Abstract
The perceptions and attitudes of health professionals toward a certain group of society are among the factors affecting the quality of health service. This study aimed to investigate the attitudes of physicians and nurses about ageism in the COVID-19 pandemic. An easy face-to-face survey was used to collect the data. It involves the questions about demographic information and geriatric perspectives, and they were taken from the University of California at Los Angeles Geriatrics Attitudes Scale (UCLA-GAS). In the study, 58.1% of participants were over 35 years old, 76.6% were women, and 50% were physicians out of 308 in total. It was found that most of the participants have worked in inpatient services and intensive care units for the longest time, where the triage issue was the most discussed topic during the pandemic. An average of 75% of the participants stated that they did not witness any ageist attitude in health care provided. In the comparative analyses conducted with the UCLA-GAS sub-dimensions, statistically significant results, which were anti-ageist and prioritized human life, were obtained. In the extraordinary periods such as pandemic, especially physicians should be able to give the treatment without feeling any social or legal concerns during their medical applications with the light of guidelines accepted scientifically, legally, and morally. Thus, health professionals will not only be away from legal concerns such as malpractice but also will not be exhausted mentally and they can provide more sufficient health service by working under these conditions.
Keywords: COVID-19, Ageism, Triage, Geriatrics, UCLA-GAS
Introduction
The worldwide epidemic situation due to the novel coronavirus infection which emerged in Wuhan, China in December 2019, has been declared as a pandemic by the World Health Organization (WHO) in March 2020 with the name of Coronavirus Disease 2019 (COVID-19) [1]. Considerable progress has been achieved in the diagnosis, treatment, and immunization of the disease during the struggle process which started with this declaration. Despite this, the disease still has not been overcome these days and continues to threaten the world with its new variants [2]. In addition to this, the social structure and government facilities of even developed countries have been questioned regardless of the modern medicine facilities of the twenty-first century. The discussions concerning the injustices in health and social service have become even more apparent during the pandemic period in these countries [3]. One of the discussion topics related to this situation was the discrimination against elderly people (ageism) that appeared both in the distribution of limited medical resources and in the social area [4]. Ageism is a type of discrimination against any person or group because of their age, and it can be applied either systematically or unconsciously.
It has been understood that governments did not have a guideline for such extraordinary situations, especially in the first period of the pandemic. One of the most dramatic examples in this field was the discrimination practices against elderly patients related to providing limited medical resources under the cover of “triage” [5]. No plans have been made for the prevention and treatment of diseases, considering the fragility of the elderly individuals [6]. Instead, classifications such as age, occupation, social status, etc., which are contrary to human rights and not based on scientific criteria, were taken into consideration for the distribution of limited medical resources such as ventilators or intensive care unit beds [7, 8]. On the other hand, practices such as lockdowns for elderly people and leaving them to die in the nursing homes have also been occurred [5, 9]. These practices which are pushing them to social isolation have caused illnesses difficult to be cured not only physically but also mentally [4]. Even though elderly individuals should be included in the first vaccination groups due to their fragility and medical conditions, they have been excluded from clinical trials in this regard [10].
These explained conditions put physicians in a difficult situation and many physicians have to make their own decisions about the use of limited resources. This situation places a heavy burden on physicians, and it also causes them to worry whether they will be held responsible for judicial and administrative aspects in the post-pandemic period or not [11, 12]. This feeling of being under pressure of the physicians has also led to increase their malpractice anxiety level in diagnosis and treatment decisions [13].
Ageism, already existing in different segments of the society, has become visible with the pandemic [8]. This study investigated the attitudes toward ageism of health workers, who actively provided services to two pandemic hospitals, and the effects on the distribution of their services. In addition, the effect of their current attitudes on the distribution of limited medical resources was also examined and discussed in terms of their judicial and legal responsibilities.
Materials and methods
The study population includes participants who were physicians and nurses working at Tepecik Training & Research Hospital in the University of Health Sciences and Bornova Turkan Ozilhan State Hospital. The hospitals were in the city of Izmir, located on the Aegean coast of the Republic of Turkey. Izmir is the third biggest city in the country, with a population of 4.321 million people and is a cosmopolitan metropolis with a secular and high socio-cultural structure. These hospitals were one of the most extensive health institutions in the country with 1120 inpatient beds in total. They were also one of the first hospitals assigned as a “pandemic hospital” after the pandemic declaration. 1150 physicians, 1042 nurses and 232 midwives overall 2424 health professionals were working in these hospitals. This study focused on 440 nurses and 370 doctors (810 people in total) from different units during the pandemic period among the total staff of the hospitals. It was aimed to reach the minimum of 160 nurses and 136 physicians (296 people in total) with the power analysis conducted according to the groups, in accordance with 80% of power range. No randomization method or specific selection was carried out during the recruitment of the participants. It was planned to reach the minimum aimed number of participants through repeated visits to the relevant units in different periods. Despite the extensive literature on healthcare during the COVID-19 pandemic, it was planned to limit the article only to references directly related to the study, in order not to depart from the specific field of the subject. The research was started after getting ethics board approval numbered 2020/5-5 and dated 27/04/2020. In this cross-sectional study, data were collected between December 25, 2020 and January 25, 2021.
