Abstract
Background
Female sexual dysfunction is a prevalent condition affecting 12% of women, yet few academic centers in the US have female sexual medicine programs.
Aim
To characterize female sexual health programs in the United States, services offered, and training of female sexual health providers.
Methods
We performed an internet search to identify female sexual health programs and clinics in the US. From each programs’ website we abstracted the location, clinic setting (academic vs private), training of providers, and whether the clinic provided investigational services (ie, PRP injections, laser/radiofrequency therapy). We categorized clinics as specialized in sexual medicine, specialized with a focus on cancer patients, general, aesthetics-focused, general & aesthetic, or specialized & aesthetic. We used Chi-square and Fisher's exact test to evaluate association between practice setting and provision of investigational therapies with a Bonferroni-adjusted critical P-value of 0.017.
Outcomes
Our outcomes were the number of clinics in each setting, in each category, and each state, as well as the number of providers by training type.
Results
We identified 235 female sexual medicine programs in the United States. Seventeen percent were in the academic setting. Clinics in the non-academic setting were significantly (α = 0.017) more likely to offer PRP injections (0% vs 47%, P < .001), laser/radiofrequency therapy (14% vs 56%, P < .0001), and shockwave therapy (0% vs 14%, P = .011). Among all clinics, 22% provided specialized care, 2% provided care for cancer patients, 29% were more general clinics that advertised female sexual healthcare, 23% were aesthetics-focused, 22% were general practices that provided aesthetics services, and 2% were specialized clinics that offered aesthetics services. 81% of aesthetics-focused clinics advertised PRP injections. Seven states had no clinics and 26 states lacked a clinic specializing in female sexual health. The most frequent providers were OB/Gyns (40%), nurse practitioners (22%), urologists (13%), and physicians assistants (10%).
Clinical Implications
The geographic distribution of clinics and pervasiveness of clinics offering investigational services for female sexual dysfunction may be a barrier for patients seeking care.
Limitations
As a result of our internet search methodology, we likely did not capture all clinics providing female sexual health services. Further, the accuracy of our data depends on the level of detail provided on each clinics’ website.
Conclusion
Online search identified few clinics providing female sexual healthcare in academic medicine: development of such clinics could benefit patients by improving access to evidence-based care and promoting training of future providers.
Elizabeth E. Stanley and Rachel J. Pope, Characteristics of Female Sexual Health Programs and Providers in the United States. Sex Med 2022;10:100524.
Key Words: Female Sexual Health, Sexual Dysfunction, Sexual Health Providers, Hypoactive Sexual Desire Disorder, Genitourinary Syndrome of Menopause
Introduction
Female sexual dysfunction is a prevalent condition: in the United States, an estimated 44% of women experience sexual problems and 12% of women experience sexual problems associated with distress.1 Conditions causing female sexual dysfunction can impact patients’ quality of life as much as other chronic medical conditions. For example, hypoactive sexual desire disorder reduces quality of life to a similar extent as back pain and vulvovaginal atrophy reduces quality of life to a similar extent as irritable bowel syndrome.2,3 In the last decade, female sexual medicine has garnered attention as medical and surgical treatments have flourished. Research into novel treatments led to the approval of flibanserin and bremelanotide for the treatment of hyposexual desire disorder in 2015 and 2019, respectively.4,5 Other potential therapies–such as laser/radiofrequency therapy, shockwave therapy and platelet rich plasma (PRP) injections–are under investigation and are not currently recommended for treatment of female sexual dysfunction.4,6,7 Studies have also demonstrated that specialized, multidisciplinary treatment teams improve sexual function, both for cancer patient and the general population.8,9
Despite these advances in treatment for female sexual dysfunction, education about sexual health topics, including sexual dysfunction, remains limited in training programs for healthcare practitioners.10,11 Although surveys have found that patients expect healthcare providers to enquire about their sexual health,12, 13, 14 a national survey of US obstetrician/gynecologists (OB/Gyns) found that only 40% routinely ask questions to assess patients’ sexual function.15 This suggests that women experiencing sexual dysfunction may face difficulty finding a provider comfortable treating their condition. To evaluate this potential gap in care, we aim to characterize the female sexual dysfunction providers in the United States, including delineation of the clinic setting, practitioner training, and whether investigational treatments (ie, laser therapy, PRP injections) are offered. We aim to answer the questions of whether more clinics are in the nonacademic setting, and whether clinics in the nonacademic setting are more likely to offer investigational therapies.
