Abstract
Background:
Heart failure is a progressive condition characterized by frequent hospitalizations for exacerbated symptoms. Informal family caregivers may help patients improve self-care, which may in turn reduce hospitalizations. However, little is known about how mutuality, defined as the quality of the patient–caregiver relationship, and caregiver burden affect self-care.
Objective:
This study examines the associations among mutuality, patient self-care confidence (beliefs in abilities to engage in self-care behaviors) and maintenance (behaviors such as medication adherence, activity, and low salt intake), caregiver confidence in and maintenance of patient care, and caregiver perceived burden.
Methods:
This study used cross-sectional baseline data from a multi-site randomized clinical trial of a symptom and psychosocial care intervention. Patient–caregiver dyads (N=99) completed self-report surveys of mutuality and self-care confidence and maintenance, and caregivers completed a measure of caregiver burden. Path analysis, with actor (effects within a person) partner (effects across the dyad) interdependence model paths and regression models were used to examine the associations among mutuality, caregiver burden, and self-care.
Results:
The majority of patients (M age=66, 21% female) and caregivers (M age=57, 81% female) were spouses (60%). The path model demonstrated significant actor effects; patients and caregivers with better mutuality were more confident in patient self-care (p<.05). Partner effects were not significant. Regression models indicated that caregivers with greater mutuality reported less perceived burden (p<.01).
Conclusions:
Mutuality in patient–caregiver dyads is associated with patient self-care and caregiver burden and may be an important intervention target to improve self-care and reduce hospitalizations.
Keywords: Burden, confidence, maintenance, mutuality, caregiving
Improving patient self-care in heart failure represents an important opportunity to improve outcomes such as quality of life (QOL) and hospitalization.1–4 Patients with heart failure commonly rely on informal caregivers to aid with self-care.5,6 Informal caregivers, hereafter referred to as “caregivers,” are family or friends who assist patients with managing their health. Caregiver support is associated with patient adherence to self-care recommendations7 and fewer hospitalizations.8 Although caregiver involvement may be associated with improved patient outcomes, caregiving can be demanding and can lead to caregiver burden, depressive symptoms, and reduced QOL for the caregiver.9,10
Most of the literature focuses on how patient or caregiver individual factors influence patient self-care, with less attention on relationship quality within the dyad. Mutuality, the degree to which the patient–caregiver relationship is characterized by love and affection, shared pleasurable activities, shared values, and empathy, has been described as one measure of the quality of a patient–caregiver relationship.11 Evidence suggests that relationship quality, a construct closely related to mutuality, between patients with heart failure and their caregivers is related to reduced risk for patient mortality,12 improved patient health status,13 and reduced caregiver burden and depressive symptoms.14 However, among four studies that examined the associations between relationship quality and patient self-care,10,15–18 the results conflict. For example, one study15 found that both patient- and caregiver-reported empathy towards the other was associated with patient self-care confidence, whereas another16 found that only patient-reported relationship quality was related to self-care confidence. Whereas mutuality has been well-studied in patient populations other than heart failure,19 patients with heart failure and their caregivers are relatively understudied. Given the mixed findings and the limited available evidence linking patient–caregiver mutuality to patient self-care, further research needs to clarify the associations between patient–caregiver mutuality and patient self-care.
Although it is hypothesized that mutuality is beneficial for health outcomes, there is little scholarship specifying possible mechanisms specifying how mutuality may be related to better health. We draw on the Dyadic Health Behavior Change model of Trivedi et al.,10,20 suggesting that caregiver burden mediates the association between caregiver-reported mutuality and caregiver confidence in patient care. Perceived caregiver burden is the extent to which caregivers feel overwhelmed or stressed.20 Several studies show that relationship quality and mutuality are negatively associated with perceived caregiver burden.10,21–23 Caregiver burden may negatively impact caregivers’ abilities to contribute to patient self-care. Both patient and caregiver perspectives on mutuality and patient self-care are needed to fully understand the dyadic influences on patient self-care.
This study examined the relationships between patient and caregiver perceptions of mutuality and patient self-care and caregiver contributions to patient self-care. To this end, a conceptual model examining the associations between mutuality and self-care using path analysis with actor–partner interdependence model (APIM) paths24 was proposed (see Figure 1). It was hypothesized that greater mutuality would be associated with greater self-care confidence (both within a person and across the dyad). Further, consistent with self-care theory,25 it was hypothesized that greater self-care confidence would be associated with greater self-care maintenance, or ability to adhere to treatment recommendations and engage in healthy behaviors. As a secondary aim (and analysis), it was hypothesized that caregiver-reported mutuality would be related to less perceived burden, which, in turn, would be related to greater self-care confidence.
Figure 1.
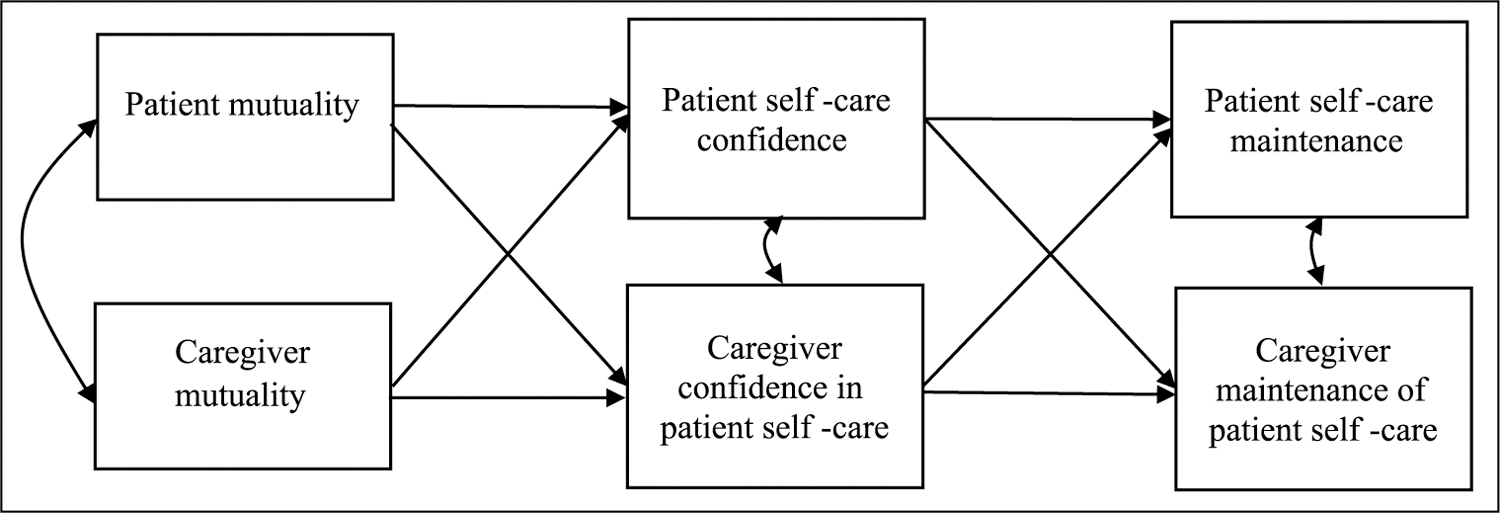
Path analysis with actor–partner interdependence paths predicting patient self-care and caregiver contributions to patient self-care.