The survey forms, which were prepared before the research, were used as a data collection method. They were applied face-to-face to all participants by the same researcher for the reliability of the answers. Participants were informed about the study, and their consent was taken before they filled the survey. The identities of the participants were not included in the documents. A survey form consisting of two parts was given to the participants. The first part contained 10 questions about the experiences of the participants in the pandemic period and their demographic information, while the second part contained 14 questions from the University of California at Los Angeles Geriatrics Attitudes Scale (UCLA-GAS) [14]. These 14 items were measured on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Five items were positive and other nine were negative items. Scores of the negative items were reversed to calculate the total score which can range from 14 to 70. A higher score indicated a positive attitude of participants toward older people. The positive attitude acceptance level was considered as > 3.00 for the UCLA-GAS scores. Total four sub-dimension of the scale consisted of social values, medical care, compassion, and resources distribution aspects [15]. Total attitude score included the combination of these four aspects. Having the score of aspects or the total score of scale above three points was considered as a positive attitude. UCLA-GAS adaptation study for the healthcare providers in our country was applied in 2012 [16] and documented consent was taken from the scale developer before the research began.
Statistical analysis
The distribution of scale scores was analyzed using the Shapiro–Wilk test and normality graphics. The median was summarized by IQR. Frequency (%) was given for categorical variables such as age group, gender, etc. Pearson chi-square test and Fisher-Freeman-Halton chi-square test were used to analyze the answers according to the demographic characteristics of the participants. According to the answers given to these questions in the first part of the study, the Mann–Whitney U test or the Kruskal–Wallis test was used in the comparison done with UCLA-GAS scores. The stepwise step-down approach, proposed by Campbell-Skillings, was performed as a post hoc test after the Kruskal–Wallis test, when necessary. Then, it was determined with the stepwise step-down method suggested by Campbell and Skillings [17]. The consistency of the responses given to the scale was evaluated by using Cronbach α coefficient. The answers were accepted as unreliable with the Cronbach α score between 0.0 and 0.40, low reliable between 0.40 and 0.60, quite reliable between 0.60 and 0.80, and highly reliable between 0.80 and 1.00. The p value was accepted as < 0.05 for the statistical significance level.
For making the statistical analysis, IBM SPSS Statistics 22.0 (IBM Corp. Released 2013 IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.) program was used.
Results
We found that 41.9% (n = 129) of the 308 health professionals participating in the study were under 35 years old, 76.6% (n = 236) of them were female, 62.7% (n = 193) of them were married, and half of them (n = 154) were physicians. Moreover, 57.5% (n = 177) of the participants stated that they have lived with an elderly person before, meanwhile, the majority of these participants consisted of the individuals over 35 years with the rate of 59.3% (n = 105). The rate of participants, stating that they received a geriatric education before, was 20.1% (n = 62). The majority of these 62 participants who have received a geriatric education before were nurses with the rate of 56% (n = 35). In addition, the rate of these educated people according to their professions was 22.7% for nurses and it was limited to 17.5% for physicians. Other demographic characteristics of the participants are given in Table 1.
Table 1.
Demographic information of the participants
| Variables (n = 308) | n (%) | Variables (n = 308) | n (%) |
|---|---|---|---|
| Age | Occupation | ||
| 22–34 years | 129 (41.9) | Nurse | 154 (50.0) |
| 35–65 years | 179 (58.1) | Resident | 56 (18.2) |
| Gender | General practitioner | 10 (3.2) | |
| Female | 236 (76.6) | Specialist | 75 (24.4) |
| Male | 72 (23.4) | Associate professor | 9 (2.9) |
| Professor doctor | 4 (1.3) | ||
| Marital status | Receiving geriatric education | ||
| Married | 193 (62.7) | Yes | 62 (20.1) |
| Single | 115 (37.3) | No | 246 (79.9) |
| Living with elderly relatives | The unit served the COVID-19 cases for the longest time | ||
| Yes | 177 (57.5) | Emergency service | 33 (10.7) |
| No | 131 (42.5) | Polyclinic | 53 (17.2) |
| Inpatient service | 165 (53.6) | ||
| Intensive care unit | 57 (18.5) |
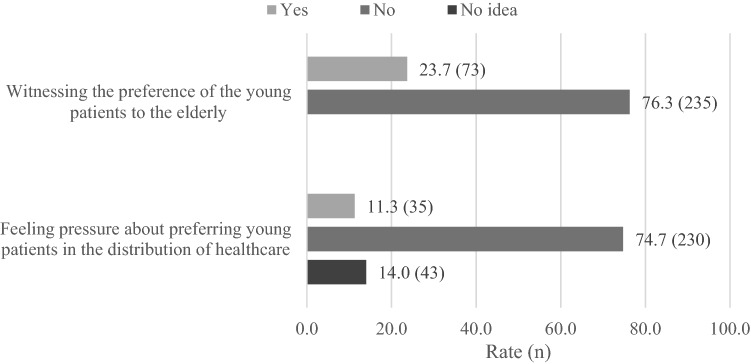
We also found that 23.7% (n = 73) of 308 participants stated that they witnessed that young patients were preferred rather than elderly patients when they receive healthcare services or are hospitalized in intensive care units during the pandemic. On the other hand, 11.3% of the participants (n = 35) stated that they felt pressure about preferring young patients to elderly patients in the distribution of limited medical resources (Fig. 1).
Fig. 1.
Answers about the healthcare services during the pandemic
We determined that 31.0% (n = 40) of participants under 35 years and 18.4% (n = 33) of participants over 35 years witnessed that young patients were preferred than elderly patients during the pandemic and a statistically significant difference was found between the ratios (p = 0.010, Table 2). The rate of answering yes to the same question was higher in participants who were single, physicians, have less than 10 years of professional experience and have received geriatrics education (p < 0.05). The rate of those stating that they feel pressure about preferring young patients in the distribution of limited medical resources was significantly higher in participants under 35 years and physicians (p < 0.05, Table 2).
