Abstract
Purpose
To compile and analyze the top 50 most frequently cited articles published on robotic-assisted arthroplasty, allowing clinicians to effectively identify the most influential literature pertaining to this topic.
Methods
Guidelines set by the Preferred Reporting Items for Systematic Reviews were used as the foundation for data collection and analysis. All papers pertaining to robotic-assisted arthroplasty were retrieved using the Scopus database. Data including: manuscript title, authors, total citation count, level of evidence, journal, publication year, and country of publication was extracted from a final list of articles.
Results
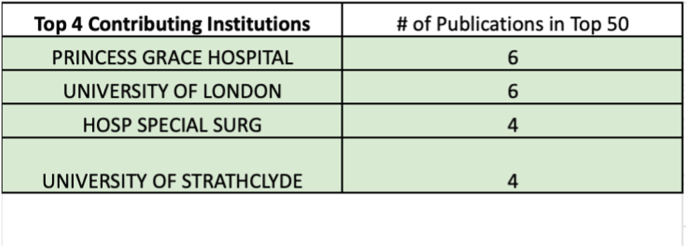
The top 50 publications regarding robotic assisted arthroplasty were cited a total of 4530 times (including self-citations), with an average total of 91. The years with the most publications in the top 50 were: 2017, 2018, and 2019, producing 7, 6, and 5 papers, respectively. Only 4 papers in the top 50 were published prior to the year 2003. The most common level of evidence was level V, and the most common category was Clinical Outcomes (74%). The United States contributed half of the 50 articles, and Princess Grace Hospital and University of London were the most contributory institutions, each with 6 of the top 50 articles.
Conclusion
This analysis provides a comprehensive review of the most cited and influential papers in robotic-assisted arthroplasty. Understanding these trends in the literature will ultimately pave the way for physicians and researchers to continue to innovate and research in a targeted manner as they gain an understanding of what has been studied and what remains inadequately explored.
Level of evidence
3.
Keywords: Robotic surgery, Arthroplasty, Robotic assisted arthroplasty, Bibliometric review
1. Introduction
There are more than 2 million Americans living with a hip replacement today, and that number is expected to rise by 71% by 2030.1,2 As numbers continue to rise, total joint arthroplasty (TJA) continues to be one of the most studied and researched topics in orthopaedics.3 Despite improvement in surgical technique and implant design, there are still risks and complications associated with TJA, including but not limited to implant failure, low patient satisfaction, and challenging postoperative recovery and pain. Robotic assistance continues to grow and evolve as a method to try and address these shortcomings. Robotic technology allows surgeons to minimize potential human errors and optimize accuracy, with the goal of improving clinical outcomes.4
Robotic assistance is an umbrella term used to designated implementation of programmable devices to enhance surgical practices. For example, robotic systems can use CT imaging to reconstruct patient anatomy so that implants can be selected and molded to fit exact patient dimensions.5 Additionally, robotic assistance can come in the form of physical systems used in the operating room. Using the 3D reconstruction of the patient's anatomy, the robotic system can create constraints which limit the surgeon from operating outside of optimal parameters, thus optimizing accuracy.6 Despite the theoretical benefits of robotic assisted joint arthroplasty, there are also associated hindrances inherent to this novel technology. The integration of robotic assisted technology is complex and often adds increased operative time and costs to joint replacements.7
Bibliometric analyses have recently become a more popular tool to evaluate published literature. They allow for easy access to the most influential studies in an area of interest through a cross-sectional examination of the literature. To our knowledge, there are no previous studies that have specifically analyzed the most influential articles related to robotic-assisted arthroplasty.
The purpose of this study is to analyze the most influential literature on robotic-assisted total joint arthroplasty. The analysis will be in the form of a bibliometric review, using number of citations as a measure of influence. This paper is the first in the literature to review the most cited literature on this particular topic.
2. Methods
The database used to accumulate the data for this study was Clarivate Analytics Web of Science (WOS). A literature search was performed using the following search queries: “(Arthroplast* OR joint replacement) AND (robot* OR robot assisted OR robotic arm OR robotic arm assisted)”. The original search yielded a total of 1215 publications. A filter was added to include only articles published in English. The publications were then sorted in descending order from highest to lowest number of total citations. This sorted list was then exported to an excel file for further analysis. A full-text review was conducted on each publication by two authors (RM and JW) until a total of 50 publications were accepted for analysis. Publications were included only if their content pertained specifically to robotic-assisted joint arthroplasty. The top 50 publications that met the inclusion and exclusion criteria were selected for further analysis. A multi-author review was conducted to assign Level of Evidence (LOE) to each publication. The LOE, according to the Oxford Center for Evidence Based Medicine, was assigned using the following guidelines:
-
1
Systematic reviews of randomized trials, or systematic reviews of inception cohort studies.