Method
Participants
Patients with heart failure (N=314) participated in a randomized clinical trial of a symptom management and psychosocial care intervention (Collaborative Care to Alleviate Symptoms and Adjust to Illness;26 ClinicalTrials.gov Identifier: NCT01739686). The present study uses a cross-sectional study design from the baseline data of this trial, and because it focused on the patient–caregiver relationship, only patients with caregivers were included. About 66% (n = 208 of 314) of patients identified that they had an informal caregiver and were willing to have the research team contact that person for participation in the study. Only 73 of 208 (33%) caregivers were present at patient enrollment visits; thus, 147 of 208 caregivers were contacted after the enrollment visit (via mail, email, or phone) to participate. Most caregivers present agreed to participate (n = 61 of 73, 84%); however, only 38 of 147 (25%) caregivers not present for the enrollment visit participated. Thus, the final sample included 99 patient–caregiver dyads. Patients with caregivers were more likely to be married (p<.001) and to report a greater annual income (p=.04) than patients without caregivers. There were no other significant differences between patients with caregivers and patients without caregivers. This study was a planned secondary analysis of data from this trial, and caregiver measures as well as the measure of patient mutuality were added prior to the initiation of the trial for this study’s purpose.
Patients were included in the study if they (1) were ≥18 years of age; (2) able to read and understand English; (3) had consistent access to a telephone; (4) had a primary care provider willing to facilitate intervention medical recommendations; (5) had a current heart failure diagnosis with at least one of the following: (a) hospitalization primarily for heart failure, (b) prescribed ≥20 mg oral furosemide or equivalent daily, (c) brain natriuretic peptide (BNP) ≥100 or NT-proBNP ≥500, or (d) left ventricular ejection fraction ≤40%; (6) Kansas City Cardiomyopathy Questionnaire – Short Form27 score ≤70; and (7) bothered by at least one symptom (pain, depression, fatigue, or breathlessness). Patients were excluded if they had dementia, active substance abuse or dependence, schizophrenia, bipolar disorder, or comorbid metastatic cancer; lived in a nursing home; or had received a heart transplant or left ventricular assist device. Caregivers were invited to participate but it was not required for patients to participate in the clinical trial. Patients identified potential caregivers as “the one person (besides a healthcare provider) who helps you the most with your medical conditions.” Caregivers had to be ≥18 years old, able to read or understand English, and not be a paid caregiver.
Procedures
The investigation conforms to the principles outlined in the Declaration of Helsinki, and the study was approved by the Institutional Review Board. Participants were recruited between July 2012 and April 2015 from one of three area hospitals: (1) an academic-affiliated tertiary medical center; (2) a Veterans Affairs Medical Center; or (3) an integrated, urban safety net hospital. Eligible participants provided written informed consent. Informal caregivers present at the enrollment visit were also asked to participate and provided informed consent. If identified caregivers were not present, research staff asked the patient’s permission to contact the identified caregiver for participation. Patients and caregivers completed the self-report questionnaires described below. Patients completed the surveys during an in-person baseline enrollment visit using paper and pencil. Caregivers present at this visit were invited to complete the survey in person. Caregivers who were not present were either (1) mailed a paper survey with a return stamped envelope or (2) emailed a link to complete the survey in an online data management system (REDCap).28 Patients and caregivers completing surveys in the clinic were monitored by research staff, and were discouraged from consulting each other when answering questions. Because the caregivers could complete this questionnaire at their own convenience outside of the clinic, there was no way to ensure patients and caregivers did not talk when caregivers were completing their questionnaires.
Measures
Demographics and clinical characteristics.
Age, gender, race and ethnicity, education level, and clinical variables were gathered at the enrollment visit from the electronic medical record and patient self-report. Caregivers self-reported age, gender, race, ethnicity, marital status, and relationship to patient.
Mutuality.
The 15-item Mutuality Scale of the Family Caregiving Inventory11 assessed the extent to which a relationship is characterized by emotional investment and mutual support (e.g. “How much emotional support does he or she give you?”). Participants completed each item on a scale from 0 (Not at all) to 4 (A great deal). Both patients and caregivers completed this scale regarding their relationship, and higher scores indicate better mutuality. Previous evidence suggested that the Mutuality Scale demonstrates good reliability and validity in caregivers.11 Additionally, the Mutuality Scale has been used in several patient samples, including older adults,29,30 patients with Parkinson’s disease,31 and stroke survivors,32 and has demonstrated very good internal consistency (αs = .90–.95) in these samples. In this study, the internal consistency for both patients (α = .91) and caregivers (α = .94) was very high.
Self-care.
The Self-care of Heart Failure Index (SCHFI) v. 6 measured self-care behaviors recommended for patients with heart failure and included three self-care scales: maintenance, management, and confidence.33 The 10-item self-care maintenance scale assessed the extent to which patients regularly engaged in self-care behaviors (e.g. checking weight, taking medications, eating a low-salt diet) on a scale from 1 (Never or rarely) to 4 (Always or daily). Higher scores indicate greater adherence to recommended behaviors. In this sample, the internal consistency was low (α = .65), but considered acceptable for a behavioral scale. Moreover, this value was higher than what was found in the original validation study (α = .55).33 Higher scores indicated greater adherence to recommended behaviors. The six-item self-care confidence scale assessed the extent to which patients are confident that they can engage in regular self-care behaviors to keep themselves free of heart failure symptoms (e.g. “In general, how confident are you that you can keep yourself free of heart failure symptoms?”). Participants rated each item on a scale from 1 (Not confident) to 4 (Extremely confident), and higher scores indicated greater confidence in managing their health. The internal consistency of this scale was high (α = .83). Scores for both scales are converted to standardized index scores with possible scores ranging from 0 to 100. The self-care management scale was only administered if patients reported dyspnea or edema in the prior month and was not used in this study.
The Caregiver Contributions to SCHFI (CC-SCHFI) measured caregivers’ contributions to patient self-care.34 The CC-SCHFI paralleled the patient version of the SCHFI, but the maintenance scale asked how often caregivers recommended that patients do the behaviors (or how often they do the behaviors for the patient), and the confidence scale asked how confident caregivers were in helping patients manage their heart failure self-care. In the validation study, the CC-SCHFI demonstrated acceptable internal consistency and good test–retest reliability.34 Both the maintenance and confidence scales demonstrated high internal consistency (α = .89 and .86, respectively).
Perceived caregiver burden.
The 12-item Zarit Burden Inventory-Short Form (ZBI-SF)35 measured the extent to which caregivers feel overwhelmed by their caregiving responsibilities (e.g. “Do you feel stressed between caring for ______ (the name of the patient) and trying to meet other responsibilities (work/family)?”). Participants rated the extent they felt each item on a scale from 0 (Never) to 4 (Nearly always). Higher scores indicated greater perceived burden. Evidence suggested that the ZBI-SF demonstrates good reliability and validity as a measure of perceived caregiver burden,35 and the internal consistency in this sample was high (α = .89). Higher scores indicated greater perceived burden.
