Abstract
Background
The characteristics and outcome of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-positive patients with ST-Elevation Myocardial Infarction (STEMI) undergoing primary percutaneous coronary intervention (PPCI) are still poorly known.
Methods
The PANDEMIC study was an investigator-initiated, collaborative, individual patient data (IPD) meta-analysis of registry-based studies. MEDLINE, ScienceDirect, Web of Sciences, and SCOPUS were searched to identify all registry-based studies describing the characteristics and outcome of SARS-CoV-2-positive STEMI patients undergoing PPCI. The control group consisted of SARS-CoV-2-negative STEMI patients undergoing PPCI in the same time period from the ISACS-STEMI COVID 19 registry. The primary outcome was in-hospital mortality; the secondary outcome was postprocedural reperfusion assessed by TIMI flow.
Results
Of 8 registry-based studies identified, IPD were obtained from 6 studies including 941 SARS-CoV-2-positive patients; the control group included 2005 SARS-CoV-2-negative patients. SARS-CoV-2-positive patients showed a significantly higher in-hospital mortality (p < 0.001) and worse postprocedural TIMI flow (<3, p < 0.001) compared with SARS-CoV-2-negative subjects. The increased risk for SARS-CoV-2-positive patients was significantly higher in males compared to females for both the primary (pinteraction = 0.001) and secondary outcome (pinteraction = 0.023). In SARS-CoV-2-positive patients, age ≥ 75 years (OR = 5.72; 95%CI: 1.77–18.5), impaired postprocedural TIMI flow (OR = 11.72; 95%CI: 2.64–52.10), and cardiogenic shock at presentation (OR = 11.02; 95%CI: 2.84–42.80) were independent predictors of mortality.
Conclusions
In STEMI patients undergoing PPCI, SARS-CoV-2 positivity is independently associated with impaired reperfusion and with a higher risk of in-hospital mortality, especially among male patients. Age ≥ 75 years, cardiogenic shock, and impaired postprocedural TIMI flow independently predict mortality in this high-risk population.
Keywords: Coronavirus disease 2019, COVID-19, Myocardial infarction, Mortality, Outcome
1. Introduction
Coronavirus disease 2019 (COVID-19) has strongly impacted on worldwide healthcare systems with significant resources diverted to deal with this unforeseeable modern pandemic. Several reports have described an increased cardiovascular mortality during the COVID-19 pandemic due to direct [1,2] and indirect effects of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [3], [4], [5], [6], [7], [8]. COVID-19 may induce oxygen supply/demand imbalance, abnormal systemic inflammatory response, atherosclerotic plaque rupture, overactivation of the coagulation system, and platelet hyperreactivity [1,2].
The indirect consequences of the COVID-19 pandemic included social distancing, the fear of the contagion and the prominent media attention on the uncontrolled spread of the disease, which refrained patients from activating the emergency system or doing so, but with considerable delay. The redistribution of healthcare resources affected the local emergency networks and contributed to treatment delays [7], [8], [9], [10].
Previous studies reported a very high mortality among SARS-CoV-2 positive patients with ST-segment Elevation Myocardial Infarction (STEMI) during hospitalization [11], [12], [13], [14], [15], [16], [17], [18]. However, this finding was limited to few reports and small studies with limited power for assessing the indirect (logistic) and direct reasons for the increased mortality in SARS-CoV-2 positive patients.
The aim of the present cooperation was, by merging worldwide data from real-world registry-based studies, to evaluate the clinical characteristics, natural history, and response to primary percutaneous coronary intervention (PPCI) in SARS-CoV-2 positive patients presenting with STEMI. This information can be of great interest for the clinical management of patients, for health system decisions and for the design of studies to test different treatment modalities.
2. Methods
The PercutANeous coronary intervention During COVID-19 pandEmic in SARS-CoV-2 positive patients with acute ST-segment elevation Myocardial InfarCtion (PANDEMIC) study was an investigator-initiated, collaborative individual patient data (IPD) meta-analysis of registry-based studies.
IPD was pooled when all the following eligibility criteria were satisfied: (i) SARS-CoV-2 positive STEMI patients undergoing PPCI; (ii) SARS-CoV-2 positivity confirmed by real-time reverse transcriptase–polymerase chain reaction (RT-PCR) from nasal/pharyngeal swab; (iii) availability of angiographic data; and (iv) availability of in-hospital mortality data.
A comprehensive MEDLINE, ScienceDirect, Web of Sciences, and SCOPUS search of the literature dealing with PPCI in SARS-CoV-2 positive STEMI patients was conducted from February 2020 until September 2021. The details of the search strategy are summarized in (Supplementary Table 1. Citations were screened on title and abstract level by two independent reviewers (A.S. and M.V.), and potentially eligible reports were retrieved and scrutinized in full text. Divergences were resolved by discussion and consultation with a third investigator (G.D.L.).
Exclusion criteria at the study level were: (i) Studies with less than 30 patients; (ii) use of fibrinolytic therapy as the only reperfusion therapy; (iii) unavailability of in-hospital mortality data; (iv) SARS-CoV-2 positivity suspected but not confirmed by RT-PCR; and (v) unwillingness to provide IPD.