Table 2.
Answers about the healthcare services during the pandemic according to demographic
| Witnessing the preference of the young patients to the elderly patients | Feeling pressure about preferring young patients in the allocation of scarce medical resources | ||||||
|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Have no idea | |||
| n (%) | n (%) | p-value* | n (%) | n (%) | n (%) | p-value* | |
| Age | 0.010 | 0.007 | |||||
| < 35 years | 40 (31.0) | 89 (69.0) | 23 (17.8)1 | 92 (71.3) | 14 (10.9) | ||
| ≥ 35 years | 33 (18.4) | 146 (81.6) | 12 (6.7)1 | 138 (77.1) | 29 (16.2) | ||
| Gender | > 0.999 | 0.419 | |||||
| Female | 56 (23.7) | 180 (76.3) | 29 (12.3) | 172 (72.9) | 35 (14.8) | ||
| Male | 17 (23.6) | 55 (76.4) | 6 (8.3) | 58 (80.6) | 8 (11.1) | ||
| Marital status | 0.032 | 0.495 | |||||
| Married | 38 (19.7) | 155 (80.3) | 20 (10.4) | 143 (74.1) | 30 (15.5) | ||
| Single | 35 (30.4) | 80 (69.6) | 15 (13.0) | 87 (75.7) | 13 (11.3) | ||
| Living w elderly relatives | 0.797 | 0.339 | |||||
| Yes | 41 (23.2) | 136 (76.8) | 17 (9.6) | 132 (74.6) | 28 (15.8) | ||
| No | 32 (24.4) | 99 (75.6) | 18 (13.7) | 98 (74.8) | 15 (11.5) | ||
| Occupation | < 0.001 | < 0.001 | |||||
| Nurse | 23 (14.9) | 131 (85.1) | 3 (1.9)1 | 127 (82.5)2 | 24 (15.6) | ||
| Physician | 50 (32.5) | 104 (67.5) | 32 (20.8)1 | 103 (66.9)2 | 19 (12.3) | ||
| Receiving geriatric education | 0.035 | < 0.001 | |||||
| Yes | 21 (33.9) | 41 (66.1) | 16 (25.8)1 | 41 (66.1) | 5 (8.1) | ||
| No | 52 (21.1) | 194 (78.9) | 19 (7.7)1 | 189 (76.8) | 38 (15.4) | ||
| The unit served the COVID-19 cases for the longest time | 0.132 | 0.312 | |||||
| Emergency service | 5 (15.2) | 28 (84.8) | 4 (12.1) | 23 (69.7) | 6 (18.2) | ||
| Polyclinic | 9 (17.0) | 44 (83.0) | 7 (13.2) | 36 (67.9) | 10 (18.9) | ||
| Inpatient service | 40 (24.2) | 125 (75.8) | 16 (9.7) | 125 (75.8) | 24 (14.5) | ||
| Intensive care unit | 19 (33.3) | 38 (66.7) | 8 (14.0) | 46 (80.7) | 3 (5.3) | ||
* Statistically significant results are highlighted in bold (p < 0.05)
1,2There is a difference in scores between two related lines shown with the same number (p < 0.05)
The Cronbach α value was found 0.733 for the total of University of California at Los Angeles Geriatrics Attitudes Scale (UCLA-GAS), and the answers to the scale were quite reliable. Internal consistency coefficients were found to be lower for the sub-dimensions of the scale (Table 3).
Table 3.
Internal consistency of UCLA-GAS and sub-dimensions
| Sub-dimensions | Number of items | Cronbach α coefficient |
|---|---|---|
| Social values | 2 | 0.585 |
| Medical care | 4 | 0.514 |
| Compassion | 4 | 0.431 |
| Resources distribution | 4 | 0.512 |
| Total | 14 | 0.733 |
When the UCLA-GAS scores of health professionals were examined, it was determined that all scores were significantly higher (p < 0.05) in participants over 35 years (Table 4). The sub-dimension score of medical care and compassion and also the total score of the scale were higher in married people (p < 0.05). The only sub-dimension in which gender and occupation parameters were found significant was distribution of resources. The score of this sub-dimension was higher in nurses (p < 0.001). All scores were significantly higher in health professionals with more than 20 years of professional experience (p < 0.05). No significant difference was found in the scale scores about receiving geriatric education (p > 0.05). The social values sub-dimension score was significantly higher in the participants working in the inpatient service for the longest time during the pandemic period (p < 0.05). There was a significant difference between the scores indicated by the same numbers. For example, the social values scores differed significantly between professionals who served mostly in emergency services and those in inpatient services. Similarly, there was a significant difference between professionals who worked in inpatient services and those in polyclinics.
Table 4.