Data analysis
Analyses were conducted in SAS v. 9.4 and Mplus v. 7.3. Differences on demographic and clinical characteristics and study variables between patients with and without caregivers were examined using independent samples t-tests (continuous variables) and χ2 tests (categorical variables). Bivariate Pearson correlations were used to examine the associations among study variables. Differences between spousal and non-spousal caregivers on study variables were examined using independent samples t-tests, and differences in the relationships among study variables between spousal and non-spousal caregivers were examined using bivariate Pearson correlations and r to z transformations.
Using path analysis in a structural equation modeling framework, the primary analysis for this study involved APIM paths24 (see Figure 1). This method was ideal to test the proposed conceptual model because multiple relationships were estimated simultaneously, and it accounted for the nested nature of dyadic data because the dyad was the unit of analysis.24 Covariates (patient age, patient gender, caregiver age, caregiver gender, and spousal versus non-spousal caregiver) were included by adding paths from the covariates to patient and caregiver maintenance. For visual simplicity, these paths are not depicted in the figures but are included in the results table. The magnitude and significance of the path coefficients in this model were of primary interest. The actor effects were the associations within a person (e.g. patient-reported mutuality and patient-reported self-care confidence). The partner effects were the associations across members of the dyad (e.g. patient-reported mutuality and caregiver-reported confidence in patient self-care). Additionally, overall model fit was assessed using Hu and Bentler’s36 recommendations for assessing model fit, including the χ2 test of model fit (a non-significant χ2), root mean square error of approximation (RMSEA; value ≤.06), confirmatory fit index (CFI; value ≥.95), and standardized root mean-square residual (SRMR; value ≤.08).
To examine hypothesis 3, a series of regression models were used.37 First, a linear regression model with caregiver mutuality (independent variable) predicting caregiver confidence in patient self-care (dependent variable) was run. Second, the relationship between caregiver mutuality and the hypothesized mediator (caregiver perceived burden) was examined using a linear regression model. Finally, perceived burden was added to the regression model with caregiver mutuality to predict perceived caregiver burden. The indirect effects of caregiver-reported mutuality on caregiver self-care confidence through caregiver perceived burden was assessed using the product of coefficients method (quantified as the product of the relationship between the predictor and the mediator and the relationship between the mediator and the outcome38) and the Sobel standard error.39
This study was a secondary data analysis, and although there is not a consensus in the literature regarding the best approach for power analysis in path analyses, some authors suggest estimating power based on the largest multiple regression analysis in the path model.40 In our path model, the regression models predicting caregiver and patient maintenance had the largest number of predictors (eight). Using G*Power 3.1,41 we estimated our sensitivity to detect a significant effect. In our sample size of 99 dyads, and eight predictors, we have 95% power to detect a large effect (f2 = .25) and 80% power to detect a medium effect (f2 = .17). A sample size of 159 dyads would be needed to have 80% power to detect a small effect (f2 = .10).
Results
Patients were primarily male (79%) whereas caregivers were primarily female (81%) (Table 1). Caregivers were younger than patients. About 60% of caregivers were spousal caregivers, and of those patients who were married, 94% of their caregivers were spouses. Caregivers reported that the average length of their relationship with the patient was 36.8 years (SD=17 years, range = 1–70 years). Most patients and caregivers lived together (89%), for an average of 26.7 years (SD = 18.9 years, range = <1–70 years). Approximately 35% of caregivers were employed full- or part-time in addition to their caregiving responsibilities. Spousal caregivers did not report significantly better mutuality, confidence in patient self-care, maintenance of patient self-care, or more time spent caregiving than non-spousal caregivers (ps>.05). Similarly, patients with spousal caregivers did not report better mutuality, self-care confidence, or self-care maintenance than patients with non-spousal caregivers (ps>.05).
Table 1.
Demographics and clinical characteristics of patients and caregivers (N = 99 dyads).
| Characteristics | Patient | Caregiver |
|---|---|---|
| Age: mean, SD, range | 65.6, 12.4, 30–93 | 57.4, 15.8, 22–86 |
| Female: n (%) | 21 (21) | 80 (80.8) |
| Race: n (%) | N=97 | |
| White | 71 (73) | 69 (70) |
| African American | 16 (17) | 14 (14) |
| Hispanic or Latino | 7 (7) | 11 (11) |
| Other | 3 (3) | 3 (3) |
| Highest level education: n (%) | ||
| Less than high school graduate | 5 (5) | 4 (4) |
| High school graduate, or equivalent | 24 (24) | 36 (36) |
| Some college | 41 (41) | 25 (25) |
| College graduate | 16 (16) | 20 (20) |
| Any post-graduate | 13 (13) | 13 (13) |
| Current work situation: n (%) | ||
| Full time | 4 (4) | 20 (20) |
| Part time | 4 (4) | 15 (15) |
| Retired | 51 (52) | 32 (32) |
| On Disability | 29 (29) | 9 (9) |
| Homemaker | 1 (1) | 8 (8) |
| Unemployed | 6 (6) | 6 (6) |
| Other | 4 (4) | 9 (9) |
| Current relationship status: n (%) | n = 98 | |
| Married/living with a partner | 70 (71) | 81 (82) |
| Divorced or separated | 18 (18) | 5 (5) |
| Widowed | 9 (9) | 2 (2) |
| Never married | 3 (3) | 9 (9) |
| Total household income: n (%) | ||
| ≤ US$40,000 | 52 (52) | 45 (45) |
| Relationship to patient: n (%) | N/A | N = 98 |
| Spouse | 59 (60%) | |
| Partner or significant other | 10 (10%) | |
| Daughter or son | 26 (26%) | |
| Friend | 2 (2%) | |
| Other | 2 (2%) | |
| Hours per week spent caregiving: n (%) | – | N = 98 |
| <1 h | 8 (8) | |
| 1–2 h | 5 (5) | |
| 3–5 h | 1 (11) | |
| 6–8 h | 17 (17) | |
| > 8 h | 57 (58) | |
| Attend appointments with the patient? n (%) | ||
| Never | – | 4 (4) |
| Occasionally | 19 (19) | |
| Often | 16 (16) | |
| Almost all the time | 60 (61) | |
| LVEF: n (%) | N=88 | – |
| Normal: ≥ 50% | 34 (38.6) | |
| Mildly reduced: 40–49% | 18 (20.5) | |
| Moderately reduced: 30–39% | 12 (13.6) | |
| Severely reduced: <30% | 24 (27.3) | |
| NYHA class: n (%) | ||
| I: No limitation of physical activity. | 3 (3) | – |
| II: Slight limitation of physical activity. | 33 (33) | |
| III: Marked limitation of physical activity. | 49 (50) | |
| IV: Unable to carry on any physical activity without discomfort. | 14 (14) | |
| Comorbiditiesa: M, SD, range | 4.4, 1.9, 0–10 | – |
Sample sizes of each group are reported only if data were missing for that variable; for all other variables, N = 99.