After protocol drafting, the primary investigator of each eligible study was invited to contribute to the PANDEMIC study. Data extraction was coordinated by the primary investigator of each study. Variables of interest were selected at the study protocol stage according to the clinical relevance and consistency across studies by cross check on original publications. Additional unpublished information, including in-hospital mortality data, were provided when available in the original databases. All the data were independently checked before generating the electronic database of the PANDEMIC study; the final database was created and stored at the coordinating center (Eastern Piedmont University, Novara, Italy).
All included studies were conducted in accordance with the ethical principles of the Declaration of Helsinki and their protocols were approved by each center institutional review board.
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses of individual participant data (PRISMA-IPD) and to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) statements [19,20] (Supplementary Table 2). The review protocol was not registered on PROSPERO.
2.1. Data collection
Individual patient data were extracted and transferred in preformatted sheets including patient demographics, baseline clinical characteristics, coronary angiographic and PCI procedural features, and in-hospital mortality.
Our control group consisted of SARS-CoV-2 negative STEMI patients undergoing PPCI enrolled from March to June 2020 in the ISACS-STEMI COVID 19 registry [8].
2.2. Study endpoints
The primary study endpoint was in-hospital mortality. The secondary study endpoint was impaired postprocedural epicardial reperfusion expressed by TIMI (Thrombolysis In Myocardial Infarction) flow grade after PPCI.
2.3. Statistical analysis
Data were analyzed using SPSS Statistics Software 23.0 (IBM SPSS Inc., Chicago, Illinois). Distribution of continuous data was tested with the Kolmogorov–Smirnov and the Shapiro-Wilk test. Normally distributed variables were expressed as mean ± standard deviation, whereas non-normal ones as median and interquartile range (IQR). Categorical variables were reported as numbers and percentages. Continuous normally distributed variables were compared by using the Student t test. Categorical variables were compared with chi-squared test, or Fisher exact test when appropriate. Differences between non-normally distributed variables were tested with Mann-Whitney test.
Logistic regression analysis was conducted to evaluate the effects of SARS-CoV-2 positivity on the study outcomes. We used the propensity score technique to account for potential confounding between groups, as previously described [21,22]. For each patient, a propensity score indicating the likelihood of being SARS-CoV-2-positive was calculated through step forward logistic regression analysis that identified variables independently associated with SARS-CoV-2 positivity. We included baseline clinical variables associated with SARS-CoV-2 positivity at univariable analysis (inclusion in the model: p < 0.05; exclusion from the model: p < 0.1). The following variables were entered into the model: age, gender, hypertension, smoking, ischemia time >12 h, door-to-balloon time >30 min. preprocedural TIMI 0 flow and use of thrombectomy. The stepwise selection of the variable and estimation of significant probabilities were computed by means of maximal likelihood ratio test. The χ 2 value was calculated from the log of the ratio of maximal partial likelihood functions. The additional value of each category of variables added sequentially was evaluated on the basis of the increases in the overall likelihood statistic ratio. The final score was built according to the global χ 2 value of the multivariate statistical model and the χ 2 value of each variable. The discriminatory performance of the propensity score was assessed by the receiver operating characteristic curve method, which indicated a good accuracy of the propensity score model (area under the curve = 0.83) [23]. On the basis of the propensity score values, the population was divided into 4 groups (from the lowest to the highest probability to have SARS-CoV-2 positivity) by the use of quartiles values of the propensity score. The effect of SARS-CoV-2 positivity on the primary outcome was evaluated for each quartile, separately.
Missing data, if any, were handled using multiple imputations with the method of chained equations. Twenty data sets including imputed data were generated and combined using Rubin's rules [24].
The consistency of the main results for the primary outcome of the study was investigated across propensity score quartiles and in the following subgroups of clinical interest: age ≥75 or <75 years, females or males, presence or not of hypertension, smoking, or diabetes. A further sensitivity analysis was conducted according to the timing of SARS-CoV-2 positivity (before vs. during the hospitalization).
An additional multivariable analysis was restricted to SARS-CoV-2 positive patients in order to identify independent predictors of mortality in SARS-CoV-2 positive patients. A step forward model was used (inclusion in the model: p < 0.05; exclusion from the model: p < 0.1). A p < 0.05 was considered statistically significant.
3. Results
From a total of 1759 reports initially identified, we retrieved 1153 studies through merging of data from independent searches and removing duplicates. During screening and eligibility assessment, we identified 8 articles which fulfilled the criteria of this meta-analysis [[8], [11], [13], [14], [15], [16], [17], [18]]. IPD were provided for 6 out of 8 studies [[8], [11], [13], [14], [15], [16]] (Supplementary Fig. 1 and Supplementary Table 3), encompassing a total of 1711 patients. Of them, 941 SARS-CoV-2 positive patients were finally included in the quantitative synthesis of data based on the study criteria (Supplementary Fig. 2). Two studies did not provide IPD e and were excluded from this analysis [17,18]. The control group included a total of 2005 SARS-CoV2 negative STEMI patients undergoing PPCI enrolled in the ISACS-STEMI COVID-19 registry.