-
2
Systematic reviews of cohort studies, inception cohort studies, cross-sectional studies, randomized trials, or observational studies with dramatic effect.
-
3
Cohort studies (primarily retrospective), epidemiological/observational study
-
4
Case-control studies, low impact cohort studies, animal trials
-
5
Simulations, models, or mechanism-based reasoning
The publications included in the top 50 analysis were further classified into one of the following categories as determined by the reviewing authors: clinical outcomes, devices/technology, anatomy/biomechanics/physiology, learning curve, and economics. Some publications with overlapping categorization were included in multiple classifications. The total number of citations, citations per year since publication, authorship, year of publication, affiliated institution, and country of origin were also recorded for each publication.
3. Results
As a whole, the top 50 most cited publications in the field of robotic-assisted arthroplasty have been cited 4530 times based on a comprehensive database search which included self-citations. The most cited paper amassed 211 citations in comparison to the least cited paper that was cited 46 total times (Table 1.)
Table 1.
Most cited articles by total number of citations.
| Rank | Publication | Total Citations | Citations/Year of Publication Until 2022 |
|---|---|---|---|
| 1 | Jaramaz B, DiGioia AM, 3rd, Blackwell M, Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop Relat Res. Sep 1998; (354):70–81. https://doi.org/10.1097/00003086-199809000-00010 | 211 | 9 |
| 2 | Cobb J, Henckel J, Gomes P et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. Feb 2006; 88(2):188-97. https://doi.org/10.1302/0301-620X.88B2.17220 | 205 | 13 |
| 3 | Paul HA, Bargar WL, Mittlestadt B et al. Development of a surgical robot for cementless total hip arthroplasty. Clin Orthop Relat Res. Dec 1992; (285):57–66. | 193 | 6 |
| 4 | Delp SL, Stulberg SD, Davies B, Picard F, Leitner F. Computer assisted knee replacement. Clin Orthop Relat Res. Sep 1998; (354):49–56. https://doi.org/10.1097/00003086-199809000-00007 | 167 | 7 |
| 5 | Jacofsky DJ, Allen M. Robotics in Arthroplasty: A Comprehensive Review. J Arthroplasty. Oct 2016; 31(10):2353-63. https://doi.org/10.1016/j.arth.2016.05.026 | 148 | 25 |
| 6 | Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J Bone Joint Surg Am. Apr 20, 2016; 98(8):627-35. https://doi.org/10.2106/JBJS.15.00664 | 145 | 24 |
| 7 | Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. Jan 2013; 471(1):118-26. https://doi.org/10.1007/s11999-012-2407-3 | 138 | 15 |
| 8 | Honl M, Dierk O, Gauck C et al. Comparison of robotic-assisted and manual implantation of a primary total hip replacement. A prospective study. J Bone Joint Surg Am. Aug 2003; 85(8):1470-8. https://doi.org/10.2106/00004623-200308000-00007 | 135 | 7 |
| 9 | Yamazaki T, Watanabe T, Nakajima Y et al. Improvement of depth position in 2-D/3-D registration of knee implants using single-plane fluoroscopy. IEEE Trans Med Imaging. May 2004; 23(5):602-12. https://doi.org/10.1109/tmi.2004.826051 | 131 | 7 |
| 10 | Domb BG, El Bitar YF, Sadik AY, Stake CE, Botser IB. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. Jan 2014; 472(1):329-36. https://doi.org/10.1007/s11999-013-3253-7 | 128 | 16 |
| 11 | Lonner JH, John TK, Conditt MA. Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res. Jan 2010; 468(1):141-6. https://doi.org/10.1007/s11999-009-0977-5 | 125 | 10 |
| 12 | Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. Jul 2011; 19(7):1069-76. https://doi.org/10.1007/s00167-011-1400-9 | 112 | 10 |
| 13 | Lang JE, Mannava S, Floyd AJ et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br. Oct 2011; 93(10):1296-9. https://doi.org/10.1302/0301-620X.93B10.27418 | 106 | 7 |
| 14 | Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty. Oct 2007; 22(7):1054-9. https://doi.org/10.1016/j.arth.2007.05.036 | 106 | 10 |
| 15 | Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. Jul 2018; 100-B(7):930–937. https://doi.org/10.1302/0301-620X.100B7.BJJ-2017-1449.R1 | 104 | 26 |
| 16 | Liow MH, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty. Dec 2014; 29(12):2373-7. https://doi.org/10.1016/j.arth.2013.12.010 | 98 | 8 |