Comorbidities included a count of 16 comorbidities: prior myocardial infarction, prior percutaneous coronary intervention, prior coronary artery bypass graft, diabetes, hypertension, peripheral vascular disease, cancer (non-skin), stroke or transient ischemic attack, chronic obstructive pulmonary disease, atrial fibrillation or atrial flutter, deep venous thrombosis or pulmonary embolus, sleep apnea, depression, post-traumatic stress disorder, history of alcohol abuse or history of other substance abuse.
LVEF: left ventricular ejection fraction; NYHA: New York Heart Association
Means and standard deviations of and bivariate Pearson correlations among study variables are presented in Table 2. Patient- and caregiver-reported mutuality was moderately correlated. Patient-reported mutuality was not significantly correlated with either patient self-care confidence or maintenance or caregiver confidence in or maintenance of patient care, but was negatively correlated with perceived caregiver burden. Caregiver-reported mutuality was positively correlated with caregiver confidence in patient self-care and negatively correlated with perceived caregiver burden.
Table 2.
Means and standard deviations of and Pearson correlations between survey measures.
| Measure | M (SD) | α | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|
| Patient | ||||||||
| 1. Mutuality | 3.4 (0.6) | .91 | ||||||
| 2. Self-care confidence | 63.3 (21.3) | .83 | .18 | |||||
| 3. Self-care maintenance | 66.8 (15.0) | .65 | .17 | .33* | ||||
| Caregiver | ||||||||
| 4. Mutuality | 3.3 (0.7) | .94 | .52** | .02 | .05 | |||
| 5. Confidence in patient care | 58.7 (21.6) | .86 | .12 | .12 | .16 | .27* | ||
| 6. Maintenance of patient care | 36.9 (26.4) | .89 | .10 | .05 | −.04 | −.04 | −.05 | |
| 7. Perceived burden | 13.1 (8.3) | .89 | −.28* | −.05 | −.06 | −.61** | −.29* | −.01 |
Correlations in light gray are within-patient or within-caregiver correlations; correlations in dark gray are patient–caregiver correlations.
p < .05
p < .001
N = 99 dyads
M : mean; SD: standard deviation; α: Cronbach’s alpha measure of internal consistency reliability
Mutuality, self-care confidence, and self-care maintenance among patients and caregivers
The path model fit the data well: χ2(24)=25.883, p=.36, RMSEA=.028 (90% confidence interval=.00, .08), CFI=.93, SRMR=.06. Standardized path coefficients are presented in Figure 2 and unstandardized and standardized regression coefficients are presented in Table 3.
Figure 2.
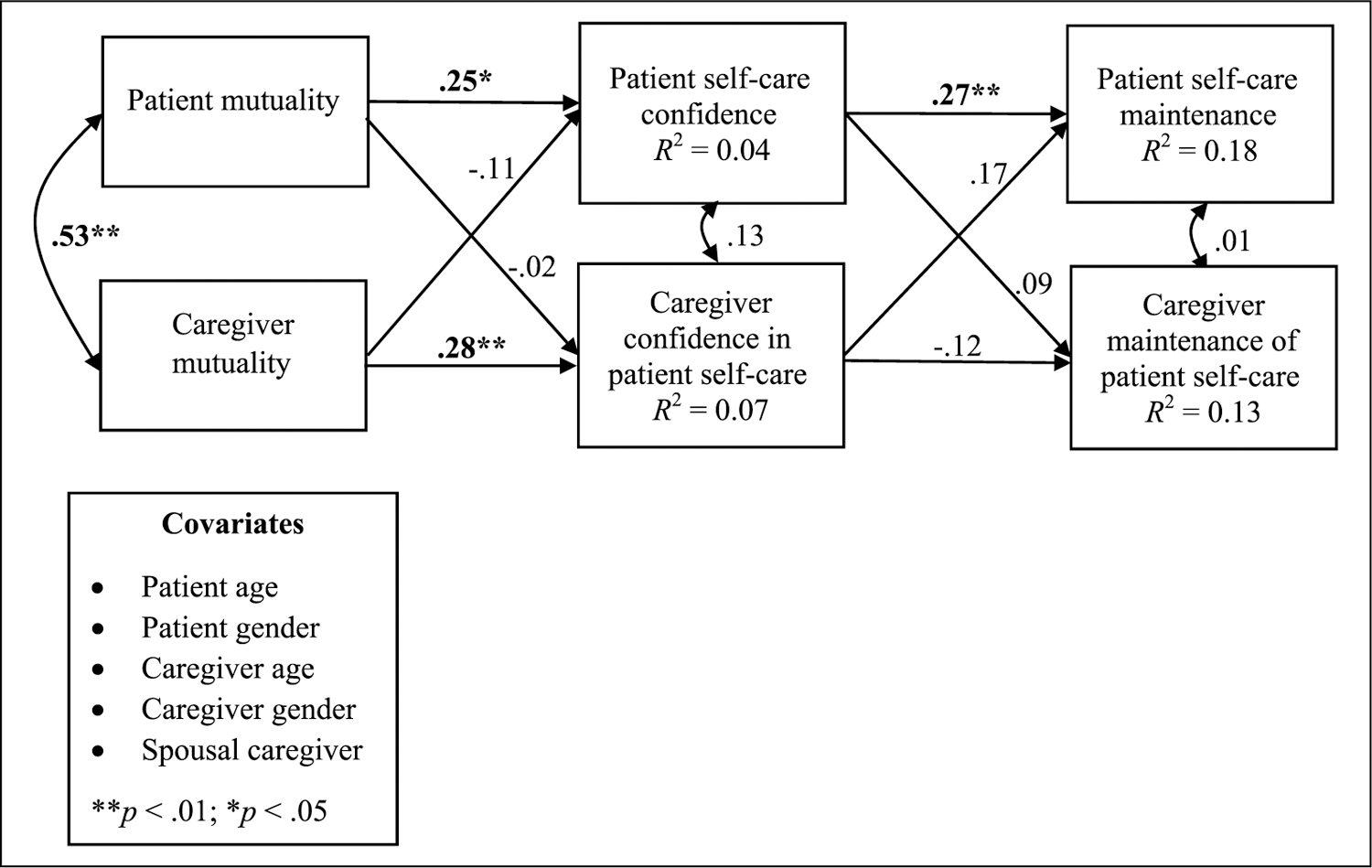
Standardized path estimates assessing hypothesized relationships. Path estimates are standardized (β) coefficients. Significant path coefficients are in bold.
Table 3.