The baseline demographic, clinical and angiographic/procedural characteristics of the study population are summarized in Table 1 . SARS-CoV-2 positive patients were older (68 [IQR 58–74] vs. 63 [IQR 54–72] years, p = 0.002) than SARS-CoV-2 negative patients and were less frequently males (72.6% vs. 77.4%, p = 0.005) and active smokers (36.8% vs. 42.1%, p = 0.006). As expected, ischemia time (245 [IQR 138–605] vs. 210 [IQR 123–360] minutes, p < 0.001) and door-to-balloon time (85 [IQR 50–130] vs. 35 [IQR 22–60] minutes, p < 0.001) were longer in SARS-CoV-2 positive group. No difference was observed in the proportion of infarct location, cardiogenic shock or out-of-hospital cardiac arrest between groups.
Table 1.
Baseline demographic, clinical and angiographic/procedural characteristics according to SARS-CoV-2 positivity.
| SARS-CoV-2 Positive (n = 941) | SARS-CoV-2 Negative (n = 2005) | P value | |
|---|---|---|---|
| Age, median [25–75th] | 68 [58–74] | 63 [54–72] | 0.002 |
| Age > 75 year – n (%) | 222 (23.6) | 396 (19.8) | 0.017 |
| Male gender – n (%) | 683 (72.6) | 1551 (77.4) | 0.005 |
| Diabetes Mellitus- n (%) | 204 (21.7) | 458 (22.8) | 0.48 |
| Hypertension - n (%) | 817 (86.8) | 1121 (55.9) | < 0.001 |
| Smoking – n (%) | 346 (36.8) | 844 (42.1) | 0.006 |
| Ischemia time, median [25–75th] | 245 [138–605] | 210 [123–360] | < 0.001 |
| Total Ischemia time >12 h – n (%) | 202 (21.5) | 247 (12.3) | <0.001 |
| Door-to-balloon time, median [25 - 75th] | 85 [50–130] | 35 [22–60] | < 0.001 |
| Door-to-balloon time >30 min (%)– n (%) | 813 (86.4) | 1101 (54.9) | <0.001 |
| Anterior STEMI– n (%) | 476 (50.6) | 953 (47.5) | 0.120 |
| Out-of-hospital cardiac arrest – n (%) | 73 (7.8) | 174 (8.7) | 0.410 |
| Cardiogenic shock– n (%) |
77 (8.2) | 193 (9.6) | 0.210 |
| Radial Access (%) | 718 (81.7) | 1668 (83.2) | 0.320 |
| Culpirt vessel Left main – n (%) Left Anterior Descending Artery – n (%) Circumflex – n (%) Right Coronary Artery – n (%) Anterolateral Branch – n (%) |
21 (2.2) 455 (48.4) 124 (13.2) 333 (35.4) 1 (0.1) |
37 (1.8) 916 (45.7) 324 (16.2) 710 (35.4) 5 (0.2) |
0.310 |
| Multivessel disease – n (%) | 449 (47.7) | 1023 (51.0) | 0.094 |
| Preprocedural TIMI 0 flow – n (%) | 574 (61.0) | 1336 (66.7) | 0.003 |
| Thrombectomy– n (%) | 160 (17.0) | 410 (20.4) | 0.027 |
| Stenting– n (%) | 828 (88.0) | 1780 (88.8) | 0.530 |
| Postprocedural TIMI 3 Flow – n (%) | 829 (88.1) | 1847 (92.1) | < 0.001 |
IQR = interquartile range; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; STEMI = ST-segment Elevation Myocardial Infarction; TIMI = Thrombolysis in Myocardial Infarction.
There were no differences in rates of radial access or stent use between groups between groups, although SARS-CoV-2 positive patients less often received thrombectomy (17% vs. 20.4%, p = 0.027). Despite being associated less often with preprocedural TIMI 0 flow (61% vs. 66.7%, p = 0.003), SARS-CoV-2 positive patients showed a higher proportion of impaired postprocedural TIMI flow (TIMI 0-2: 11.9% vs. 7.9%, p < 0.001; Fig. 1 ).
Fig. 1.
Bar Graphs showing the association between SARS-CoV-2 positivity and impaired postprocedural TIMI flow (0-2) (Upper graph) and in-hospital mortality (Lower graph).
CI, confidence interval; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TIMI, Thrombolysis In Myocardial Infarction.
