restores renal HIF-1α-PPAR α-OCTN2 levels, maintains carnitine homeostasis and rescues severe CKD phenotype in eTG2-deficient mice. In control mice, eTG2-depedent O2 delivery is enhanced. Thus, L-carnitine attenuates mild CKD phenotype with dual therapeutic effects including reduced hypertension and lowered ROS in erythrocytes. All data are expressed as mean ± SD and were analyzed by two-way ANOVA followed with Sidak’s multiple comparisons test. See also Figure S5.