Evaluation of UCLA-GAS scores according to the demographic
| Social values | Medical care | Compassion | Resource distribution | Total | |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |
| Age | |||||
| < 35 years | 3.50 (2.50–4.00) | 2.50 (2.00–3.00) | 4.00 (3.38–4.50) | 3.50 (3.00–4.25) | 3.43 (3.04–3.71) |
| 35–65 years | 3.50 (3.00–4.00) | 2.75 (2.50–3.25) | 4.25 (3.75–4.50) | 4.00 (3.50–4.25) | 3.64 (3.36–3.93) |
| p-value | 0.005 | < 0.001 | 0.001 | 0.001 | < 0.001 |
| Gender | |||||
| Male | 3.50 (3.00–4.00) | 2.75 (2.50–3.25) | 4.00 (3.75–4.50) | 4.00 (3.31–4.25) | 3.57 (3.21–3.86) |
| Female | 3.50 (2.63–4.00) | 3.00 (2.25–3.25) | 4.00 (3.75–4.69) | 3.63 (3.06–4.00) | 3.57 (3.09–3.86) |
| p-value | 0.154 | 0.866 | 0.321 | 0.016 | 0.406 |
| Marital status | |||||
| Married | 3.50 (3.00–4.00) | 2.75 (2.50–3.25) | 4.25 (3.75–4.50) | 4.00 (3.50–4.25) | 3.64 (3.36–3.86) |
| Single | 3.50 (2.50–4.00) | 2.50 (2.25–3.00) | 3.75 (3.50–4.25) | 3.75 (3.00–4.25) | 3.50 (3.00–3.79) |
| p-value | 0.086 | 0.004 | < 0.001 | 0.103 | < 0.001 |
| Living w elderly relatives | |||||
| Yes | 3.50 (3.00–4.00) | 2.75 (2.25–3.25) | 4.25 (3.75–4.50) | 4.00 (3.25–4.25) | 3.57 (3.21–3.86) |
| No | 3.50 (3.00–4.00) | 2.75 (2.50–3.25) | 4.00 (3.75–4.50) | 3.75 (3.25–4.25) | 3.57 (3.21–3.86) |
| p-value | 0.809 | 0.531 | 0.151 | 0.319 | 0.409 |
| Occupation | |||||
| Nurse | 3.50 (3.00–4.00) | 2.75 (2.50–3.25) | 4.00 (3.75–4.50) | 4.00 (3.50–4.31) | 3.57 (3.29–3.86) |
| Physician | 3.50 (2.50–4.00) | 2.75 (2.25–3.25) | 4.00 (3.75–4.50) | 3.63 (3.19–4.00) | 3.57 (3.07–3.80) |
| p-value | 0.580 | 0.130 | 0.461 | < 0.001 | 0.072 |
| Receiving geriatric education | |||||
| Yes | 3.50 (2.50–4.00) | 2.88 (2.25–3.25) | 4.00 (3.50–4.25) | 3.75 (3.25–4.25) | 3.54 (3.27–3.79) |
| No | 3.50 (3.00–4.00) | 2.75 (2.50–3.25) | 4.00 (3.75–4.50) | 3.75 (3.25–4.25) | 3.57 (3.21–3.86) |
| p-value | 0.396 | 0.454 | 0.286 | 0.975 | 0.477 |
| The unit served the COVID-19 cases for the longest time | |||||
| Emergency service | 3.00 (2.50–3.75)1 | 2.50 (2.25–3.00)1 | 4.00 (3.75–4.50) | 3.75 (3.25–4.00) | 3.21 (3.07–3.71)1 |
| Polyclinic | 3.00 (2.50–4.00)2 | 2.75 (2.38–3.00) | 4.25 (3.75–4.50) | 3.75 (3.00–4.25) | 3.57 (3.07–3.82) |
| Inpatient service | 3.50 (3.00–4.00)1,2 | 3.00 (2.50–3.38)1 | 4.00 (3.75–4.50) | 4.00 (3.50–4.25) | 3.64 (3.36–3.93)1,2 |
| Intensive care unit | 3.50 (3.00–4.00) | 2.50 (2.13–3.25) | 4.00 (3.50–4.50) | 3.75 (3.25–4.25) | 3.50 (3.14–3.71)2 |
| p-value | 0.004 | 0.035 | 0.641 | 0.182 | 0.009 |
| Witnessing the preference of the young patients to the elderly patients | |||||
| Yes | 3.50 (3.00–4.00) | 2.50 (2.00–3.00) | 4.25 (3.75–4.50) | 3.50 (2.88–4.25) | 3.57 (2.86–3.79) |
| No | 3.50 (3.00–4.00) | 2.75 (2.50–3.25) | 4.00 (3.75–4.50) | 4.00 (3.50–4.25) | 3.57 (3.21–3.86) |
| p-value | 0.846 | < 0.001 | 0.096 | 0.006 | 0.105 |
| Feeling pressure about preferring young patients in allocation of scarce resources | |||||
| Yes | 3.00 (2.50–4.00) | 2.50 (2.00–3.00)1 | 4.00 (3.25–4.25)1 | 3.50 (3.00–4.00)1,2 | 3.29 (2.86–3.64)1,2 |
| No | 3.50 (3.00–4.00) | 2.75 (2.50–3.25)1 | 4.13 (3.75–4.50)1 | 3.75 (3.25–4.25)1 | 3.57 (3.21–3.86)1 |
| Have no idea | 3.00 (2.50–4.00) | 2.75 (2.25–3.25) | 4.00 (3.75–4.50) | 4.00 (3.50–4.25)2 | 3.64 (3.29–3.86)2 |
| p-value | 0.268 | 0.045 | 0.013 | 0.008 | 0.006 |
Statistically significant result is highlighted in bold
IQR 1st quarter–3rd quarter
1,2There is a difference in scores between two related lines shown with the same number (p < 0.05)
Discussion
It was seen that 58% of all participants were over 35 years and 57% of the physicians were senior physicians attending as physicians, associate professors and professors when the results of the demographic data were examined (Table 1). 76.6% of the total participants were women, and this rate was 53% between physicians. Despite being a Muslim-majority country, the characteristics of the study population in a secular city were pleasant in terms of taking a part in the business life for women. Based on this, we believe that our research can be a reference for many studies, which will be conducted in developed countries, and can be compared with them.