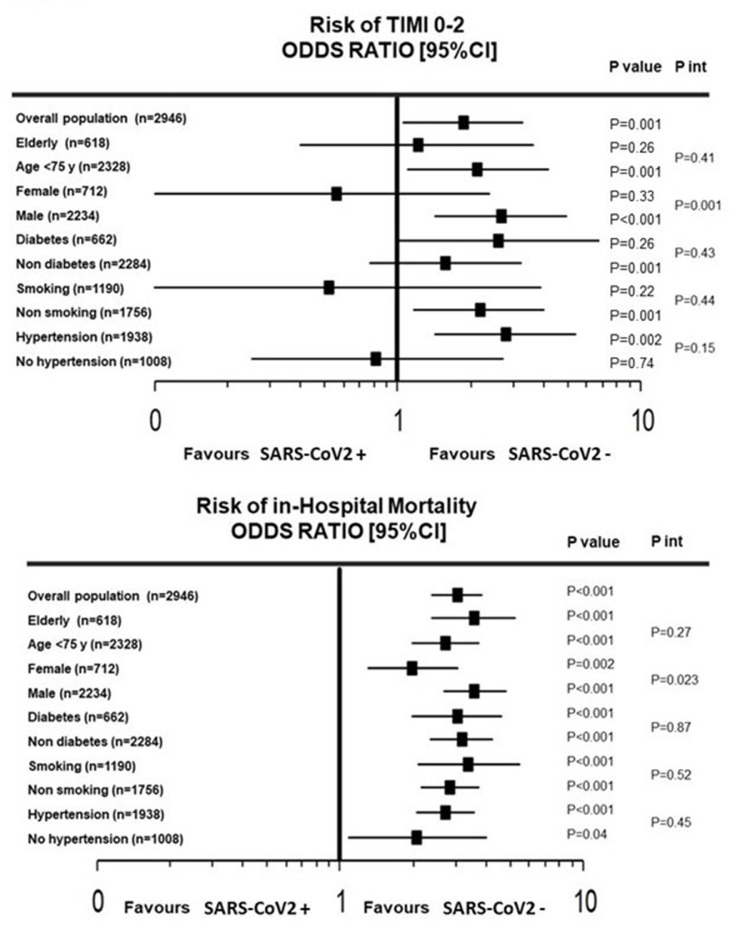
The negative impact of SARS-CoV-2 positivity on postprocedural TIMI flow was consistent across the propensity score quartile subgroups (p for interaction = 0.180; Fig. 2 ). The association of SARS-CoV-2 positivity with the probability of postprocedural TIMI 0-2 was confirmed in most of the prespecified subgroups of interest except for sex, where a significant subgroup interaction was observed (p for interaction <0.001; Fig. 3 ). In fact, male patients SARS-CoV-2 positive showed a significantly higher risk of postprocedural TIMI 0-2 than those SARS-CoV-2 negative (OR: 2.67; 95% CI: 1.43–4.99, p < 0.001); in female patients, no difference was found between groups (OR: 0.56; 95% CI: 0.13–2.42, p = 0.330). These results were confirmed after propensity score adjustment (females: adjusted OR = 0.57; 95% CI 0.31–1.03, p = 0.062; males: adjusted OR = 2.13; 95% CI 1.51–3.01, p < 0.001).
Fig. 2.
Forest plot showing the association between SARS-CoV-2 positivity and impaired postprocedural TIMI flow (0-2) (Upper graph) and in-hospital mortality (Lower graph) in each quartile of the propensity score.
CI, confidence interval; PS, propensity score; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TIMI, Thrombolysis In Myocardial Infarction.
Fig. 3.
Forest plot shows the association between SARS-CoV-2 positive and impaired postprocedural TIMI flow (0-2) (Upper graph) and in-hospital mortality (Lower graph) in major subgroups of interest.
CI, confidence interval; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TIMI, Thrombolysis In Myocardial Infarction.
SARS-CoV-2 positive patients had a significantly higher risk of in-hospital mortality (18.7% vs. 7%, OR: 3.; 95%CI: 2.40–3.85, p < 0.001; Fig. 1). Similar mortality was observed in patients with already known SARS-CoV-2 positivity before the admission (N = 738) compared with those who tested positive during the hospitalization (N = 133) (19% vs. 18%, OR: 1.06; 95% CI: 0.66–1.72, p = 0.80). These results were confirmed in all the subgroups according to the propensity score quartiles (p for interaction = 0.580) and in all the prespecified subgroups (Fig. 2 and 3). A significant heterogeneity was observed for gender, with a significantly higher impact of SARS-CoV-2 positivity on mortality in males (OR: 3.59; 95% CI: 2.70–4.79, p < 0.001) as compared to females (OR: 1.99; 95% CI: 1.3–3.04, p = 0.001; p for interaction = 0.023). The significant association between SARS-CoV-2 positivity and mortality persisted after propensity score adjustment in males (adjusted OR = 3.36; 95% CI: 2.42–4.69, p < 0.001) but not in females (adjusted OR = 1.49; 95% CI: 0.91–2.45, p = 0.110).
At multivariable logistic regression analysis, we identified age >75 years (OR = 5.72; 95% CI: 1.77–18.5, p = 0.004), postprocedural TIMI flow grade 0-2 (OR = 11.72; 95% CI: 2.64–52.10, p < 0.001), and cardiogenic shock at presentation (OR = 11.02; 95% CI: 2.84–42.80, p < 0.001) as independent predictors on in-hospital mortality among SARS-CoV-2 positive patients (Table 2 ). This result was confirmed after forcing sex into the multivariable model, which showed also an independent association of diabetes (OR = 2.19; 95% CI: 1.43–3.34, p < 0.001) and radial access (OR = 0.61; 95% CI: 0.39–0.97, p = 0.036) with in-hospital mortality (Table 2).
Table 2.