Path model parameter estimates.
| Parameter | b | SE | p | β |
|---|---|---|---|---|
| Patient actor effects | ||||
| Patient mutuality → patient confidence | 9.35 | 4.72 | .047 | .25 |
| Patient confidence → patient maintenance | 0.19 | 0.07 | .004 | .27 |
| Caregiver actor effects | ||||
| Caregiver mutuality → caregiver confidence | 8.96 | 3.72 | .016 | .28 |
| Caregiver confidence → caregiver maintenance | −0.18 | 0.12 | .335 | −.10 |
| Patient partner effects | ||||
| Patient mutuality → caregiver confidence | −0.78 | 4.61 | .865 | −.02 |
| Patient confidence → caregiver maintenance | 0.11 | 0.12 | .356 | .09 |
| Caregiver partner effects | ||||
| Caregiver mutuality → patient confidence | −3.60 | 3.77 | .340 | −.11 |
| Caregiver confidence → patient maintenance | 0.12 | 0.07 | .071 | .17 |
| Covariances | ||||
| Patient mutuality with caregiver mutuality | 0.19 | 0.04 | .000 | .53 |
| Patient confidence with caregiver confidence | 56.36 | 43.55 | .196 | .13 |
| Patient maintenance with caregiver maintenance | 4.55 | 33.45 | .136 | .01 |
| Covariates | ||||
| Patient maintenance | ||||
| Male caregiver | 3.85 | 4.21 | .361 | .10 |
| Male patient | 4.88 | 3.58 | .172 | .16 |
| Patient age | 0.09 | 0.16 | .583 | .07 |
| Caregiver age | 0.05 | 0.13 | .715 | .05 |
| Spousal caregiver | −6.13 | 4.33 | .156 | −.17 |
| Caregiver maintenance | ||||
| Male caregiver | −17.51 | 7.73 | .023 | −.26 |
| Male patient | −11.03 | 6.56 | .093 | −.21 |
| Patient age | 0.15 | 0.29 | .604 | .07 |
| Caregiver age | −0.14 | 0.24 | .571 | −.08 |
| Spousal caregiver | −1.73 | 7.94 | .828 | −.03 |
As hypothesized, patient actor paths were all significant. Patient-reported mutuality was significantly and positively associated with patient self-care confidence. Thus, patients who reported better mutuality were more confident in their abilities to maintain self-care. Interestingly, the correlation between patient-reported mutuality and patient self-care confidence presented in Table 2 was not significant, but after controlling for covariates (patient and caregiver age and gender, spousal versus non-spousal caregiver), and caregiver mutuality in the path model, this relationship became statistically significant in the path model. Patient self-care confidence was significantly and positively associated with patient self-care maintenance. Thus, patients who were more confident in their self-care abilities also reported engaging in more self-care maintenance behaviors.
For the caregiver actor paths, caregiver-reported mutuality was also significantly and positively associated with caregiver confidence. Caregivers who reported better relationships with their patients also reported more confidence in patient self-care. However, in contrast to what was expected, the relationship between caregiver confidence in patient self-care and caregiver maintenance of patient self-care was not significant. More confident caregivers did not assist with patient self-care maintenance behaviors.
Further, none of the partner paths in the model were statistically significant. Patient-reported mutuality was not significantly related to caregiver confidence in patient self-care; similarly, caregiver mutuality was not significantly related to patient self-care confidence. Patient confidence in self-care was not related to caregiver contributions to patient self-care maintenance. Similarly, caregiver confidence in patient self-care was not related to patient self-care maintenance.
Associations among mutuality, caregiver burden, and self-care confidence in caregivers
To test hypothesis 3, a series of regression models were conducted to examine whether perceived caregiver burden was associated with caregiver mutuality and caregiver confidence in patient self-care through effects on perceived caregiver burden. In our correlation analyses, we determined that all three variables were significantly associated with one another in the expected directions (see Table 2). In the first step, caregiver-reported mutuality was significantly and positively associated with perceived caregiver confidence (see Figure 3(a)). In the second step, perceived caregiver burden was also significantly and negatively associated with caregiver confidence in patient self-care (b= −0.76, SE=0.25, β= −.29, p=.003; see Figure 3(b)). Caregivers who reported greater burden were also less confident in patients’ self-care. After adding perceived caregiver burden to the model, the negative association between perceived caregiver burden and caregiver confidence in patient self-care was no longer significant (b= −0.54, SE=0.32, β= −.21, p=.09; see Figure 3(b)). Similarly, the association between caregiver mutuality and caregiver confidence was no longer significant (b=4.58, SE=3.94, β=.14, p=.25; see Figure 3(c)). The indirect association between caregiver-reported mutuality and caregiver confidence in patient self-care through perceived caregiver burden was not significant (z=1.54, SE=2.47, p=.089, β=.12). Thus, the full mediation model was not supported. This suggests that greater caregiver mutuality is associated with less perceived caregiver burden, and both may play a role in greater caregiver confidence in patient self-care.
Figure 3.
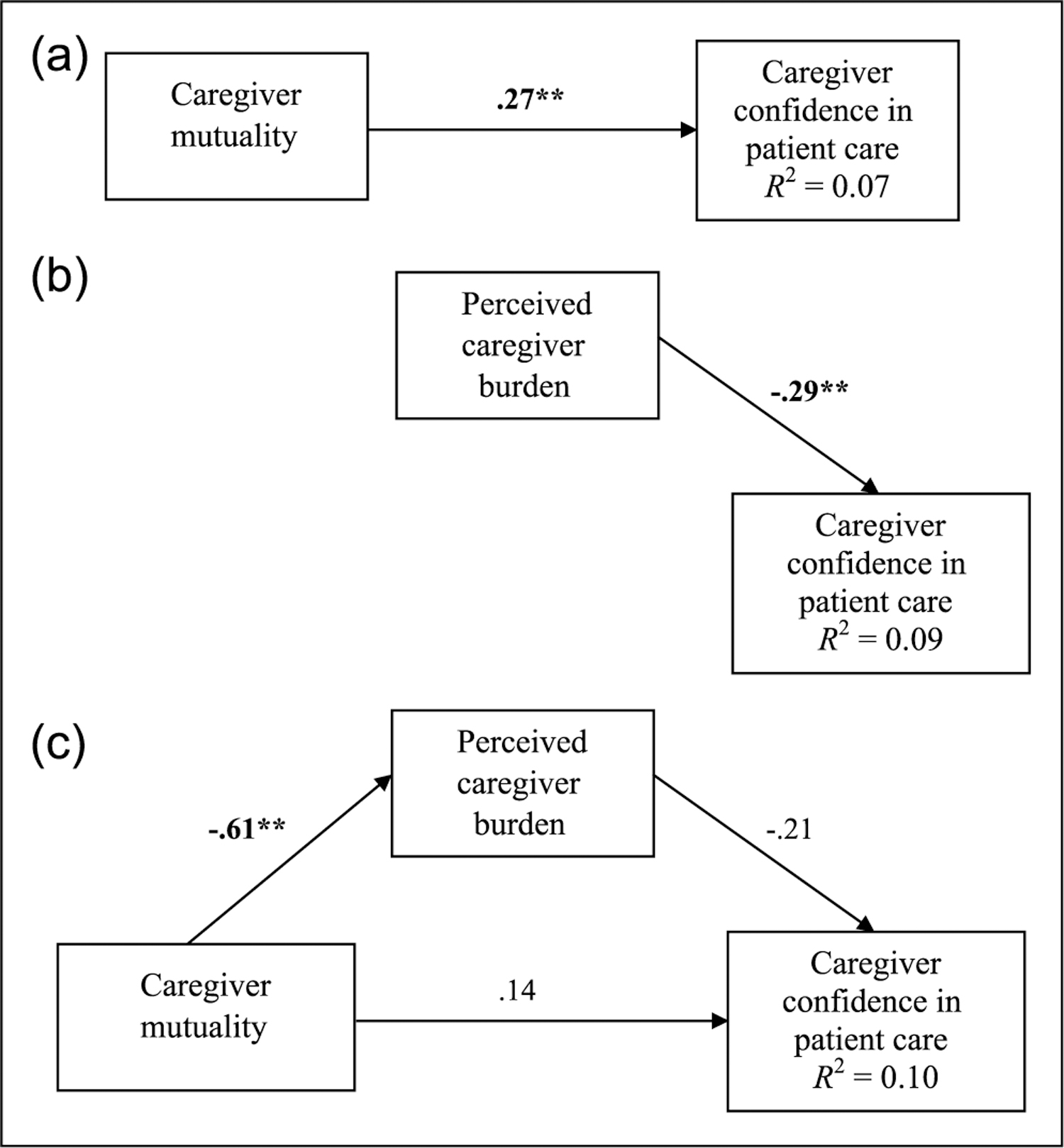
Regression models examining the relationships between caregiver mutuality, caregiver confidence in patient care, and perceived caregiver burden. (a) Regression model with caregiver mutuality predicting caregiver confidence in patient self-care. (b) Regression model with caregiver burden predicting caregiver confidence in patient self-care. (c) Regression mediation model with caregiver mutuality and perceived caregiver burden predicting caregiver confidence in patient self-care.