| 17 | Pearle AD, O'Loughlin PF, Kendoff DO. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty. Feb 2010; 25(2):230-7. https://doi.org/10.1016/j.arth.2008.09.024 | 98 | 12 |
| 18 | Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res. Nov 2007; 464:111–6. https://doi.org/10.1097/BLO.0b013e318126c0c0 | 93 | 6 |
| 19 | Citak M, Suero EM, Citak M et al. Unicompartmental knee arthroplasty: is robotic technology more accurate than conventional technique? Knee. Aug 2013; 20(4):268-71. https://doi.org/10.1016/j.knee.2012.11.001 | 91 | 10 |
| 20 | Schulz AP, Seide K, Queitsch C et al. Results of total hip replacement using the Robodoc surgical assistant system: clinical outcome and evaluation of complications for 97 procedures. Int J Med Robot. Dec 2007; 3(4):301-6. https://doi.org/10.1002/rcs.161 | 91 | 6 |
| 21 | Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty. May 2012; 27(5):803-8 e1. https://doi.org/10.1016/j.arth.2011.09.021 | 87 | 9 |
| 22 | Pearle AD, van der List JP, Lee L, Coon TM, Borus TA, Roche MW. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum two-year follow-up. Knee. Mar 2017; 24(2):419–428. https://doi.org/10.1016/j.knee.2016.12.001 | 78 | 16 |
| 23 | Jones CW, Jerabek SA. Current Role of Computer Navigation in Total Knee Arthroplasty. J Arthroplasty. Jul 2018; 33(7):1989–1993. https://doi.org/10.1016/j.arth.2018.01.027 | 76 | 19 |
| 24 | Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: Exploratory secondary analysis of a randomised controlled trial. Bone Joint Res. Nov 2017; 6(11):631–639. https://doi.org/10.1302/2046-3758.611.BJR-2017-0060.R1 | 74 | 15 |
| 25 | Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc. Apr 2019; 27(4):1132–1141. https://doi.org/10.1007/s00167-018-5138-5 | 73 | 24 |
| 26 | Hampp EL, Chughtai M, Scholl LY et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Greater Accuracy and Precision to Plan Compared with Manual Techniques. J Knee Surg. Mar 2019; 32(3):239–250. https://doi.org/10.1055/s-0038-1641729 | 73 | 24 |
| 27 | Marchand RC, Sodhi N, Khlopas A et al. Patient Satisfaction Outcomes after Robotic Arm-Assisted Total Knee Arthroplasty: A Short-Term Evaluation. J Knee Surg. Nov 2017; 30(9):849–853. https://doi.org/10.1055/s-0037-1607450 | 71 | 14 |
| 28 | Moschetti WE, Konopka JF, Rubash HE, Genuario JW. Can Robot-Assisted Unicompartmental Knee Arthroplasty Be Cost-Effective? A Markov Decision Analysis. J Arthroplasty. Apr 2016; 31(4):759-65. https://doi.org/10.1016/j.arth.2015.10.018 | 71 | 12 |
| 29 | Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. Apr 2019; 27(4):1232–1240. https://doi.org/10.1007/s00167-018-5081-5 | 70 | 23 |
| 30 | Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE. High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res. Jan 2015; 473(1):206-12. https://doi.org/10.1007/s11999-014-3764-x | 70 | 6 |
| 31 | Nakamura N, Sugano N, Nishii T, Kakimoto A, Miki H. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res. Apr 2010; 468(4):1072-81. https://doi.org/10.1007/s11999-009-1158-2 | 70 | 10 |
| 32 | 42. Plaskos C, Cinquin P, Lavallee S, Hodgson AJ. Praxiteles: a miniature bone-mounted robot for minimal access total knee arthroplasty. Int J Med Robot. Dec 2005; 1(4):67–79. https://doi.org/10.1002/rcs.59 | 70 | 4 |
| 33 | Bargar WL. Robots in orthopaedic surgery: past, present, and future. Clin Orthop Relat Res. Oct 2007; 463:31–6. | 67 | 4 |
| 34 | Sodhi N, Khlopas A, Piuzzi NS et al. The Learning Curve Associated with Robotic Total Knee Arthroplasty. J Knee Surg. Jan 2018; 31(1):17–21. https://doi.org/10.1055/s-0037-1608809 | 66 | 17 |
| 35 | Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty. Aug 2018; 33(8):2496–2501. https://doi.org/10.1016/j.arth.2018.03.042 | 66 | 17 |
| 36 | Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. Sep 2017; 25(9):2942–2951. https://doi.org/10.1007/s00167-016-4076-3 | 65 | 13 |
| 37 | Wolf A, Jaramaz B, Lisien B, DiGioia AM. MBARS: mini bone-attached robotic system for joint arthroplasty. Int J Med Robot. Jan 2005; 1(2):101-21. https://doi.org/10.1002/rcs.20 | 65 | 4 |