Methods
Clinic Identification
We identified clinics using Google search between July and October 2021 and the International Society for the Study of Women's Health (ISSWSH) provider directory in February 2022. In the Google search, we used incognito mode to eliminate the effect of browser search history and search location on the results. We used the search terms “female sexual health clinic [state]” and “female sexual health doctor [state]” for each of the 50 states and Washington, DC. One researcher reviewed the first ten pages of results from each search, as well as all providers in the ISSWSH directory. We included clinics in our dataset if they met the following four criteria: (1) the clinic or practice name included “sexual medicine” or “sexual health,” or the clinic website had page(s) describing sexual health services; (2) the clinic advertised services for hypoactive sexual desire disorder, arousal disorder, or low libido; (3) the clinic webpage mentioned treating painful intercourse, or conditions that cause painful intercourse (i.e. vaginismus, vulvodynia, vaginal atrophy, etc.); (4) the clinic webpage advertised services for orgasm dysfunction. We excluded practices if the only medical staff were psychologists or physical therapists. We received a waiver from IRB approval from the University Hospitals IRB, Cleveland, OH.
To assess the robustness of our search methodology, we conducted a more comprehensive search for the state of Ohio, using the following search terms to identify additional practices: “hypoactive sexual desire disorder doctor Ohio,” “dyspareunia doctor Ohio,” “vaginismus doctor Ohio,” “orgasm disorder doctor Ohio,” “sexual arousal disorder doctor Ohio,” “sexual pain disorder doctor Ohio,” “cosmetic gynecology Ohio,” “sexual health Ohio,” and “sexual medicine Ohio.” In this search, we looked through Google results until the Google results ended, or until two consecutive pages of results did not include any medical clinics.
Data Collection
We used the website of each clinic to ascertain the state(s) in which the practice was located, number and training of medical practitioners, the clinic setting (academic vs private), and whether the clinic offered investigational therapies (laser/radiofrequency therapy, shockwave therapy, PRP injections). Providers were categorized as nurse practitioner/nurse midwife, physician assistants (PAs), physician, therapist, chiropractor, or practitioner of alternative medicine. We further categorized physicians by residency training received. Although nurse practitioners may receive training in a specialty area (i.e. nurse practitioner of women's health) we did not collect data on this training due to incomplete reporting on many clinic websites. We considered the setting to be academic if the healthcare organization was affiliated with a university or had a residency program.
We sorted clinics into one of 6 categories: specialized in sexual medicine, specialized in sexual medicine for cancer patients, general, aesthetics-focused, general & aesthetic, or specialized & aesthetic. Clinics were considered specialized in sexual medicine if they primarily provided care for female sexual dysfunction, without a specific focus on cancer patients. Clinics were considered specialized in sexual medicine for cancer patients if they advertised sexual health services for female cancer patients. Clinics were considered aesthetics-focused if they advertised themselves as a MedSpa, an antiaging/rejuvenation practice, or an aesthetics practice. Clinics were considered general if they offered female sexual health services as part of a larger family medicine, urology, or OB/Gyn practice, but did not have a specific center or program focused on female sexual health concerns. Clinics were included in the specialized & aesthetic or general & aesthetic categories if they met the definition for the specialized or general category and also offered aesthetics services (ie, facial botox injections, plastic surgery, etc).
Statistical Analysis
Statistical analyses were conducted using JMP ®16, SAS Institutes Inc., Cary, NC. We used Chi-square or Fisher's exact test to evaluate associations between clinic setting and provision of each investigational therapy. As three comparisons were made, we used a Bonferroni-corrected critical P value of 0.017 (0.05/3). Figures were generated using Microsoft Excel 365 and Microsoft Powerpoint 365, Microsoft Corporation, Redmond, WA. Maps were generated using the Microsoft Excel map generator, which uses Bing Map service. We generated descriptive statistics of clinic and provider characteristics.