Regression estimates are standardized (β) coefficients. Significant regression coefficients are in bold. The relationship between caregiver mutuality and perceived caregiver burden (in (c)) is from a separate linear regression model with caregiver mutuality predicting perceived caregiver burden.
**p < .01.
Discussion
This study examined the associations among mutuality, caregiver burden, patient self-care, and caregivers’ contributions to patient self-care. Patients and caregivers who perceived better mutuality also reported more confidence in patient self-care, and for patients, those who were more confident also reported better maintenance. However, there were no significant partner effects, suggesting that patient and caregiver perceptions of mutuality did not relate to the other’s confidence, nor did confidence of one member of the dyad relate to the other’s maintenance of patient self-care. Caregivers who reported greater mutuality were less burdened, and results suggest that reduced burden and caregiver perception of mutuality play a role in caregiver confidence in patient self-care.
Patients and caregivers who perceived better mutuality were more confident in patient self-care. These results suggest that patients who feel as though they have good quality relationships with their caregivers have more confidence to engage in the required self-care behaviors, and caregivers who perceive their relationships with their patients being of good quality are more confident in the patients’ abilities to engage in self-care. Some studies suggest that this finding could be due to increased social support, which is related to both self-care confidence and maintenance in patients with heart failure.42,43 Family members may assist patients with maintaining treatment regimens43 and patients who have support from caregivers may be more confident in their self-care abilities.44 Having quality relationships with important others, such as caregivers, may give patients reasons or meaning to engage in healthy behaviors.45–48
Consistent with hypothesis 3 and Trivedi and colleagues’20 Dyadic Health Behavior Change model, the findings also imply that mutuality is associated with reduced burden, and both may play a role in caregiver confidence in patient self-care. This may be because caregivers who perceive their relationships with their patients to be mutually beneficial may not see the caregiving tasks they are performing as burdensome,21 and are therefore more confident in patients’ abilities to maintain their self-care.
Contrary to the hypotheses, there were no observed partner effects. Patient-reported mutuality was not associated with caregivers’ confidence in patient self-care, and caregiver-reported mutuality was not associated with patient-reported self-care confidence. This implies that how one perceives the quality of the relationship is more important for self-care confidence than how a partner perceives the quality of the relationship. In contrast, one study demonstrated that patients’ total perception of relationship qualities, but not caregivers’ perception of relationship, were significantly and positively related to patients’ and caregivers’ confidence in patients’ self-care.16 However, in another study, only caregiver perceptions of relationship quality were positively associated with caregiver confidence (actor effects).6
It is not clear what may account for the differences in findings, but there is likely substantial variability in patient–caregiver dyads in heart failure. Our study enrolled patients who were symptomatic and experiencing poor health status. If patients are more symptomatic, caregivers may be more burdened and relationships may be more strained. Another possibility is that mutuality and relationship quality are often measured in multiple ways, including various self-report questionnaires (e.g. marital satisfaction, marital quality, communication concerns, relationship satisfaction (Dyadic Adjustment Scale49), and relationship quality (Caregiver Esteem Subscale50)).14 The variability in measurement across studies may also contribute to the variability in findings. Our study also included non-spousal caregivers, which accounted for 40% of the sample. It is possible that this may also contribute to the lack of partner effects; however, our results indicated that spousal and non-spousal caregivers did not differ on mutuality or contributions to self-care, nor were most bivariate relationships different between dyads comprising spousal and non-spousal caregivers. Finally, it is possible that partner effects are very small, and this study was not sufficiently powered to detect partner effects.
To improve research in caregiver dyads, it may be helpful to carefully design studies to fully understand partner effects. Some constructs may not be as sensitive to partner effects (e.g. self-care) whereas others (e.g. depression) may be more sensitive to partner effects. The only way to discern these differences is to continue high-quality caregiver research. We recommend that researchers adequately power studies to detect small effects, reduce the lag time between patient and caregiver survey administration as much as possible, and ensure that both patients and caregivers agree about their roles in the relationship (both the patient and caregiver see the caregiver as such).
Consistent with heart failure self-care theory25 and previous research,51 patients with greater self-care confidence reported engaging in more self-care behaviors. Conversely, caregivers’ confidence in patient self-care may not influence the extent caregivers contribute to patient self-care. Increasing patient self-care confidence may be an important target to improve patient self-care, but targeting caregiver confidence may not improve a patient’s own self-care behaviors. The models reported herein accounted for small to medium proportions of the variance in self-care confidence and self-care maintenance, respectively, suggesting that mutuality and burden could improve both patient self-care confidence and caregivers’ confidence in patient self-care, which may in turn impact patient self-care maintenance. However, causal studies are still needed to test this hypothesis. Ultimately, improving patient self-care maintenance could improve patient QOL and reduce rehospitalizations for exacerbated symptoms.1–4
This study has several methodological strengths. First, the sample of patient–caregiver dyads was larger than in many heart failure dyad studies and was adequately powered to detect medium and large effects. To our knowledge, only one study examining mutuality and self-care has been conducted with a larger sample of dyads (N = 329 dyads)16 and most include less than 60 dyads.14 Additionally, mutuality was examined from both patient and caregiver perspectives. Many of the studies in this area have used the perspective of one member of the dyad and not a combination of the two. Finally, patient–caregiver dyads were recruited from three different health systems. The diversity in the patient population may increase the generalizability of these results to larger populations of patients with heart failure and their caregivers. Study limitations include a sample with primarily male patients and primarily female caregivers who are predominantly Caucasian, well educated, and younger than some heart failure patient samples; the cross-sectional design; self-reported self-care behavior rather than objectively measured behavior; a low survey response rate from caregivers not present at the patients’ enrollment visit; caregivers completing their surveys at home may have communicated with their patients when completing questionnaires; and insufficient power to identify small effects or examine differences among the patient–caregiver dyads by caregiver’s relationship to patient (spousal versus non-spousal).