| 38 | Kayani B, Konan S, Pietrzak JRT, Huq SS, Tahmassebi J, Haddad FS. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. Aug 2018; 100-B(8):1033–1042. https://doi.org/10.1302/0301-620X.100B8.BJJ-2018-0040.R1 | 64 | 16 |
| 39 | Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. Jan 2019; 101-B(1):24–33. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0564.R2 | 61 | 20 |
| 40 | Gilmour A, MacLean AD, Rowe PJ et al. Robotic-Arm-Assisted vs Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. J Arthroplasty. Jul 2018; 33(7S):S109–S115. https://doi.org/10.1016/j.arth.2018.02.050 | 60 | 15 |
| 41 | Domb BG, Redmond JM, Louis SS et al. Accuracy of Component Positioning in 1980 Total Hip Arthroplasties: A Comparative Analysis by Surgical Technique and Mode of Guidance. J Arthroplasty. Dec 2015; 30(12):2208-18. https://doi.org/10.1016/j.arth.2015.06.059 | 60 | 9 |
| 42 | Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop. Nov 2017; 41(11):2265–2271. https://doi.org/10.1007/s00264-017-3633-9 | 55 | 11 |
| 43 | Beldame J, Boisrenoult P, Beaufils P. Pin track induced fractures around computer-assisted TKA. Orthop Traumatol Surg Res. May 2010; 96(3):249-55. https://doi.org/10.1016/j.otsr.2009.12.005 | 55 | 5 |
| 44 | Nishihara S, Sugano N, Nishii T, Miki H, Nakamura N, Yoshikawa H. Comparison between hand rasping and robotic milling for stem implantation in cementless total hip arthroplasty. J Arthroplasty. Oct 2006; 21(7):957-66. https://doi.org/10.1016/j.arth.2006.01.001 | 53 | 3 |
| 45 | Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand. Oct 2004; 75(5):573-9. https://doi.org/10.1080/00016470410001448 | 50 | 3 |
| 46 | Yang HY, Seon JK, Shin YJ, Lim HA, Song EK. Robotic Total Knee Arthroplasty with a Cruciate-Retaining Implant: A 10-Year Follow-up Study. Clin Orthop Surg. Jun 2017; 9(2):169–176. https://doi.org/10.4055/cios.2017.9.2.169 | 48 | 10 |
| 47 | Plate JF, Augart MA, Seyler TM et al. Obesity has no effect on outcomes following unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. Mar 2017; 25(3):645–651. https://doi.org/10.1007/s00167-015-3597-5 | 47 | 9 |
| 48 | Hansen DC, Kusuma SK, Palmer RM, Harris KB. Robotic guidance does not improve component position or short-term outcome in medial unicompartmental knee arthroplasty. J Arthroplasty. Sep 2014; 29(9):1784-9. https://doi.org/10.1016/j.arth.2014.04.012 | 47 | 2 |
| 49 | O'Toole RV, 3rd, Jaramaz B, DiGioia AM, 3rd, Visnic CD, Reid RH. Biomechanics for preoperative planning and surgical simulations in orthopaedics. Comput Biol Med. Mar 1995; 25(2):183-91. https://doi.org/10.1016/0010-4825(9400043-p) | 47 | 6 |
| 50 | Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev. Oct 2019; 4(10):611–617. https://doi.org/10.1302/2058-5241.4.190022 | 46 | 15 |
There were 40 unique authors that contributed to the top 50 publications. Kayani what is the most prolific author, contributing six publications out of the top 50 articles (Fig. 1). The year 2017 was the most productive with a total of 7 publications, followed by 2018 with 6 publications and then 2019 which yielded 5 publications. Out of the top 50 papers, only 4 were published before the year 2003 (Fig. 2).
Fig. 1.
Author count.
Fig. 2.
Publication years.
With respect to Level of Evidence (LOE), Level V was the most common level of evidence (n = 14, 28%). This was followed by 13 publications meeting criteria for Level III evidence. Additionally, Level I evidence was represented by four papers, Level II evidence was represented by 10 papers, and Level IV evidence was represented by 9 papers. There were no publications in the top 50 they were unable to be categorized in terms of their Level of Evidence (Fig. 3).
Fig. 3.
Level of evidence.
Most articles published were classified as Clinical Outcomes, with a total of 37 papers, followed by Anatomy/Biomechanics/Physiology with 13 papers and Devices/Technology with 10 publications. Many studies spanned multiple categories of classification and those which encompassed multiple classifications were included in the total count, once for each classification. Each of the top 50 publications fell within our classification system and none of the publications analyzed remained unclassified by the end of the analysis (Fig. 4).