Results
Clinic Characteristics
We identified 235 clinics in the United States that provided care for female sexual dysfunction. Of these, 17% (95% CI: 13.1%–22.8%) were in the academic setting. Clinics in the nonacademic setting were significantly (α = 0.017) more likely to offer PRP injections (47% vs 0%, P < .001), laser/radiofrequency therapy (56% vs 14%, P < .0001), and shockwave therapy (14% vs 0%, P = .011). Among all clinics, 52 (22%) specialized in providing care for female sexual dysfunction (without a focus on cancer); 4 (2%) provide care for cancer patients; 69 (29%) were primary care, urology, or OB/Gyn practices that advertised care for female sexual dysfunction; 54 (23%) were practices with a focus on aesthetics; 51 (22%) were general practices that provided aesthetics services; and 5 (2%) were specialized practices that also offered aesthetics services. The proportion, by clinic type, of practices in the academic setting and practices offering each investigational therapy is outlined in Table 1.
Table 1.
Clinic characteristics
| SpecializedN = 52 | CancerN = 4 | GeneralN = 69 | General & aestheticN = 51 | AestheticN = 54 | Specialized & aesthetic N = 5 | |
|---|---|---|---|---|---|---|
| Number with academic setting (% of clinic type in academic setting) |
23 (44%) | 4 (100%) | 13 (19%) | 0 (0%) | 1 (2%) | 0 (0%) |
| Number offering PRP injections (% of clinic type offering PRP injections) | 6 (12%) | 0 (0%) | 10 (14%) | 29 (57%) | 44 (81%) | 3 (60%) |
| Number offering laser therapy (% of clinic type offering laser) | 13 (25%) | 0 (0%) | 24 (35%) | 40 (78%) | 33 (61%) | 4 (80%) |
| Number offering shockwave therapy (% of clinic type shockwave) | 4 (8%) | 0 (0%) | 1 (1%) | 11 (22%) | 9 (17%) | 1 (20%) |
Practitioner Characteristics
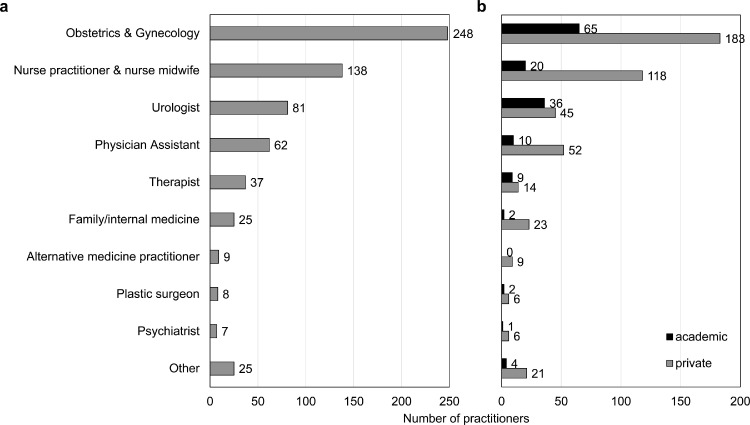
Overall, OB/Gyns comprise the majority of female sexual health practitioners (Figure 1A), with 248 identified. Next most common were nurse practitioners/nurse midwives (138), urologists (81), physician assistants (62), and family medicine/internal medicine providers (25), and therapists (23). Additional physicians identified included psychiatrists, plastic surgeons, emergency medicine doctors, endocrinologists, dermatologists, anesthesiologists, and PMR doctors. Fewer than 10 practitioners of each of these specialties were identified. There were also 3 chiropractors and 9 alternative medicine practitioners (non-accredited degrees) identified. Doctors without specialty training related to female sexual medicine (i.e. emergency medicine) more frequently practiced in the private setting and in aesthetics-focused practices (Figure 1B, Table 2).
Figure 1.
Training of Female Sexual Medicine Providers (a) Number of female sexual medicine providers by provider training. (b) Number of providers by training in academic (grey, top bar) vs. private (black, bottom bar) clinic settings. “Other” includes doctors whose training could not be ascertained, as well as emergency medicine doctors, endocrinologists, dermatologists, anesthesiologists, physical medicine and rehabilitation doctors, and chiropractors; fewer than 7 practitioners total were identified in these categories.