These findings raise several important future directions. Larger, longitudinal studies of the dyadic influences on patient self-care are needed. Additionally, given the potential negative impact of caregiving on caregivers’ QOL9 and that caregivers of patients with heart failure are highly distressed,49 studies examining how mutuality influences caregivers’ own self-care behaviors are needed. Finally, designing and testing interventions to improve mutuality and patient self-care could experimentally test the study’s hypotheses. One small pilot study that addressed self-management and managing negative emotions, interpersonal relationship issues, and relationship stress in patients with heart failure and their caregivers demonstrated improvements in patients’ self-management, communication, and relationship quality and caregivers’ depressive symptoms and caregiver burden.20 In this particular intervention, patients and caregivers attended six in-person sessions, two of which focused on the dyadic relationship by using strategies to build empathy, increase constructive communication, reduce negative or counterproductive interactions, improve collaboration, and reframe heart failure as “our problem” rather than just the patient’s problem. The intervention demonstrated improvements in caregiver depression, mutuality, and burden, but was not powered to test intervention efficacy. Thus, work remains to be done to establish interventions to improve mutuality, which may influence patient self-care confidence and caregiver confidence in patient self-care.
In conclusion, mutuality in patients with heart failure and their caregivers has several important associations with self-care confidence and reduced perceptions of caregiver burden. Ultimately, addressing mutuality in patient–caregiver dyads may be an important intervention target to improve patient self-care and to potentially reduce hospitalizations, which in turn could reduce overall healthcare costs.
Implications for practice.
Caregivers who are experiencing high levels of burden could be targeted for assistance, relief, or skills training to improve confidence and reduce burden.
Screening for the quality of the patient–caregiver relationship in the clinic could be done through brief self-report questions (e.g. using the Mutuality scale) or by asking brief interview questions (e.g. “How is your relationship with [the patient or your caregiver]?” “Do you feel supported by [him or her]?”).
Practitioners may address the quality of the patient–caregiver relationship (i.e. mutuality) through screening, psychoeducation, or targeted interventions to improve patient self-care.
Although formal intervention strategies in the clinic have yet to be empirically tested, patient–caregiver dyads with identified difficulties could be encouraged to communicate about any problems. Consider a referral to a clinic social worker or chaplain. Those with more complicated relationship difficulties could be referred to mental health professionals for focused interventions to improve mutuality.
Some interventions for patients and caregivers with heart failure use strategies to build empathy, increase constructive communication, reduce negative or counterproductive interactions, improve collaboration, and reframe heart failure as “our problem” rather than just the patient’s problem to help reduce caregiver burden and improve mutuality.20
Acknowledgement
The views expressed in this paper are those of the authors and do not necessarily reflect the views of the Department of Veterans Affairs, the NIH, or the United States Government.
Funding
This work was supported by the National Institutes of Health (NIH) National Institute of Nursing Research (grant number R01NR013422 to DBB); NIH/NCATS Colorado CTSA (grant number UL1 TR001082); the American Heart Association Southwest Affiliate (grant number 14PRE18710033 to SAH); and the Department of Veterans Affairs (grant numbers HSR&D CDA 09–206 to RBT and HSR&D CDA 08–022 to DBB).
Footnotes
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
References
- 1.Riegel B, Moser DK, Anker SD, et al. State of the science: Promoting self-care in persons with heart failure: A scientific statement from the American Heart Association. Circulation 2009; 120: 1141–1163. [DOI] [PubMed] [Google Scholar]
- 2.Kato N, Kinugawa K, Nakayama E, et al. Insufficient self-care is an independent risk factor for adverse clinical outcomes in Japanese patients with heart failure. Int Heart J 2013; 54: 382–389. [DOI] [PubMed] [Google Scholar]
- 3.Riegel B, Lee CS and Dickson VV. Self-care in patients with chronic heart failure. Nat Rev Cardiol 2011; 8: 644–654. [DOI] [PubMed] [Google Scholar]
- 4.Schiff GD, Fung S, Speroff T, et al. Decompensated heart failure: Symptoms, patterns of onset, and contributing factors. Am J Med 2003; 114: 625–630. [DOI] [PubMed] [Google Scholar]
- 5.Buck HG, Harkness K, Wion R, et al. Caregivers’ contributions to heart failure self-care: A systematic review. Eur J Cardiovasc Nurs 2015; 14: 79–89. [DOI] [PubMed] [Google Scholar]
- 6.Buck HG, Mogle J, Riegel B, et al. Exploring the relationship of patient and informal caregiver characteristics with heart failure self-care using the actor-partner interdependence model: Implications for outpatient palliative care. J Palliat Med 2015; 18: 1–7. [DOI] [PubMed] [Google Scholar]
- 7.Clark AM, Reid ME, Morrison CE, et al. The complex nature of informal care in home-based heart failure management. J Adv Nurs 2008; 61: 373–383. [DOI] [PubMed] [Google Scholar]
- 8.Dunbar SB, Clark PC, Quinn C, et al. Family influences on heart failure self-care and outcomes. J Cardiovasc Nurs 2008; 23: 258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pressler SJ, Gradus-Pizlo I, Chubinski SD, et al. Family caregivers of patients with heart failure: A longitudinal study. J Cardiovasc Nurs 2013; 28: 417–428. [DOI] [PubMed] [Google Scholar]
- 10.Trivedi RB, Piette J, Fihn SD, et al. Examining the interrelatedness of patient and spousal stress in heart failure: Conceptual model and pilot data. J Cardiovasc Nurs 2012; 27: 24–32. [DOI] [PubMed] [Google Scholar]
- 11.Archbold PG, Stewart BJ, Greenlick MR, et al. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health 1990; 13: 375–384. [DOI] [PubMed] [Google Scholar]
- 12.Rohrbaugh MJ, Shoham V and Coyne JC. Effect of marital quality on eight-year survival of patients with heart failure. Am J Cardiol 2006; 98: 1069–1072. [DOI] [PubMed] [Google Scholar]
- 13.Rohrbaugh MJ, Shoham V, Cleary AA, et al. Health consequences of partner distress in couples coping with heart failure. Heart Lung 2009; 38; 298–305. [DOI] [PubMed] [Google Scholar]
- 14.Hooker SA, Grigsby ME, Riegel B, et al. The impact of relationship quality on health-related outcomes in heart failure patients and informal family caregivers: An integrative review. J Cardiovasc Nurs 2015; 30: S52–S63. [DOI] [PubMed] [Google Scholar]