Fig. 4.
Classifications.
Four institutions contributed 20 of the top 50 publications (40%). The top contributors were Princess Grace Hospital and University of London, each with 6 of the top 50 articles. Both the Hospital for Special Surgery and the University of Strathclyde produced 4 publications each (Fig. 5).
Fig. 5.
Top contributing institutions.
The country which produced the most publications was the United States (n = 25), followed by England with 8 publications, and France with 5 publications (Fig. 6).
Fig. 6.
Top contributing countries.
The two most cited articles in this study attained over 200 citations each since being published. The most cited publication, by Jaramaz et al., was cited a total of 211 times. This paper sought to use computer assisted techniques to link preoperative plan, intraoperative acetabular cup placement, with most operative cup measurement in total hip arthroplasty. The next most cited paper, by Cobb et al., amassed a total of 205 citations. This was a prospective, randomized controlled trial of unicompartmental knee arthroplasty comparing the angle of tibiofemoral alignment in the coronal plane, between the Acrobot system and conventional surgery. The third most cited paper in the top 50, by Paul et al., has been cited 193 times. This study aimed to obtain an exact fit for the femoral prosthesis via use of an image-directed surgical robot, particularly for femoral canal preparation (Table 1).
A separate analysis was then performed, evaluating these articles for the amount of citations accrued on a yearly basis since their publication. The top paper was by Kayani et al., which was cited 26 times per year since publication in 2018. This study compared early postoperative outcomes and time to discharge between conventional jig-based total knee arthroplasty (TKA) and robotic-arm assisted TKA (Table 2).
Table 2.
Most cited articles by citations per year.
| Rank | Publication | Total Citations | Citations per Year | Year Published |
|---|---|---|---|---|
| 1 | Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. Jul 2018; 100-B(7):930–937. https://doi.org/10.1302/0301-620X.100B7.BJJ-2017-1449.R1 | 104 | 26 | 2018 |
| 2 | Jacofsky DJ, Allen M. Robotics in Arthroplasty: A Comprehensive Review. J Arthroplasty. Oct 2016; 31(10):2353-63. https://doi.org/10.1016/j.arth.2016.05.026 | 148 | 25 | 2016 |
| 3 | Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc. Apr 2019; 27(4):1132–1141. https://doi.org/10.1007/s00167-018-5138-5 | 73 | 24 | 2019 |
| 4 | Hampp EL, Chughtai M, Scholl LY et al. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Greater Accuracy and Precision to Plan Compared with Manual Techniques. J Knee Surg. Mar 2019; 32(3):239–250. https://doi.org/10.1055/s-0038-1641729 | 73 | 24 | 2019 |
| 5 | Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J Bone Joint Surg Am. Apr 20, 2016; 98(8):627-35. https://doi.org/10.2106/JBJS.15.00664 | 145 | 24 | 2016 |
| 6 | Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. Apr 2019; 27(4):1232–1240. https://doi.org/10.1007/s00167-018-5081-5 | 70 | 23 | 2019 |
| 7 | Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J. Jan 2019; 101-B(1):24–33. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0564.R2 | 61 | 20 | 2019 |
| 8 | Jones CW, Jerabek SA. Current Role of Computer Navigation in Total Knee Arthroplasty. J Arthroplasty. Jul 2018; 33(7):1989–1993. https://doi.org/10.1016/j.arth.2018.01.027 | 76 | 19 | 2018 |
| 9 | Sodhi N, Khlopas A, Piuzzi NS et al. The Learning Curve Associated with Robotic Total Knee Arthroplasty. J Knee Surg. Jan 2018; 31(1):17–21. https://doi.org/10.1055/s-0037-1608809 | 66 | 17 | 2018 |
| 10 | Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty. Aug 2018; 33(8):2496–2501. https://doi.org/10.1016/j.arth.2018.03.042 | 66 | 17 | 2018 |
4. Discussion
The proportion of arthroplasty procedures performed with robotic assistance is increasing annually.8, 9, 10 A retrospective study identified 321,522 patients who underwent primary hip or knee arthroplasty from 2008 to 2015 and found that the proportion of technology assisted arthroplasty increased annually and grew from 2.8% in 2008 to 8.6% in 2015.8 Moreover, between 2008 and 2015, the proportion of hospitals and surgeons utilizing technology assistance increased from 16.2% to 29.2% and 6.2%–17.1%, respectively.8 The growth continues to increase as literature continues to show improved outcomes of robotic-assisted arthroplasty in comparison to conventional techniques.5,11, 12, 13
One systematic review involving 1516 patients found reduced complication rates in patients who underwent robotic assisted total hip arthroplasty (THA) compared to those who underwent conventional THA.12 Robotic-assisted THA was found to have statistically lower intraoperative complications rates (OR: 0.12, 95% CI: 0.05 to 0.34, p < 0.0001) and better cup and stem placement.12 Moreover, the total complication rates (intraoperative and postoperative) were higher in patients who underwent conventional THA (OR: 0.43, p = 0.03).12 Superior radiographic outcomes were also reported in patients who underwent robotic assisted THA compared to those who underwent conventional THA, including reduced rates of stem alignment outliers (p = 0.022),14 higher rates of ideal cup placement as defined by Lewinnek's/Callanan's Safe Zone (OR: 5.64, p < 0.00001),15,16 and lower rates of heterotopic ossification (OR: 1.91, p = 0.04). They found no difference in functional outcomes scores.12
