TABLE 1.
Available QSAR models for predicting various parameters in the MPML MechDermA (default methods in bold)
| Parameter | QSAR name and equation | Reference | Description | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drug partition parameters | ||||||||||||
| Stratum corneum lipid to water partition coefficient (K SClip:w) |
Equation 42 ‐ Nitsche 2006 Equation 43 ‐ Raykar 1988 Equation 44 ‐ Hansen 2013 |
108, 109, 110 | K SClip:w describes the relative affinities of water and the stratum corneum lipid phase | |||||||||
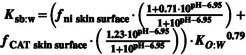
| Sebum: water partition coefficient (K sb:w) |
Equation 45 ‐ Valiveti 2008 Equation 46 ‐ Yang 2018
where: f ni – fraction of the drug which is in non‐ionized form for current pH f CAT – fraction of the drug which is cation form for the current pH |
111 | K sb:w describes the relative affinities of water and sebum | |||||||||
| Stratum corneum to viable epidermis partition coefficient (K SC:VE) |
Equation 47 ‐ Shatkin and Brown 1991 Equation 48 ‐ Modified Chen 2015 |
20, 50 |
K
SClip:VE describes the relative affinities of viable epidermis and stratum corneum
|
|||||||||
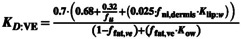
| Dermis to viable epidermis partition coefficient (K D:VE) |
Equation 49
|
20, 50 | Calculated based on estimated affinities from Chen and Shatkin and Brown methods | |||||||||
| Dermis to blood partition coefficient (K D:b ) |
Equation 50 ‐ Shatkin and Brown |
50 | ||||||||||
| Dermis to Sebum partition coefficient (K D:sb) |
Equation 51 |
|||||||||||
| Subcutis to dermis; muscle to subcutis; blood to subcutis; blood to muscle partition coefficients | User defined (No QSARs available) Default value = 1 | These subdermal tissue partition coefficients should be obtained from experimental methods or other theoretical calculations or QSARs. These tissues can be modified to mimic other deep tissues such as synovial fluid | ||||||||||
| Drug Diffusion Parameters | ||||||||||||
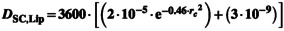
| Diffusion coefficient for SC and sebum lipid (D sc,lip/D sb) (cm2/h) |
Equation 52 ‐ Johnson Method
A = 0.000145 B = 1.32 K bolt = 1.38E‐16 J/K T [°K] = Skin[°C] + 273.15 Equation 53 ‐ Mitragotri Method
Where
Equation 54 ‐ Wang 2006 |
112 |
Johnson model is an adaptation of Stokes‐Einstein equation for diffusivity of the molecule where the parameters A, B, and gammas were estimated using the dermal diffusion data through lipid bilayer systems. The MPML MechDermA model allows modification of viscosity of SC over depth as well as that of sebum Mitragotri derived a relationship with molecular weight based on first principles and parameterization from experimental data Wang equation is similar to Mitragotri where the coefficients were estimated with a different set of experimental data |
|||||||||
| Diffusion Coefficient in VE and Dermis (D D or D VE) (cm2/h) |
Equation 55 ‐ Modified Chen 2015 Where: fu–unbound fraction of the drug; f ni,D–fraction of the drug which is in non‐ionized form for current pH; D D,free–free (unbound) drug diffusion in the dermis |
20, 68 | This is an adaptation of original Kretsos 2008 model by Chen et al. 2015 by using lipid fraction of 2.5% and using K sc,lip:w rather than LogP | |||||||||
| Diffusion coefficients in muscle and subcutis compartments | User defined (No QSARs available) Default = 1 · 10−5 | ‐ | These subdermal tissue partition coefficients should be obtained from experimental methods or other theoretical calculations or QSARs | |||||||||
| Binding in various tissues and Corneocyte permeability | ||||||||||||
| Cornecoyte permeability (P cell) (cm/h) | User defined (No QSARs available). Default = 1 · 10−5 | ‐ | The default value of this parameter is 10−5. However, this likely varies by compound. Currently no methods are available to predict this parameter | |||||||||
| Steady state binding in SC (f u,sc) |
Equation 56 ‐ Polak et al. 2018 (requires HBA, and LogP) f u,sc = 1 – (EXP(logK Nernst )/(1 + EXP(logK Nernst )) where: logK Nernst = (ln[HBA + 4.824]) (ln(abs[LogP])) Equation 57 ‐ Nitsche 2006 f u,sc = 1 / (1 + PCpro) where PCpro = 5.4·(K o:w 0.27) PCpro is the SC protein to water partition coefficient |
108, 113 | This model assumes the keratin binding is non‐saturable and equilibrium is established instantaneously. Binding is reversible | |||||||||
| Dynamic Binding in SC (K on/K off model) |
Equation 58 ‐ Seif et al. 2012 |
114 | This model accounts for difference in “on and off” rate for drug adsorption onto skin protein accounting for time‐dependent nonlinearity in binding. Binding/adsorption is reversible | |||||||||
| Binding in muscle (f u,muscle) |
Equation 59 Minimum predicted value truncated to 0.001 |
In‐house empirical model | ||||||||||
| Binding in dermis and VE |
Equation 60 where: f u –unbound fraction of the drug; f ni,t –fraction of the drug which is in non‐ionized form for current pH; Cut is the unbound concentration in tissue (dermis or VE) |
20, 68 | ||||||||||
Abbreviations: MPML MechDermA, multiphase, multilayer mechanistic dermal absorption; QSAR, quantitative structure activity relationship; SC, stratum corneum; VE, viable epidermis.