Predictors of in-hospital mortality in SARS-CoV-2 positive patients.
| Variable | Univariable analysis OR [95% CI] | P value | Multivariable analysis OR [95% CI] | P value | Sex-adjusted multivariable analysis OR [95% CI]* | P value |
|---|---|---|---|---|---|---|
| Postprocedural TIMI 0–2 | 12.5 [3.5–43.9] | <0.001 | 11.7 [2.64–52.1] | <0.001 | 10.45 [2.15–45.6] | <0.001 |
| Cardiogenic shock | 6.95 [4.27–11.3] | <0.001 | 11.0 [2.84–42.89] | <0.001 | 8.47 [2.05–20.83] | <0.001 |
| Age > 75 year | 3.89 [2.75–5.52] | <0.001 | 5.72 [1.77–52.1] | 0.002 | 4.01 [2.62–6.14] | < 0.001 |
| Out-of-hospital cardiac arrest | 2.65 [1.59–4.41] | <0.001 | – | – | ||
| Diabetes Mellitus | 2.1 [1.45–2.99] | <0.001 | – | 2.16 [1.43–3.34] | <0.001 | |
| Radial Access | 0.39 [0.26–0.57] | <0.001 | – | 0.61 [0.39–0.97] | 0.031 | |
| Smoking | 0.47 [0.33–0.69] | <0.001 | – | – | ||
| Hypertension | 2.13 [1.17–3.89] | 0.012 | – | – |
CI = confidence interval; OR = odds ratio; TIMI = Thrombolysis in Myocardial Infarction.
*multivariate analysis with sex forced into the model.
4. Discussion
This is the largest study so far conducted that describes characteristics and in-hospital outcome of SARS-CoV-2 positive STEMI patients undergoing PPCI. The main findings of this study can be summarized as follows:
(i) SARS-CoV-2 positivity is independently associated with impaired reperfusion after PPCI and a significantly higher risk of in-hospital mortality; (ii) SARS-CoV-2 positivity showed a higher prognostic impact among males, being associated with significantly higher probability of postprocedural TIMI flow 0-2 and of in-hospital mortality as compared to females; (iii) age ≥ 75 years, cardiogenic shock and impaired postprocedural TIMI flow emerged as independent predictors of mortality in this high-risk STEMI population.
Since March 2020, COVID-19 has rapidly reached pandemic proportions with more than 200 million people infected and 5 million deaths so far, and has severely stressed the healthcare systems worldwide (https://www.worldometers.info/coronavirus).
In this analysis, consistent with previous studies, we reported a significantly higher risk of in-hospital mortality among SARS-CoV-2 positive STEMI patients compared with SARS-CoV-2 negative control subjects (18.7% vs. 7.0%). This association persisted after adjustment for baseline confounders, including the propensity score, and was confirmed across the propensity score quartiles and in all the prespecified subgroups of interest.
Several indirect and direct effects have been advocated to explain the increased in-hospital mortality associated with SARS-CoV-2 positivity in patients presenting with STEMI. Among the indirect effects, the fear of contagion may have affected patients’ willingness to present to hospital, resulting in a substantial delay in cardiac catheterisation laboratory activations and consequent longer ischemia time [8,9,11,18]. In our study we confirmed the substantial longer ischemia time among SARS-CoV-2 positive patients. We also reported a longer door-to-balloon time in SARS-CoV-2 positive STEMI patients, reflecting the in-hospital delay. This has been attributed, especially during the first part of the pandemic, to the different triaging systems for STEMI patients suspected of COVID-19, to the use of COVID-19-dedicated pathways, and to the time spent for donning personal protective equipment.
Previous reports have highlighted the direct prothrombotic effects of SARS-CoV-2 infection, mainly mediated by inflammation, endothelial dysfunction, increased activation of platelets and coagulation cascade [3]. The interplay between these mechanisms increases thrombus burden and the probability of coronary distal microembolization with consequent impaired reperfusion, larger infarct size, and higher risk of mortality during the hospitalization [11]. In our study, this phenomenon was confirmed by the higher proportion of post-procedural TIMI flow <3 in SARS-CoV-2 positive patients (11.9% vs. 7.9%), which reflects the higher probability of failure in restoring normal epicardial coronary flow after PPCI in this high-risk STEMI population.
The impaired coronary reperfusion in the infarct-related artery is an established indicator of procedural success and outcome after PPCI [25,26]. In the present analysis, these parameters emerged as an independent predictor of in-hospital mortality among SARS-CoV-2 positive STEMI patients, emphasizing its value for prognostic stratification and the importance of implementing every strategy to avoid post-procedural TIMI flow <3. Previous studies reported a higher use of glycoprotein IIb-IIIa inhibitors and thrombectomy in SARS-CoV-2 positive STEMI patients compared with SARS-CoV-2 negative controls, that may certainly suggest a larger thrombus burden and potential benefits from adjunctive therapies [7,27]. In a single-center observational study including 115 consecutive STEMI patients undergoing PPCI between March 1, 2020, and May 20, 2020, SARS-CoV-2 positive patients presenting with STEMI had higher troponin levels, an impaired myocardial blush grade, and larger thrombus burden than SARS-CoV-2 negative group, resulting in a higher use of glycoprotein IIb/IIIa inhibitors and aspiration thrombectomy [11]. Furthermore, SARS-CoV-2 showed a significantly higher mortality rate and in-stent thrombosis. Similar findings have been reported in the ISACS-STEMI COVID-19 registry, which showed a higher use of glycoprotein IIb-IIIa inhibitors and thrombectomy, and a higher rate of mortality (29% vs. 5.5%) in-stent thrombosis (8.1% vs. 1.6%) and heart failure (22.6% vs. 10.6%) in SARS-CoV-2 positive STEMI patients compared with SARS-CoV-2 negative controls, that was confirmed after adjustment for confounding factors [12].