Similarly, another systematic review involving 1199 patients who underwent robotic versus conventional total knee arthroplasty (TKA) revealed improved accuracy, precision, and alignment in the robotic-assisted group across multiple studies.13 This included a significant reduction in mechanical axis outliers (0% vs 24%; p < 0.001) and markedly superior outcomes of tibiofemoral alignment with one study showing only 1 of 70 patients with deviation from the planned angle (4°) versus 18 of 52 patients in the conventional group with deviations >3°–7° (p < 0.0001).17,18 Improved quality of life measures were also noted in a 2-year follow up of a prospective randomized control trial comparing patients who underwent robotic versus conventional TKA, reporting a better SF-36 general health at 6 months (p = 0.04) and a better SF-36 vitality (p = 0.03) and role emotional (p = 0.02) at 2 years postoperatively.11
In addition to emerging evidence of improved outcomes, robotic-assisted arthroplasty is economically advantageous, with multiple studies showing reduced costs, lengths of stay, and utilization of services in patients undergoing robotic-assisted arthroplasty in comparison to the conventional approach.19, 20, 21 For example, one retrospective study analyzing a total of 2142 patients found a length of stay of nearly a day less (1.80 vs 2.72 days; p < 0.0001), reduced utilization of skilled nursing facilities (1.68% vs 6.05%; p < 0.0001) and inpatient services (2.24% vs 4.37%; p = 0.0444), reduced home health days (5.33 vs 6.36; p = 0.0037), and a reduced 90-day payer cost ($28,204 vs $32,253 p < 0.0001).21 Overall, as outcomes continue to improve and advances in technology continue to develop, further research is indicated in this promising topic.22,23
The most cited paper, by Jaramaz et al., cited a total of 211 times, discusses the influence of image guided systems on preoperative planning and post-operative biomechanical outcomes in THA.24 This study utilized the HipNav system, containing both preoperative planning and intraoperative guidance components. Although the sample size was too small for statistical analysis (n = 8), in all cases, the HipNav demonstrated improved orientation and cup placement in comparison to mechanical guidance in hip arthroplasty.24 This was defined by the final cup position achieved in degrees of abduction and flexion in comparison to the preoperative plan.24 The paper was published in 1998, one of the earliest published articles discussing this topic.
The second most cited paper, by Cobb et al., gained a total of 205 citations. This randomized control trial, published in 2006, examined outcomes of tibiofemoral alignment in 27 patients undergoing Acrobot device-assisted versus conventional unicompartmental knee arthroplasty.25 Surgeons were able to more reliably execute a pre-operative plan with robotic-assistance.25 Moreover, all patients in the Acrobot group achieved a tibiofemoral alignment within 2° of the planned position, compared to only 40% of the conventional group achieving this level of accuracy (p = 0.001).25 Furthermore, differences in functional scores were noted using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and American Knee Society (AKS) scores.25 The mean pre-to post-operative increase in AKS score was two times greater in the Acrobot group (65.2 vs 32.5) and the median value was more than three times as high (62 vs 19) (p = 0.004) (16434522). On the WOMAC, although superior scores of pain, stiffness, and physical function were achieved in the Acrobot group, this difference was not statistically significant (p = 0.06).25
The most common level of evidence (LOE) amongst the cited articles was level 5, comprising 14 of the 50 papers, followed closely by level 3, representing 13 articles. There is a current lack in higher quality research currently being cited in today's literature on robotic-assisted arthroplasty. In comparison, bibliometric reviews evaluating conventional arthroplasty techniques tended to show studies with higher levels of evidence. For example, a bibliometric analysis on total hip arthroplasty from 2019 found a relatively even distribution of level II, III, and IV as the most common levels of evidence.26 Similarly, a bibliometric analysis on unicondylar knee arthroplasty found level III and IV evidence to be the most common categories.27 One explanation for this is that these techniques have been utilized for longer, allowing more time for higher quality research to develop. In our analysis, 4 papers were level 1 evidence, further supporting the need for higher quality research discussing robotic-assisted arthroplasty.