Table 2.
Training of female sexual medicine providers by clinic type
| Number of providers (% of providers in setting) |
||||||
|---|---|---|---|---|---|---|
| Specialized | Cancer | Aesthetic | General | General & aesthetic | Specialized & aesthetic | |
| Obstetrics & gynecology | 48 (38%) | 4 (50%) | 11 (11%) | 123 (47%) | 61 (48%) | 1 (11%) |
| Nurse practitioner & nurse midwife | 23 (18%) | 1 (13%) | 26 (26%) | >45 (17%) | 38 (30%) | 5 (56%) |
| Urologist | 23 (18%) | 1 (13%) | 1 (1%) | >46 (18%) | 7 (5%) | 3 (33%) |
| Physician Assistant | 6 (5%) | 1 (13%) | 13 (13%) | >29 (11%) | 13 (10%) | 0 (0%) |
| Therapist | 16 (13%) | 1 (13%) | 0 (0%) | >6 (2%) | 0 (0%) | 0 (0%) |
| Family/internal medicine | 3 (2%) | 0 (0%) | 12 (12%) | >5 (2%) | 5 (4%) | 0 (0%) |
| Alternative medicine practitioner | 0 (0%) | 0 (0%) | 9 (9%) | >0 (0%) | 0 (0%) | 0 (0%) |
| Plastic surgeon | 0 (0%) | 0 (0%) | 8 (8%) | >0 (0%) | 0 (0%) | 0 (0%) |
| Psychiatrist | 1 (1%) | 0 (0%) | 1 (1%) | >5 (2%) | 0 (0%) | 0 (0%) |
| Other | 5 (4%) | 0 (0%) | 20 (20%) | >1 (0%) | 4 (3%) | 0 (0%) |
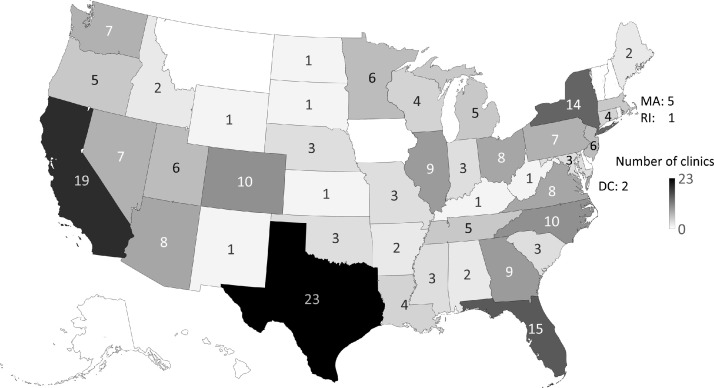
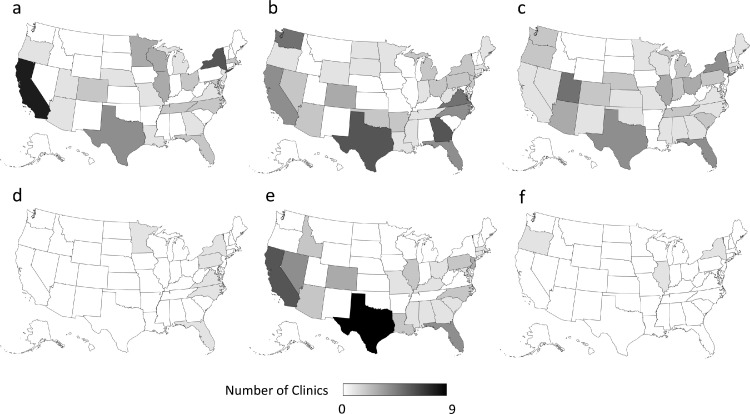
Geographical Distribution
Figure 2 depicts the geographic distribution of clinics. Texas, California, and Florida have the highest number of clinics with 23, 19, and 15, respectively. Seven states (Alaska, Hawaii, Montana, Vermont, New Hampshire, Iowa, and Delaware) all had 0 clinics; nine states only had one clinic. Twenty-six states had zero clinics specializing in treatment of female sexual dysfunction (Figure 3).