In the present study, the largest so far conducted in STEMI patients, we did not confirm the higher use of thrombectomy in SARS-CoV-2 positive patients. This result might reflect the lower rate of TIMI 0 flow at baseline in SARS-CoV-2 positive patients, but also the heterogeneity in the use of this technique between different catheterization laboratories and registries (in this meta-analysis ranged from 8.6% to 44.0%). The lower use of thrombectomy was reported in the ORPKI Polish national registry [13] and in the international COVID-ACS registry [15], where thrombectomy was less frequently used in SARS-CoV-2 positive compared with negative control subjects.
The higher mortality observed in SARS-CoV-2 positive patients may also be partially explained by the effect of COVID-19 on other organs and body systems such as the respiratory tract. Albeit this information was not available in this pooled population, previous reports have already demonstrated a higher in-hospital mortality rate, related to both cardiac and non-cardiac causes, in ACS patients with severe forms of COVID-19 [3]. In our study the mortality rate in SARS-Cov-2 positive patients remained remarkably high even after the exclusion of COVID-related deaths (13.7%).
The novelty of this meta-analysis was the significant interaction in terms of mortality between SARS-CoV-2 and gender. This result seems to reflect the significant interaction between sex and postprocedural TIMI flow, suggesting that the poorer outcome in males may be the consequence of the impaired coronary reperfusion after PPCI, more prevalent in male STEMI patients with SARS-CoV-2. In fact, postprocedural TIMI flow but not gender, in agreement with previous reports in STEMI patients [28], emerged as an independent predictor of mortality among SARS-CoV-2 positive patients. This unreported result probably reflects the larger population and the greater statistical power of this meta-analysis compared with previous studies, and suggests a gender difference in both pathophysiology and outcome for SARS-CoV-2 positive patients [29]. The interplay between sexual hormones, inflammation, and prothrombotic factors may affect the efficacy of mechanical reperfusion in males with SARS-CoV-2 infection. It has been suggested that age-related decrease's in testosterone may influence the severity of COVID-19 in males, while the presence of estrone or high gonadotropin levels may exert a protective effect in postmenopausal women [30,31]. However, further studies are needed to confirm these results, to investigate its underlying mechanisms and the benefits from adjunctive therapies in this high-risk population [2].
Previous studies have investigated the association between baseline characteristics and outcome of patients with COVID-19, and have showed that age and multiple comorbidities, including diabetes and hypertension, may precipitate clinical course during hospitalization [4]. In our study we found that among baseline risk factors, only age and cardiogenic shock at presentation independently predicted in-hospital mortality among SARS-COV-2 positive patients, The negative impact of cardiogenic shock and advanced age, is certainly in step with all previous reports in STEMI patients treated in the pre-COVID era [32,33], as much as the negative impact of postprocedural impaired epicardial reperfusion [34]. Diabetes [[35], [36]] and femoral access [37], well known predictors of worse outcome in STEMI patients, emerged as additional independent predictors of mortality when sex was forced into the model.
4.1. Study limitations
A major limitation of our study is represented by its study design, being non-randomized and retrospective. We found some differences in baseline characteristics. However, to account for potential differences between groups, in this study we employed the propensity score technique to balance for several baseline patient-related characteristics. Although we included many variables in the model, we cannot exclude a residual bias secondary to concealed confounders.
Since our population was enrolled in the initial phase of COVID-19 pandemic, the results of this study cannot be fully translated to later peaks (different viral variants, vaccines, improved pathways of care for SARS-CoV-2-positive patients, etc.). Also, potential disparities in the use of nasopharyngeal swabs in the first months of pandemic may have caused a potential selection bias.
We could not provide data on oxygen saturation and invasive mechanical ventilation use, computed tomography scan findings, and medical therapies. Also, we could not provide indexes of COVID-19 severity, the percentage of acute respiratory distress syndrome, and COVID-related deaths.
Another limitation relates to the lack of data on myocardial blush grade and thrombus grade.
A quota of the initial population was excluded because of missing information on the study outcome measures. However, the large number of events conferred a strong statistical power to our analysis.
Finally, this meta-analysis included only 6 out of 8 studies initially identified due to unavailability of IPD for two registries [17,18]. However, we suppose that their inclusion would not have substantially changed the results of this meta-analysis encompassing 941 SARS-CoV-2 positive patients from 6 multicenter international registries.
5. Conclusions
This study of STEMI patients undergoing PPCI confirmed that SARS-CoV-2 positivity is independently associated with impaired reperfusion and a significantly higher mortality during the hospitalization, especially in male patients. Age ≥ 75 years, cardiogenic shock at presentation, and postprocedural TIMI flow < 3, emerged as independent predictors of in-hospital mortality among SARS-CoV-2 positive patients.
Author contributions
G. De Luca and A. Silverio designed the study; G. De Luca, M. Verdoia and M. Nardin analyzed and interpreted the data; G. De Luca, A. Silverio and G. Galasso wrote the manuscript; all authors revised the manuscript and gave final approval.
Declaration of Competing Interest
Authors declare that they have no conflict of interest.
Acknowledgments
The study was promoted by the University of Sassari, Sassari, Italy, without any financial support.
Authors included in the manuscript met all of the following conditions: (1) substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ejim.2022.08.021.