The rate of the elderly population over 65 years in the country was 9.5% according to the 2020 data of the official statistics institution, and this rate was found even higher (11.82%) in the province of Izmir, where the study was conducted [18]. The majority of the participants (57.5%) in the study stated that they have lived with elderly relatives before. In the light of this information, it was concluded that the majority of our participants consist of individuals who are used to live together with the elderly individuals in society. It was seen that inpatient service and intensive care unit answers were given to the question of the working in the unit for the longest time, with a total rate of 72.1%. Our study was considered as significant in terms of its contribution to the literature, because the majority of the participants have worked in these two units, where ageism was the most prevalent during the pandemic, for the longest time [4]. Findings such as familiarity of the participants with elderly individuals and working in the units, in which ageism exists, were considered as remarkable in terms of discussions about the results.
When the responses regarding the distribution of limited medical resources were analyzed, it was recognized that the answers were very close to each other (76.3 to 74.7%) and were negative to the questions of witnessing the preference of the young patients to the elderly patients and feeling pressure about giving priority to young patients (Fig. 1). This finding was evaluated as ageism or official/social pressure applied in this way during health service delivery is relatively rare. Besides, the results in which the rates were found so close to each other was evaluated positively in point of the consistency. When the answers were compared with the demographic data, the significant results (p < 0.05) were found in five parameters out of eight. These parameters are age, marital status, occupation, working time in the profession, and receiving geriatric education (Table 2). Ageism which have already existed before has become visible and the ideas on the preference of young patients in the treatments have taken a place even in the academic field with the pandemic period [19, 20]. The answers against ageism given by our population were pleasant when we consider the fact that the negative attitude of health professionals toward the elderly individuals affects their care and treatment adversely in the literature [21, 22].
Physicians were stuck in a difficult situation professionally due to the decisions they made during the uncertain period, especially at the beginning of the pandemic because of the failure to implement a guideline for treatment and triage by the authorities [3, 11]. Moreover, also in legal terms, they hesitated from being prosecuted or undergone an administrative investigation on issues such as a neglect of public service or misconduct of physician job, and they were mentally exhausted [12, 13]. In our study, it is noteworthy that physicians' values were significantly lower than nurses' in the comparative analysis of the questions about pandemic experiences with the occupation parameter (Table 2). The triage hesitancy of physicians, who have the main responsibility in decision-making and treatment processes, about the elderly patients is more prevalent and this situation was evaluated as same as the literature on the first period of the pandemic. On the other hand, with this finding obtained from our study, we believe that the pandemic was also informative about how health professionals have changed their approach. Meanwhile, there is information in the pre-pandemic literature about nurses, who have low or medium level of positive attitudes toward older patients and physicians who have more positive attitudes [23, 24].
When the analyses related to the UCLA-GAS scale, which is the second part of our study, were evaluated, the internal consistency (Cronbach α) value for the total scale was found as 0.733 (Table 3). This value was found as 0.76 in the original study in which the scale was developed [14] and 0.67 in the Turkish validity-reliability study [16]. When we consider the results of these referenced studies and also accept the minimum level as 0.70 for this value academically, it was concluded that the value of 0.733 we obtained was quite adequate. Consisting of the small number of items in sub-dimensions was predicted as the reason for the decrease in internal consistency values during the sub-dimensions of scale process. One of the considerable result of our study was that the UCLA-GAS total score and the scores of aspects in the sub-dimensions were higher than the positive attitude acceptance level and the results were generally significant (p < 0.05) in comparisons with demographic parameters (Table 4).
Participants over 35 years gave negative answers to ageism with a higher rate in both groups about two questions related to the distribution of limited medical resources during the pandemic (Table 2) and UCLA-GAS (Table 4). Although it is accepted that these participants are over 35 years and also come from the generation without geriatric awareness or education, it is noteworthy that the responses received from them were highly anti-ageism. In addition to the validity and reliability study of UCLA-GAS conducted in our country [16], it was determined that the results obtained from the studies conducted with health professionals in different countries such as Sweden [25], Saudi Arabia [26] and China [27] were similar to our results. This situation was evaluated that health professionals are more sensitive to ageism as they get more professional experience and they get older.
The rate of participants who had geriatric education was found to be as low as 20.1%, but even lower in the physician population, dramatically. It has been now accepted that geriatric education should be included in the compulsory curriculum not only in the internal medicine residency period but also in every field interrelating with the elderly individuals, including medicine, nursing and physiotherapy [25, 28]. Furthermore; the effective role of including this education in the post-graduate period has also been mentioned for reducing the ageist mentality [23, 29]. In our study, no significant results were found in the comparison of the receiving geriatric education parameter and any sub-dimension score (Table 4). The reason for this situation was thought as the effect of disproportion due to the quite high rate (79.9%) of participants who have not received geriatric education.
Though the comparative analyses of the findings with the parameter of living with an elderly person were reasonable in two parts of the study, the results were not significant. On the other side, in a study conducted with UCLA-GAS in 2012, the result was positive but not significant similarly to our study [16], and even in different studies conducted in 2015 and 2017, it was found that health professionals have negative attitudes [30, 31]. Considering these cited studies, our result was evaluated as the reflection of present-day individualized human perspective on this subject. As a matter of fact, the majority (n = 177) of those, who answered yes to only this parameter, were participants (n = 105) over 35 years, and this result supports our prediction.