Figure 2.
Distribution of Female Sexual Health Clinics Across the United States. The number of clinics in each state is indicated on a map of the United States; darker colors represent more clinics. States in white with no data label had 0 clinics. MA: Massachusetts, RI: Rhodes Island, DC: District of Columbia.
Figure 3.
Distribution of Female Sexual Health Clinics Across the United States by Clinic Category. The number of clinics in each state is indicated on a map of the United States; darker colors represent more clinics. (a) clinics specializing in providing female sexual healthcare, (b) general clinics advertising care for female sexual health, (c) aesthetics-focused clinics, (d) specialized clinics that also offer aesthetics services, (e) general clinics that also offer aesthetics services, and (f) specialized clinics focused on cancer patients.
Evaluation of Search Methodology
In Ohio, our expanded search identified 8 clinics not identified in the initial search. Of these, 6 were aesthetics-focused clinics and 2 were general OB/Gyn practices.
Discussion
We identified 235 practices in the United States that provide care for patients experiencing female sexual dysfunction. The majority of these practices (83%) are privately-owned, and a minority (22%) focus specifically on care of patients with female sexual dysfunction. Clinics in the private setting were more likely to offer investigational therapies. Care at these clinics is mostly provided by OB/Gyns and nurse practitioners or nurse midwives. Twenty three percent of clinics providing services related to female sexual function have a focus on aesthetics and, alarmingly the majority of such clinics offer expensive, investigational services with unclear clinical efficacy in improving sexual function (81% offered PRP injections, 61% offered laser/radiofrequency treatment, and 17% offered shockwave therapy). Providers without training related to female sexual health are more likely to practice in these clinics. Further, 26 states do not have a clinic specializing in the treatment of female sexual dysfunction.
We found that only 17% of female sexual medicine clinics were in the academic setting, which suggests a lack of widespread inclusion of female sexual medicine at academic institutions. In fact, prior studies have found that sexual medicine as a whole is insufficiently covered in physician and physician assistant education.10,12,16 Further, although provision of specialized, team-based care for gynecologic cancer patients received attention in recent years,8 we found that only four comprehensive programs for cancer patients nationally. Thus, our findings further the narrative that despite increasing interest in providing quality female sexual healthcare, program development remains an important next step, especially in academics.
This study has several limitations. While our internet search methodology allowed us to identify many of the practices that patients performing an online search would identify, we likely did not capture all clinics providing care for female sexual dysfunction. In particular, our expanded search for Ohio indicates that we most undercounted aesthetics-focused clinics and general practices. For many aesthetics, general primary care, urology, and OB/Gyn practices, the amount of detail provided on the website determined whether we included the clinic in our database; thus, clinics with less-detailed websites may have been excluded despite providing care for female sexual dysfunction. Additionally, lack of information on clinic websites may have limited our ability to identify all clinics that provided investigational therapies. Additionally, in larger practices, it was not always possible to identify whether all practitioners provided care for patients with female sexual dysfunction, which may have led to an overestimate in the number of providers.
We found that general practices (120) comprised the largest number of practices offering female sexual health services, followed by aesthetics-focused practices (54). Aesthetics-focused clinics most frequently offered PRP injections. Further, 26 states lack a specialized clinic. These findings suggest that inability to identify an appropriate provider for female sexual dysfunction may pose a barrier for patients in certain geographic locations. Expansion of academic female sexual health programs could create more opportunities to educate trainees about appropriate treatment for female sexual dysfunction, enabling more providers in general practice and specialized clinics to offer evidence-based services to patients.
Statement of authorship
Conceptualization: R.J.P.; Methodology: E.E.S. and R.J.P; Formal Analysis: E.E.S.; Investigation: E.E.S.; Writing - Original Draft: E.E.S. and R.J.P.; Writing - Reviewing & Editing: E.E.S. and R.J.P.; Visualization: E.E.S.; Supervision: R.J.P.