- 15.Sebern M and Riegel B. Contributions of supportive relationships to heart failure self-care. Eur J Cardiovasc Nurs 2009; 8; 97–104. [DOI] [PubMed] [Google Scholar]
- 16.Lyons KS, Vellone E, Lee CS, et al. A dyadic approach to managing heart failure with confidence. J Cardiovasc Nurs 2015; 30: S64–S71. [DOI] [PubMed] [Google Scholar]
- 17.Lee CS, Vellone E, Lyons KS, et al. Patterns and predictors of patient and caregiver engagement in heart failure care: A multi-level dyadic study. Int J Nurs Stud 2015; 52: 588–597. [DOI] [PubMed] [Google Scholar]
- 18.Bidwell JT, Vellone E, Lyons KS, et al. Determinants of heart failure self-care maintenance and management in patients and caregivers: A dyadic analysis. Res Nurs Health 2015; 38: 392–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park EO and Schumacher KL. The state of the science of family caregiver-care receiver mutuality: A systematic review. Nurs Inq 2014; 21: 140–152. [DOI] [PubMed] [Google Scholar]
- 20.Trivedi R, Slightam C, Fan VS, et al. A couples’ based self-management program for heart failure: Results of a feasibility study. Front Public Health 2016; 4: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lum HL, Lo DL, Hooker SA, et al. Caregiving in heart failure: Relationship quality is associated with caregiver benefit finding and caregiver burden. Heart Lung 2014; 43: 306–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luttik ML, Jaarsma T, Veeger N, et al. Caregiver burden in partners of heart failure patients; limited influence of disease severity. Eur J Heart Fail 2007; 9: 695–701. [DOI] [PubMed] [Google Scholar]
- 23.Yeh P and Bull M. Use of the resiliency model of family stress, adjustment and adaptation in the analysis of family caregiver reaction among families of older people with congestive heart failure. Int J Older People Nurs 2012; 7: 117–126. [DOI] [PubMed] [Google Scholar]
- 24.Cook WL and Kenny DA. The actor-partner interdependence model: A model of bidirectional effects in developmental studies. Int J Behav Dev 2005; 29: 101–109. [Google Scholar]
- 25.Riegel B, Dickson VV and Faulkner KM. The situation-specific theory of heart failure self-care: Revised and updated. J Cardiovasc Nurs 2016; 31: 226–235. [DOI] [PubMed] [Google Scholar]
- 26.Bekelman DB, Allen LA, Peterson J, et al. Rationale and study design of a patient-centered intervention to improve health status in chronic heart failure: The Collaborative Care to Alleviate Symptoms and Adjust to Illness (CASA) randomized trial. Contemp Clin Trials 2016; 51: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spertus JA and Jones PG. Development and validation of a short version of the Kansas City Cardiomyopathy Questionnaire. Circ Cardiovasc Qual Outcomes 2015; 8: 469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lyons KS, Sayer AG, Archbold PG, et al. The enduring and contextual effects of physical health and depression on caredyad mutuality. Res Nurs Health 2007; 30: 84–98. [DOI] [PubMed] [Google Scholar]
- 30.Sebern MD. Psychometric evaluation of the Shared Care Instrument in a sample of home health care family dyads. J Nurs Meas 2005; 13: 175–191. [DOI] [PubMed] [Google Scholar]
- 31.Morrow CD, Smentkowski K, Schwartz S, et al. Does spouse participation influence quality of life reporting in patients with Parkinson’s disease? Qual Life Res 2015; 23: 245–249. [DOI] [PubMed] [Google Scholar]
- 32.Godwin KM, Swank PR, Vaeth P, et al. The longitudinal and dyadic effects of mutuality on perceived stress for stroke survivors and their spousal caregivers. Aging Ment Health 2013; 17: 423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riegel B, Lee CS, Dickson VV, et al. An update on the self-care of heart failure index. J Cardiovasc Nurs 2009; 24: 485–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vellone E, Riegel B, Cocchieri A, et al. Validity and reliability of the caregiver contribution to self-care of heart failure index. J Cardiovasc Nurs 2013; 28: 245–255. [DOI] [PubMed] [Google Scholar]
- 35.Bédard M, Molloy DW, Squire L, et al. The Zarit Burden Interview: A new short version and screening version. Gerontologist 2001; 41: 652–657. [DOI] [PubMed] [Google Scholar]
- 36.Hu L and Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling 1999; 6: 1–55. [Google Scholar]
- 37.Baron RM and Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1985; 51: 1173–1182. [DOI] [PubMed] [Google Scholar]
- 38.MacKinnon DP. Introduction to statistical mediation analysis. Mahwah, NJ: Erlbaum, 2008. [Google Scholar]
- 39.Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S (ed.) Sociological methodology. San Francisco: Jossey-Bass, 1982, pp.290–312. [Google Scholar]
- 40.Norris AE. Path analysis. In: Munro BH (ed.) Statistical models for health care research. Philadelphia, PA: Linnincott Williams & Williams, 1997, pp.342–367. [Google Scholar]
- 41.Faul F G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39: 175–191. [DOI] [PubMed] [Google Scholar]
- 42.Graven LJ and Grant JS. Social support and self-care behaviors in individuals with heart failure: An integrative review. Int J Nurs Stud 2014; 51: 320–333. [DOI] [PubMed] [Google Scholar]
- 43.Gallagher R, Luttik M and Jaarsma T. Social support and self-care in heart failure. J Cardiovasc Nurs 2011; 26: 439–445. [DOI] [PubMed] [Google Scholar]
- 44.Salyer J, Schubert CM and Chiaranai C. Supportive relationships, self-care confidence, and heart failure self-care. J Cardiovasc Nurs 2012; 27: 384–393. [DOI] [PubMed] [Google Scholar]
- 45.Holahan CK, Holahan CJ and Suzuki R. Purposiveness, physical activity, and perceived health in cardiac patients. Disabil Rehabil 2008; 30: 1772–1778. [DOI] [PubMed] [Google Scholar]
- 46.Homan KJ and Boyatzis CJ. Religiosity, sense of meaning, and health behavior in older adults. Int J Psychol Relig 2010; 20: 173–186. [Google Scholar]
- 47.Zhang KM, Dindoff K, Arnold JMO, et al. What matters to patients with heart failure? The influence of non-health-related goals on patient adherence to self-care management. Patient Educ Couns 2015; 98: 927–934. [DOI] [PubMed] [Google Scholar]
- 48.Schnell-Hoehn KN, Naimark BJ and Tate RB. Determinants of self-care behaviors in community-dwelling patients with heart failure. J Cardiovasc Nurs 2009; 24: 40–47. [DOI] [PubMed] [Google Scholar]
- 49.Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marriage Fam 1976; 38: 15–28. [Google Scholar]
- 50.Given CW, Given B, Stommel M, et al. , The caregiver reactions assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health 1992; 15: 271–283. [DOI] [PubMed] [Google Scholar]
- 51.Kang X, Li Z and Nolan MT. Informal caregivers’ experiences of caring for patients with chronic heart failure: Systematic review and metasynthesis of qualitative studies. J Cardiovasc Nurs 2011; 25: 386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]