In comparison with the parameter of the working in the unit for the longest time in the pandemic, the total scale score was also found significant as well as the scores of social values and medical care aspects (Table 4). It was considered precious that these two aspects were found significant in those working in the inpatient services and intensive care units where the highest rate of discrimination cases occurred during the pandemic in terms of the attitude of our population toward the elderly patients. The scores of positive attitudes were found higher in the population who responded against ageism in the comparison of the result of the first part of the study and the UCLA-GAS scores (Table 4). This result was remarkable in terms of the consistency and significance of the answers for different scales. The differences about the significance of the two parameters related to the pandemic were seen in the compassion aspect and the total scale score. The most significant results were found in the medical care and resources distribution aspects, and the least significant result was found in the social values and compassion aspects when the results of the UCLA-GAS scale were examined in general. It is precious that there were significant results found in five out of ten parameters in the total scale score and all total scores for all parameters were higher than the positive attitude threshold (> 3.00), according to the positive attitude of the participants toward the elderly patients. Since there are no comparative analyses with the sub-dimensions of the scale in the literature, it was not possible to be discussed about this situation in the literature same as in our study. In this context, we believe that our study will enable new discussions with this contribution to the literature.
Ageism practices for the elderly individuals in the pandemic were faced also in the social life because of the lack of being seriously opposite by governments and medical authorities [5, 9]. This othering circumstance, which is being created with the excuses that elderly people are more contagious in social life, has let them many physical and mental illnesses by pushing them to the social isolation [32, 33]. Also in our study, the comparison of the social values aspect of UCLA-GAS with the scores of all parameters was found as a part of the positive attitude threshold (> 3.00) (Table 4). On the other hand, the least significant result was obtained in this sub-dimension when it was compared to all parameters (Table 4). This situation was evaluated that our participants might have had hesitations about elderly integration into society no matter that they did not have an attitude on the social isolation of the elderly individuals in the pandemic. Besides to this, the data based on the problems faced by the elderly especially in palliative care units [34, 35] were remarkable and the data about deaths of the elderly age group, which happen mostly in the nursing homes due to COVID-19, were also considerable [36]. In the consideration of our findings in this sub-dimension, the importance of post-graduate education of health professionals has been understood very clearly and the authorities should take more active roles. The social values parameter was the sub-dimension with the least significant result in general. However, it was remarkable that the parameter of the working in the unit for the longest time in the pandemic was found significant in this sub-dimension. When we consider that the highest score was found in intensive care unit and inpatient services, it was evaluated that these participants, who looked after the elderly individuals in difficult conditions, realized how important it is to reintegrate these patients into society after they recover, in this single parameter, which was found to be significant.
One of the most discussed issues since the beginning of the pandemic was the fair distribution of limited medical resources such as intensive care unit beds or ventilators [37]. Discussions, in which many discriminatory views toward the elderly individuals were supported by considering only the chronological age [38], were held on this issue under cover of “triage”, and some hypotheses were put forward [19, 39]. But there have also been ethical views supporting the idea that triage should be based on the expected response from the treatment, the benefit to the patient, and the expected survival with scientific facts despite these discriminatory views [5, 40]. Also in our study, it was seen that opinions against ageism were the major thoughts in both the answers to the questions about the pandemic experiences (Fig. 1), and the questions about UCLA-GAS (Table 4) and most of the results were statistically significant.
Summary
In this study, statistically significant results were found in the comparative analyzes between the questions about the pandemic experiences and the UCLA-GAS score, especially in the parameters related to medical treatment, including medical care and resource distribution. As it can be understood from here, the perceptions and attitudes of health professionals about ageism are the factors that may affect the quality of health care provided to elderly individuals. Also, it was remarkable that nearly one in four participants stated that they witnessed ageism in the questions about the pandemic experiences. This dramatic finding also demonstrates that national and international authorities should play an active role against discrimination attitudes such as ageism, which become more apparent in extraordinary periods like pandemic. Another notable result was that nearly 80% of the health professionals in this research did not get any education in the geriatric field and this rate was especially low among the physicians. Educations in this field should be compulsory at the medicine schools and for allied health professions dealing with the elderly individuals and they should be included even in the national curriculum of the countries. Post-graduate educations of health professionals, especially those working in the units dealing with the elderly such as nursing homes or palliative care, should be generalized by updating it in the light of developed medical literature. Moreover, participation to the educations or actions carried out on these subjects should be a prerequisite for individuals who are going to work in these units.
It is very important for professionals working in this field to be aware, as well as to be able to provide fair health services with algorithms of scientific and ethical principles. In this way, guidelines which are agreed on the medical and social field should be arranged for follow-up and treatment. While creating guidelines in this field, academic researches which are performed with internationally recognized scales such as UCLA-GAS can be used. Research such as this study, in which statistically significant and self-consistent results were obtained, will contribute to these processes. Committees should be established in certain health centres under the circumstances for which health professionals may need support in practice despite these current defined standards. These committees should consist of physicians from different departments who can provide the necessary support to health professionals on decisions such as treatment planning and triage. Legal medicine specialists and jurists should also take a part in the formation process of both the guidelines and the committees. Thus, health professionals will feel safer in their medical applications, both judicially and administratively. In this study, results about the triage hesitancy were found to be higher among the physicians, who have the primary responsibility in decision-making and treatment processes. This finding also supports that there is a requirement in this field.
These medical planning done by academic and state authorities have more important place in the periods when the fair distribution of limited medical resources is in question. In these periods, it is not always possible to provide the traditional "first come, first served" application, and criteria such as chronological age, social status, or occupation should not be a priority while algorithms for follow-up, treatment, and triage are being organized. Instead of these criteria, the pre-existing diseases of individuals and the living conditions shaped by the habits of smoking, alcohol, substance use, etc. should be taken into consideration and the triage priority should be decided by treatment planning to the expected response. The findings obtained on this subject in the study, the resource distribution sub-dimension was found to be statistically significant in most of the parameters, including the pandemic experiences. As this result indicates, the current sensitivities of the health professionals in this regard should be supported and organized by the authorities.