The most contributing country to robotics arthroplasty research was the United States, representing 50% of the top 50 articles, followed by England at 16%. A medical market and technology report on United States and European markets for joint arthroplasty products found that in 2015, the United States had more than double the volume of hip arthroplasty procedures than Germany, the next highest ranked country in the report.28 This gap widened in 2016 and thereafter, with a predicted output of more than 3 times that of Germany in 2020.28 More profoundly, for knee arthroplasty procedures, in 2015 the United States was found to have well over 4 times the volume of procedures compared to Germany.28 This gap similarly widened, with a forecast of nearly 5 times the volume of procedures in 2020.28 This trend is likely to continue as multiple models reveal a rapidly increasing volume of arthroplasty procedures in the United States.2,29
This analysis contributes valuable information to the literature as it identifies the current trends in robotic-assisted arthroplasty research. Nevertheless, there are some limitations present in this bibliometric review. For one, it is possible that some papers in the field were missed as we only evaluated peer-reviewed articles. Secondly, manuscripts that have been published at an earlier date may have more citations simply because they have been available in the literature for longer. This raises the question if citations alone can adequately determine influence. To overcome some of these limitations, a citation density was performed showing how many times an article was cited per year and the LOE for each publication was provided. These metrics provide a more comprehensive understanding of the research being presented and provide nuance in assessing quality.
5. Conclusion
This study highlights the top 50 most cited articles in robotic-assisted knee and hip arthroplasty. The most prevalent study category was clinical outcomes (74%), and the most common levels of evidence were V (28%) and III (26%). 70% of the articles were published after 2010, reflecting the recent growth of this relatively young field. The United States contributed half of the cited articles followed by England and France. This analysis provides researchers and physicians easy access to the most cited and influential papers in robotic-assisted arthroplasty.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Authors contribution
Rami H. Mahmoud: conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing – original draft, writing – review and editing, visualization, supervision, project administration. Juan J. Lizardi: methodology, investigation, resources, data curation, writing – original draft, writing – review and editing Jonathan Weinerman: investigation, resources, data curation, writing – original draft, writing – review and editing, visualization Dennis J. Vanden Berge: conceptualization, methodology, validation, resources, writing – review and editing, visualization, supervision, project administration. David S. Constantinescu: conceptualization, methodology, validation, resources, visualization, supervision, project administration. Ramakanth Yakkanti: conceptualization, methodology, validation, supervision.
Author contributions
All authors participated in the study and helped shape the research question, data, analysis, and manuscript.
Conflicts of interest and source of funding
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. There are no relevant disclosures. We have no conflicts of interest. The Manuscript submitted does not contain information about medical device(s)/drug(s). All authors significantly contributed to the document and have reviewed the final manuscript.
Declaration of competing interest
None.
Acknowledgement
None.
References
- 1.Maradit Kremers H., Larson D.R., Crowson C.S., et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386–1397. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100(17):1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 3.Lefaivre K.A., Shadgan B., O'Brien P.J. 100 most cited articles in orthopaedic surgery. Clin Orthop Relat Res. 2011;469(5):1487–1497. doi: 10.1007/s11999-010-1604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banerjee S., Cherian J.J., Elmallah R.K., Pierce T.P., Jauregui J.J., Mont M.A. Robot-assisted total hip arthroplasty. Expet Rev Med Dev. 2016;13(1):47–56. doi: 10.1586/17434440.2016.1124018. [DOI] [PubMed] [Google Scholar]
- 5.Kayani B., Konan S., Tahmassebi J., Pietrzak J.R.T., Haddad F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint Lett J. 2018;100-B(7):930–937. doi: 10.1302/0301-620X.100B7.BJJ-2017-1449.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hampp E.L., Chughtai M., Scholl L.Y., et al. Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg. 2019;32(3):239–250. doi: 10.1055/s-0038-1641729. [DOI] [PubMed] [Google Scholar]