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Shifren JL, Monz BU, Russo PA, et al. Sexual problems and distress in United States women: Prevalence and correlates. Obstet Gynecol. 2008;112:970–978. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 2.Biddle AK, West SL, D'Aloisio AA, et al. Hypoactive sexual desire disorder in postmenopausal women: Quality of life and health burden. Value Health. 2009;12:763–772. doi: 10.1111/j.1524-4733.2008.00483.x. [DOI] [PubMed] [Google Scholar]
- 3.DiBonaventura M, Luo X, Moffatt M, et al. The association between vulvovaginal atrophy symptoms and quality of life among postmenopausal women in the United States and Western Europe. J Womens Health (Larchmt) 2015;24:713–722. doi: 10.1089/jwh.2014.5177. [DOI] [PubMed] [Google Scholar]
- 4.American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology Female sexual dysfunction: ACOG practice bulletin clinical management guidelines for obstetrician-gynecologists, Number 213. Obstet Gynecol. 2019;134:e1–18. doi: 10.1097/AOG.0000000000003324. [DOI] [PubMed] [Google Scholar]
- 5.Mayer D, Lynch SE. Bremelanotide: New drug approved for treating hypoactive sexual desire disorder. Ann Pharmacother. 2020;54:684–690. doi: 10.1177/1060028019899152. [DOI] [PubMed] [Google Scholar]
- 6.Farmer M, Yoon H, Goldstein I. Future targets for female sexual dysfunction. J Sex Med. 2016;13:1147–1165. doi: 10.1016/j.jsxm.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Davis SR, Baber R, Panay N, et al. Global consensus position statement on the use of testosterone therapy for women. J Clin Endocrinol Metab. 2019;104:4660–4666. doi: 10.1210/jc.2019-01603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li JY, D'Addario J, Tymon-Rosario J, et al. Benefits of a multidisciplinary women's sexual health clinic in the management of sexual and menopausal symptoms after pelvic radiotherapy. Am J Clin Oncol. 2021;44:143–149. doi: 10.1097/COC.0000000000000800. [DOI] [PubMed] [Google Scholar]
- 9.Rullo J, Faubion SS, Hartzell R, et al. biopsychosocial management of female sexual dysfunction: A pilot study of patient perceptions from 2 multi-disciplinary clinics. Sex Med. 2018;6:217–223. doi: 10.1016/j.esxm.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eardley I, Reisman Y, Goldstein S, et al. Existing and future educational needs in graduate and postgraduate education. J Sex Med. 2017;14:475–485. doi: 10.1016/j.jsxm.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Shindel AW, Baazeem A, Eardley I, et al. Sexual health in undergraduate medical education: Existing and future needs and platforms. J Sex Med. 2016;13:1013–1026. doi: 10.1016/j.jsxm.2016.04.069. [DOI] [PubMed] [Google Scholar]
- 12.Kingsberg SA, Schaffir J, Faught BM, et al. Female sexual health: Barriers to optimal outcomes and a roadmap for improved patient-clinician communications. J Womens Health (Larchmt) 2019;28:432–443. doi: 10.1089/jwh.2018.7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fairchild PS, Haefner JK, Berger MB. Talk about sex: sexual history-taking preferences among urogynecology patients and general gynecology controls. Female Pelvic Med Reconstr Surg. 2016;22:297–302. doi: 10.1097/SPV.0000000000000291. [DOI] [PubMed] [Google Scholar]
- 14.Nappi RE, Vaginal Kokot-Kierepa M. Health: Insights, Views & Attitudes (VIVA) - Results from an international survey. Climacteric. 2012;15:36–44. doi: 10.3109/13697137.2011.647840. [DOI] [PubMed] [Google Scholar]
- 15.Sobecki JN, Curlin FA, Rasinski KA, et al. What we don't talk about when we don't talk about sex: Results of a national survey of U.S. obstetrician/gynecologists. J Sex Med. 2012;9:1285–1294. doi: 10.1111/j.1743-6109.2012.02702.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warner C, Carlson S, Crichlow R, Ross MW. Sexual health knowledge of U.S. medical students: A national survey. J Sex Med. 2018;15(8):1093–1102. doi: 10.1016/j.jsxm.2018.05.019. [DOI] [PubMed] [Google Scholar]