Health professionals, especially physicians, should not feel themselves under a heavy burden, either conscientiously or legally in the medical decisions made after all these processes. The planning, which is going to be done in this field, should protect health professionals as well as they will surely protect the elderly individuals or other groups of the society who suffer from discrimination. In this study, it is noteworthy that statistically significant results were obtained in the comparative analysis between the occupation parameter and the pandemic experiences, indicating that the physicians were under pressure about triage processes. Therefore, it can be concluded that physicians should be able to give treatment with the help of guidelines accepted scientifically, legally, and morally without any social or legal concerns in their medical applications. Thus, health professionals working under these conditions will not only be away from legal concerns such as malpractice but also will be able to provide more qualified health services and they will not be exhausted mentally as much as they are.
Acknowledgements
None.
Funding
None.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
Ethical approval was obtained from the Izmir University of Health Sciences Tepecik Training and Research Hospital Clinical Research Ethics Committee with the number 2020/5-5.
Informed consent
A detailed informed consent was at the beginning of the survey presented to the participants. Participants were asked to complete the study if they accepted this explanation.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zeynep Altın, Email: zeynpdr@hotmail.com.
Ferat Buran, Email: cudiferat@hotmail.com.
References
- 1.Archived: WHO Timeline - COVID-19, 04/27/2020: World Health Organization; 2020 [Available from: https://www.who.int/news/item/27-04-2020-who-timeline---covid-19] [
- 2.Torjesen I. Covid-19: omicron may be more transmissible than other variants and partly resistant to existing vaccines, scientists fear. Br Med J Publ Group. 2021;2:2. doi: 10.1136/bmj.n2943. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19—implications for the health care system. Mass Med Soc. 2020;2:1483–1488. doi: 10.1056/NEJMsb2021088. [DOI] [PubMed] [Google Scholar]
- 4.Silva MF, Silva DSM, Bacurau AGDM, Francisco PMSB, Assumpção DD, Neri AL, et al. Ageism against older adults in the context of the COVID-19 pandemic: an integrative review. Rev Saude Publica. 2021;5:55. doi: 10.11606/s1518-8787.2021055003082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rueda J. Ageism in the COVID-19 pandemic: age-based discrimination in triage decisions and beyond. Hist Philos Life Sci. 2021;43:1–7. doi: 10.1007/s40656-021-00441-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults—present status and future implications. Lancet. 2015;385:563–575. doi: 10.1016/S0140-6736(14)61462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daniali SS, Rahimi M, Salarvand S. Age discrimination in delivery of health services to old people during COVID-19 pandemic: a scoping review study. J. Gerontol. Geriatr. 2022;2:2. [Google Scholar]
- 8.Monahan C, Macdonald J, Lytle A, Apriceno M, Levy SR. COVID-19 and ageism: How positive and negative responses impact older adults and society. Am Psychol. 2020;2:2. doi: 10.1037/amp0000699. [DOI] [PubMed] [Google Scholar]
- 9.Aronson L. Covid-19 kills only old people. Only? NY Times. 2020;2:22. [Google Scholar]
- 10.Soiza RL, Scicluna C, Thomson EC. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing. 2021;50:279–283. doi: 10.1093/ageing/afaa274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tian YJA. The ethical unjustifications of COVID-19 triage committees. J Bioethic Inquiry. 2021;18:621–628. doi: 10.1007/s11673-021-10132-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen IG, Crespo AM, White DB. Potential legal liability for withdrawing or withholding ventilators during COVID-19: assessing the risks and identifying needed reforms. JAMA. 2020;323:1901–1902. doi: 10.1001/jama.2020.5442. [DOI] [PubMed] [Google Scholar]
- 13.Buran F, Altın Z. Burnout among physicians working in a pandemic hospital during the COVID-19 pandemic. Leg Med. 2021;51:101881. doi: 10.1016/j.legalmed.2021.101881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reuben DB, Lee M, Davis JW, Jr, Eslami MS, Osterweil DG, Melchiore S, et al. Development and validation of a geriatrics attitudes scale for primary care residents. J Am Geriatr Soc. 1998;46:1425–1430. doi: 10.1111/j.1532-5415.1998.tb06012.x. [DOI] [PubMed] [Google Scholar]
- 15.Lee M, Reuben DB, Ferrell BA. Multidimensional attitudes of medical residents and geriatrics fellows toward older people. J Am Geriatr Soc. 2005;53:489–494. doi: 10.1111/j.1532-5415.2005.53170.x. [DOI] [PubMed] [Google Scholar]
- 16.Sahin S, Mandiracioglu A, Tekin N, Senuzun F, Akcicek F. Attitudes toward the elderly among the health care providers: reliability and validity of Turkish version of the UCLA geriatrics attitudes (UCLA-GA) scale. Arch Gerontol Geriatr. 2012;55:205–209. doi: 10.1016/j.archger.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 17.Campbell G, Skillings JH. Nonparametric stepwise multiple comparison procedures. J Am Stat Assoc. 1985;80:998–1003. doi: 10.1080/01621459.1985.10478216. [DOI] [Google Scholar]