- 7.Bellemans J., Vandenneucker H., Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res. 2007;464:111–116. doi: 10.1097/BLO.0b013e318126c0c0. [DOI] [PubMed] [Google Scholar]
- 8.Boylan M., Suchman K., Vigdorchik J., Slover J., Bosco J. Technology-assisted hip and knee arthroplasties: an analysis of utilization trends. J Arthroplasty. 2018;33(4):1019–1023. doi: 10.1016/j.arth.2017.11.033. [DOI] [PubMed] [Google Scholar]
- 9.Jacofsky D.J., Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31(10):2353–2363. doi: 10.1016/j.arth.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 10.Chen X., Deng S., Sun M.L., He R. Robotic arm-assisted arthroplasty: the latest developments. Chin J Traumatol. 2022;25(3):125–131. doi: 10.1016/j.cjtee.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liow M.H.L., Goh G.S., Wong M.K., Chin P.L., Tay D.K., Yeo S.J. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2942–2951. doi: 10.1007/s00167-016-4076-3. [DOI] [PubMed] [Google Scholar]
- 12.Chen X., Xiong J., Wang P., et al. Robotic-assisted compared with conventional total hip arthroplasty: systematic review and meta-analysis. Postgrad Med. 2018;94(1112):335–341. doi: 10.1136/postgradmedj-2017-135352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mancino F., Cacciola G., Malahias M.A., et al. What are the benefits of robotic-assisted total knee arthroplasty over conventional manual total knee arthroplasty? A systematic review of comparative studies. Orthop Rev (Pavia). 2020;12(Suppl 1):8657. doi: 10.4081/or.2020.8657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lim S.J., Ko K.R., Park C.W., Moon Y.W., Park Y.S. Robot-assisted primary cementless total hip arthroplasty with a short femoral stem: a prospective randomized short-term outcome study. Comput Aided Surg. 2015;20(1):41–46. doi: 10.3109/10929088.2015.1076044. [DOI] [PubMed] [Google Scholar]
- 15.Domb B.G., El Bitar Y.F., Sadik A.Y., Stake C.E., Botser I.B. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472(1):329–336. doi: 10.1007/s11999-013-3253-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Domb B.G., Redmond J.M., Louis S.S., et al. Accuracy of component positioning in 1980 total hip arthroplasties: a comparative analysis by surgical technique and mode of guidance. J Arthroplasty. 2015;30(12):2208–2218. doi: 10.1016/j.arth.2015.06.059. [DOI] [PubMed] [Google Scholar]
- 17.Song E.K., Seon J.K., Yim J.H., Netravali N.A., Bargar W.L. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471(1):118–126. doi: 10.1007/s11999-012-2407-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siebert W., Mai S., Kober R., Heeckt P.F. Technique and first clinical results of robot-assisted total knee replacement. Knee. 2002;9(3):173–180. doi: 10.1016/s0968-0160(02)00015-7. [DOI] [PubMed] [Google Scholar]
- 19.Cool C.L., Needham K.A., Khlopas A., Mont M.A. Revision analysis of robotic arm-assisted and manual unicompartmental knee arthroplasty. J Arthroplasty. 2019;34(5):926–931. doi: 10.1016/j.arth.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 20.Maldonado D.R., Go C.C., Kyin C., et al. Robotic arm-assisted total hip arthroplasty is more cost-effective than manual total hip arthroplasty: a markov model analysis. J Am Acad Orthop Surg. 2021;29(4):e168–e177. doi: 10.5435/JAAOS-D-20-00498. [DOI] [PubMed] [Google Scholar]
- 21.Pierce J., Needham K., Adams C., Coppolecchia A., Lavernia C. Robotic arm-assisted knee surgery: an economic analysis. Am J Manag Care. 2020;26(7):e205–e210. doi: 10.37765/ajmc.2020.43763. [DOI] [PubMed] [Google Scholar]
- 22.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 23.Kurtz S.M., Lau E., Ong K., Zhao K., Kelly M., Bozic K.J. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaramaz B., DiGioia A.M., 3rd, Blackwell M., Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop Relat Res. 1998;(354):70–81. doi: 10.1097/00003086-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Cobb J., Henckel J., Gomes P., et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. 2006;88(2):188–197. doi: 10.1302/0301-620X.88B2.17220. [DOI] [PubMed] [Google Scholar]
- 26.Zhang W., Tang N., Li X., George D.M., He G., Huang T. The top 100 most cited articles on total hip arthroplasty: a bibliometric analysis. J Orthop Surg Res. 2019;14(1):412. doi: 10.1186/s13018-019-1476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yakkanti R., Greif D.N., Wilhelm J., Allegra P.R., Yakkanti R., Hernandez V.H. Unicondylar knee arthroplasty: a bibliometric analysis of the 50 most commonly cited studies. Arthroplast Today. 2020;6(4):931–940. doi: 10.1016/j.artd.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.P I . Medical Market and Technology Reports. 2016. US and European markets for joint arthroplasty products.https://pharmastore.informa.com/wp-content/uploads/2016/09/2-U.S.-and-European-Markets-for-Joint-Arthroplasty-Products.pdf Published. [Google Scholar]
- 29.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020-2040 using the national inpatient sample. J Rheumatol. 2019;46(9):1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]