Appendix. Supplementary materials
References
- 1.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 2.Esposito L., Cancro F.P., Silverio A., Di Maio M., Iannece P., Damato A., et al. COVID-19 and acute coronary syndromes: from pathophysiology to clinical perspectives. Oxid Med Cell Longev. 2021;2021 doi: 10.1155/2021/4936571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cenko E., Badimon L., Bugiardini R., Claeys M.J., De Luca G., de Wit C., et al. Cardiovascular disease and COVID-19: a consensus paper from the ESC working group on coronary pathophysiology & microcirculation, ESC working group on thrombosis and the association for acute cardiovascular care (ACVC), in collaboration with the European heart rhythm association (EHRA) Cardiovasc Res. 2021 doi: 10.1093/cvr/cvab298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silverio A., Di Maio M., Citro R., Esposito L., Iuliano G., Bellino M., et al. Cardiovascular risk factors and mortality in hospitalized patients with COVID-19: systematic review and meta-analysis of 45 studies and 18,300 patients. BMC Cardiovasc Disord. 2021;21:23. doi: 10.1186/s12872-020-01816-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tam C.C.F., Cheung K.S., Lam S., Wong A., Yung A., Sze M., et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on outcome of myocardial infarction in Hong Kong, China. Catheter Cardiovasc Interv. 2021;97:E194–E1E7. doi: 10.1002/ccd.28943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Luca G., Verdoia M., Cercek M., Jensen L.O., Vavlukis M., Calmac L., et al. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76:2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Luca G., Algowhary M., Uguz B., Oliveira D.C., Ganyukov V., Zimbakov Z., et al. COVID-19 pandemic, mechanical reperfusion and 30-day mortality in ST elevation myocardial infarction. Heart. 2021 doi: 10.1136/heartjnl-2021-319750. [DOI] [PubMed] [Google Scholar]
- 9.Xiang D.C., Xiang X., Zhang W., Yi S.D., Zhang J.X., Gu X.L., et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76:1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silverio A., Di Maio M., Ciccarelli M., Carrizzo A., Vecchione C., Galasso G. Timing of national lockdown and mortality in COVID-19: the Italian experience. Int J Infect Dis. 2020;100:193–195. doi: 10.1016/j.ijid.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choudry F.A., Hamshere S.M., Rathod K.S., Akhtar M.M., Archbold R.A., Guttmann O.P., et al. High thrombus burden in patients with COVID-19 presenting with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2020;76:1168–1176. doi: 10.1016/j.jacc.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Luca G., Debel N., Cercek M., Jensen L.O., Vavlukis M., Calmac L., et al. Impact of SARS-CoV-2 positivity on clinical outcome among STEMI patients undergoing mechanical reperfusion: insights from the ISACS STEMI COVID 19 registry. Atherosclerosis. 2021;332:48–54. doi: 10.1016/j.atherosclerosis.2021.06.926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tokarek T., Dziewierz A., Malinowski K.P., Rakowski T., Bartuś S., Dudek D., et al. Treatment delay and clinical outcomes in patients with ST-segment elevation myocardial infarction during the COVID-19 pandemic. J Clin Med. 2021;10 doi: 10.3390/jcm10173920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montero-Cabezas J.M., Córdoba-Soriano J.G., Díez-Delhoyo F., Abellán-Huerta J., Girgis H., Rama-Merchán J.C., et al. Angiographic and clinical profile of patients with COVID-19 referred for coronary angiography during SARS-CoV-2 outbreak: results from a collaborative, European, multicenter registry. Angiology. 2021 doi: 10.1177/00033197211028760. 33197211028760. [DOI] [PubMed] [Google Scholar]
- 15.Kite T.A., Ludman P.F., Gale C.P., Wu J., Caixeta A., Mansourati J., et al. International prospective registry of acute coronary syndromes in patients with COVID-19. J Am Coll Cardiol. 2021;77:2466–2476. doi: 10.1016/j.jacc.2021.03.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodriguez-Leor O., Cid Alvarez A.B., Pérez de Prado A., Rossello X., Ojeda S., Serrador A., et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16:1426–1433. doi: 10.4244/EIJ-D-20-00935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kiris T., Avci E., Ekin T., Akgün D.E., Tiryaki M., Yidirim A., et al. Impact of COVID-19 outbreak on patients with ST-segment elevation myocardial ınfarction (STEMI) in Turkey: results from TURSER study (TURKISH St-segment elevation myocardial ınfarction registry) J Thromb Thrombolysis. 2021:1–14. doi: 10.1007/s11239-021-02487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia S., Dehghani P., Grines C., Davidson L., Nayak K.R., Saw J., et al. Initial findings from the North American COVID-19 myocardial infarction registry. J Am Coll Cardiol. 2021;77:1994–2003. doi: 10.1016/j.jacc.2021.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart L.A., Clarke M., Rovers M., Riley R.D., Simmonds M., Stewart G., et al. Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313:1657–1665. doi: 10.1001/jama.2015.3656. [DOI] [PubMed] [Google Scholar]