- 18.Elders by statistics, 2020: TUIK (Turkish Statistical Institute); 2021 [Available from: https://data.tuik.gov.tr/Bulten/Index?p=Istatistiklerle-Yaslilar-2020-37227] [
- 19.Sprung CL, Joynt GM, Christian MD, Truog RD, Rello J, Nates JL. Adult ICU triage during the coronavirus disease 2019 pandemic: who will live and who will die? Recommendations to improve survival. Crit Care Med. 2020;48:1196. doi: 10.1097/CCM.0000000000004410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323:1773–1774. doi: 10.1001/jama.2020.5046. [DOI] [PubMed] [Google Scholar]
- 21.Lee TW, Ko IS, Lee KJ. Health promotion behaviors and quality of life among community-dwelling elderly in Korea: A cross-sectional survey. Int J Nurs Stud. 2006;43:293–300. doi: 10.1016/j.ijnurstu.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 22.Skirbekk H, Nortvedt P. Inadequate treatment for elderly patients: Professional norms and tight budgets could cause “ageism” in hospitals. Health Care Anal. 2014;22:192–201. doi: 10.1007/s10728-012-0207-2. [DOI] [PubMed] [Google Scholar]
- 23.Liu Y-E, While AE, Norman IJ, Ye W. Health professionals' attitudes toward older people and older patients: a systematic review. J Interprof. Care. 2012;26:397–409. doi: 10.3109/13561820.2012.702146. [DOI] [PubMed] [Google Scholar]
- 24.Mellor P, Greenhill J, Chew D. Nurses' attitudes toward elderly people and knowledge of gerontic care in a multipurpose health service (MPHS) Aust J Adv Nurs. 2007;24:37–41. [PubMed] [Google Scholar]
- 25.Engström G, Fagerberg I. Attitudes towards older people among Swedish health care students and health sare professionals working in elder care. Nurs Rep. 2011;1:2–6. doi: 10.4081/nursrep.2011.e2. [DOI] [Google Scholar]
- 26.Alamri BH, Xiao LD. Health professionals’ knowledge and attitudes toward older people in primary care in Saudi Arabia. Saudi Med J. 2017;38:229. doi: 10.15537/smj.2017.3.19293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lu L, Kao S-F, Hsieh Y-H. Positive attitudes toward older people and well-being among Chinese community older adults. J Appl Gerontol. 2010;29:622–639. doi: 10.1177/0733464809343289. [DOI] [Google Scholar]
- 28.Opsommer E, Chevalley O, Pegito I, Demeulenaere P. Transcultural adaptation and validation of a French version of the University of California, Los Angeles geriatrics attitudes scale (UCLA-GAS-F) Arch Physiother. 2021;11:1–13. doi: 10.1186/s40945-021-00114-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burnes D, Sheppard C, Henderson CR, Jr, Wassel M, Cope R, Barber C, et al. Interventions to reduce ageism against older adults: a systematic review and meta-analysis. Am J Public Health. 2019;109:e1–e9. doi: 10.2105/AJPH.2019.305123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tufan F, Yuruyen M, Kizilarslanoglu MC, Akpinar T, Emiksiye S, Yesil Y, et al. Geriatrics education is associated with positive attitudes toward older people in internal medicine residents: a multicenter study. Arch Gerontol Geriatr. 2015;60:307–310. doi: 10.1016/j.archger.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Seferoğlu M, Yıldız D, Pekel NB, Güneş A, Yıldız A, Tufan F. Attitudes of neurology specialists toward older adults. Aging Clin Exp Res. 2017;29:787–792. doi: 10.1007/s40520-016-0606-6. [DOI] [PubMed] [Google Scholar]
- 32.Beller J, Wagner A. Loneliness, social isolation, their synergistic interaction, and mortality. Health Psychol. 2018;37:808. doi: 10.1037/hea0000605. [DOI] [PubMed] [Google Scholar]
- 33.Smith BJ, Lim MH. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract. 2020;30:3022008. doi: 10.17061/phrp3022008. [DOI] [PubMed] [Google Scholar]
- 34.Rahimi M, Fadayevatan R, Abedi HA. Care instability in nursing homes; a qualitative study. Iran Red Crescent Med J. 2016;18:2. doi: 10.5812/ircmj.21515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levy BR, Ferrucci L, Zonderman AB, Slade MD, Troncoso J, Resnick SM. A culture–brain link: negative age stereotypes predict Alzheimer’s disease biomarkers. Psychol Aging. 2016;31:82. doi: 10.1037/pag0000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Merodio G, Ramis-Salas M, Valero D, Aubert A. How much is one life worth? The right to equity healthcare for improving older patients’ health infected by COVID-19. Sustainability. 2020;12:6848. doi: 10.3390/su12176848. [DOI] [Google Scholar]
- 37.Orfali K. Getting to the truth: ethics, trust, and triage in the United States versus Europe during the COVID-19 pandemic. Hast Cent Rep. 2021;51:16–22. doi: 10.1002/hast.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Archard D, Caplan A. Is it wrong to prioritise younger patients with covid-19? BMJ. 2020;2:369. doi: 10.1136/bmj.m1509. [DOI] [PubMed] [Google Scholar]
- 39.Vergano M, Bertolini G, Giannini A, Gristina GR, Livigni S, Mistraletti G, et al. Clinical ethics recommendations for the allocation of intensive care treatments in exceptional, resource-limited circumstances: the Italian perspective during the COVID-19 epidemic. Crit Care. 2020;24:1–3. doi: 10.1186/s13054-020-02891-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reynolds L. The COVID-19 pandemic exposes limited understanding of ageism. J Aging Soc Policy. 2020;32:499–505. doi: 10.1080/08959420.2020.1772003. [DOI] [PubMed] [Google Scholar]