- 20.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 21.De Luca G., Suryapranata H., Ottervanger J.P., van 't Hof A.W., Hoorntje J.C., Gosselink A.T., et al. Impact of statin therapy at discharge on 1-year mortality in patients with ST-segment elevation myocardial infarction treated with primary angioplasty. Atherosclerosis. 2006;189:186–192. doi: 10.1016/j.atherosclerosis.2005.11.028. [DOI] [PubMed] [Google Scholar]
- 22.Rubin D.B. Estimating causal effects from large data sets using propensity scores. Ann. Intern. Med. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 23.Hanley J.A., McNeil B.J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 24.Rubin D.B., Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10:585–598. doi: 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 25.Mehta R.H., Ou F.S., Peterson E.D., Shaw R.E., Hillegass W.B., Jr., Rumsfeld J.S., et al. Clinical significance of post-procedural TIMI flow in patients with cardiogenic shock undergoing primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2009;2:56–64. doi: 10.1016/j.jcin.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 26.Ndrepepa G., Mehilli J., Schulz S., Iijima R., Keta D., Byrne R.A., et al. Prognostic significance of epicardial blood flow before and after percutaneous coronary intervention in patients with acute coronary syndromes. J Am Coll Cardiol. 2008;52:512–517. doi: 10.1016/j.jacc.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 27.De Luca G., Navarese E., Marino P. Risk profile and benefits from Gp IIb-IIIa inhibitors among patients with ST-segment elevation myocardial infarction treated with primary angioplasty: a meta-regression analysis of randomized trials. Eur Heart J. 2009;30:2705–2713. doi: 10.1093/eurheartj/ehp118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Luca G., Gibson C.M., Gyöngyösi M., Zeymer U., Dudek D., Arntz H.R., et al. Gender-related differences in outcome after ST-segment elevation myocardial infarction treated by primary angioplasty and glycoprotein IIb-IIIa inhibitors: insights from the EGYPT cooperation. J Thromb Thrombolysis. 2010;30:342–346. doi: 10.1007/s11239-010-0451-y. [DOI] [PubMed] [Google Scholar]
- 29.Nachtigall I., Bonsignore M., Thürmann P., Hohenstein S., Jóźwiak K., Hauptmann M., et al. Sex differences in clinical course and intensive care unit admission in a national cohort of hospitalized patients with COVID-19. J Clin Med. 2021;10 doi: 10.3390/jcm10214954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brandi M.L. Are sex hormones promising candidates to explain sex disparities in the COVID-19 pandemic? Rev Endocr Metab Disord. 2021:1–13. doi: 10.1007/s11154-021-09692-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Infante M., Pieri M., Lupisella S., D'Amore L., Bernardini S., Fabbri A., et al. Low testosterone levels and high estradiol to testosterone ratio are associated with hyperinflammatory state and mortality in hospitalized men with COVID-19. Eur Rev Med Pharmacol Sci. 2021;25:5889–5903. doi: 10.26355/eurrev_202110_26865. [DOI] [PubMed] [Google Scholar]
- 32.De Luca G., van 't Hof A.W., de Boer M.J., Hoorntje J.C., Gosselink A.T., Dambrink J.H., et al. Impaired myocardial perfusion is a major explanation of the poor outcome observed in patients undergoing primary angioplasty for ST-segment-elevation myocardial infarction and signs of heart failure. Circulation. 2004;109:958–961. doi: 10.1161/01.CIR.0000120504.31457.28. [DOI] [PubMed] [Google Scholar]
- 33.De Luca G., van 't Hof A.W., Ottervanger J.P., Hoorntje J.C., Gosselink A.T., Dambrink J.H., et al. Ageing, impaired myocardial perfusion, and mortality in patients with ST-segment elevation myocardial infarction treated by primary angioplasty. Eur Heart J. 2005;26:662–666. doi: 10.1093/eurheartj/ehi110. [DOI] [PubMed] [Google Scholar]
- 34.De Luca G., Suryapranata H., van 't Hof A.W., de Boer M.J., Hoorntje J.C., Dambrink J.H., Gosselink A.T., Ottervanger J.P., Zijlstra F. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: implications for early discharge. Circulation. 2004;109(22):2737–2743. doi: 10.1161/01.CIR.0000131765.73959.87. [DOI] [PubMed] [Google Scholar]
- 35.De Luca G., Dirksen M.T., Spaulding C., Kelbæk H., Schalij M., Thuesen L., van der Hoeven B., Vink M.A., Kaiser C., Musto C., Chechi T., Spaziani G., Diaz de la Llera L.S., Pasceri V., Di Lorenzo E., Violini R., Suryapranata H., Stone G.W., DESERT cooperation Impact of diabetes on long-term outcome after primary angioplasty: insights from the DESERT cooperation. Diabetes Care. 2013;36(4):1020–1025. doi: 10.2337/dc12-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Verdoia M., Schaffer A., Barbieri L., Aimaretti G., Marino P., Sinigaglia F., Suryapranata H., De Luca G., Novara Atherosclerosis Study Group (NAS) Impact of diabetes on neutrophil-to-lymphocyte ratio and its relationship to coronary artery disease. Diabetes Metab. 2015;41(4):304–311. doi: 10.1016/j.diabet.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 37.De Luca G., Schaffer A., Wirianta J., Suryapranata H. Comprehensive meta-analysis of radial vs. femoral approach in primary angioplasty for STEMI. Int J Cardiol. 2013;168:2070–2081. doi: 10.1016/j.ijcard.2013.01.161. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.