Abstract
Objectives
During orthodontic treatment, patients are often apprehensive about reduced food intake and loss of body weight. Body mass index (BMI) assessment is an inexpensive, easy method for screening and studying changes in weight categories. This research aimed to determine whether long-term changes in BMI, self-esteem, and food habits occur in patients during the first year of orthodontic treatment.
Methods
BMI was calculated for 120 patients undergoing orthodontic treatment. Data were collected at baseline, and after the end of the first, second, third, sixth, and twelfth months. Rosenberg's self-esteem scale was used for scoring self-esteem. The Food Habit Assessment Scale was used to study changes in eating habits. Statistical analysis was performed with repeated measures ANOVA followed by Tukey HSD post-hoc test for BMI scores and Kruskal–Wallis test followed by Dunn's multiple comparison post-hoc tests for the Rosenberg scale and food habits questionnaire.
Results
At the end of 12 months, 43.4% of patients had a decrease in BMI, 45.8% had a mild to moderate increase in BMI, and 10.8% of patients maintained their BMI levels. The changes were not statistically significant. Self-esteem changes were statistically significant for both genders. Changes in food habits were also significant.
Conclusion
BMI decreased for the first 3 months and gradually recovered by the end of the first year of treatment. Self-esteem scores showed a significant improvement in both genders. Patients reverted to pre-treatment food habits by the end of the year.
Keywords: Body mass index, Food habits, Orthodontic appliances-fixed, Orthodontics, Prospective study, Self-esteem
الملخص
أهداف البحث
أثناء علاج تقويم الأسنان، غالبا ما نواجه المرضى القلقين حول انخفاض تناول الطعام وفقدان وزن الجسم. مؤشر كتلة الجسم غير مكلف وطريقة سهلة التنفيذ لفحص ودراسة التغيرات في فئات الوزن. يهدف هذا البحث إلى معرفة ما إذا كانت هناك تغييرات طويلة الأجل في مؤشر كتلة الجسم، واحترام الذات، والعادات الغذائية للمرضى خلال السنة الأولى من علاج تقويم الأسنان.
طرق البحث
تم حساب مؤشر كتلة الجسم لعدد 120 مريضا يخضعون لعلاج تقويم الأسنان. تم جمع البيانات في بداية ونهاية شهر العلاج الأول والثاني والثالث والسادس والثاني عشر. تم استخدام مقياس روزنبرغ لتقدير الذات لتقييم مستوى احترام الذات. تم استخدام مقياس تقييم العادة الغذائية لدراسة التغيرات في عادات الأكل.
النتائج
في نهاية 12 شهرا، كان لدى 43.4٪ من المرضى انخفاض في مؤشر كتلة الجسم، و45.8٪ لديهم زيادة خفيفة إلى معتدلة في مؤشر كتلة الجسم، وحافظ 10.8٪ من المرضى على مستويات مؤشر كتلة الجسم لديهم. لم تكن التغييرات ذات دلالة إحصائية. كانت تغييرات احترام الذات ذات دلالة إحصائية لكلا الجنسين. التغييرات في العادات الغذائية كانت ذات دلالة إحصائية أيضا.
الاستنتاجات
انخفاض مؤشر كتلة الجسم كان في الأشهر الثلاثة الأولى وتعافى تدريجيا بنهاية السنة الأولى من العلاج. أظهرت درجات احترام الذات تحسنا كبيرا في كلا الجنسين. عاد المرضى إلى العادات الغذائية قبل العلاج بنهاية السنة.
الكلمات المفتاحية: مؤشر كتلة الجسم, العادات الغذائية, تقدير الذات, أجهزة تقويم الأسنان الثابتة, تقويم الأسنان, الدراسة المستقبلية
Introduction
Orthodontic treatment offers several benefits, such as improvement in facial esthetics; oral functional efficiency; and an overall enhancement of individuals’ self-esteem, self-confidence, and work performance.1 Beyond the discomfort caused by brackets, arch wires, and auxiliary springs, mild to moderate pain is also experienced after separators are placed and after every activation.2 Patients are instructed to avoid or reduce consumption of hard, sticky, and fibrous foods to avoid breakage of the appliance and prevent dental caries, and for ease of maintenance of better oral hygiene. As a result of these protocols, both parents and patients complain about food restrictions and are apprehensive about weight loss during orthodontic treatment, thus potentially affecting patient compliance. Clinicians and patients cite these negatives as major concerns.3
The body mass index (BMI) is an easy and inexpensive way to screen and study changes in weight categories that may result in health problems. The World Health Organization uses BMI as the standard for recording obesity statistics. In the early nineteenth century, Adolphe Quetelet, a Belgian astronomer and mathematician, developed the basis of the BMI. Ancel Keys coined the modern term “body mass index” in the 1970s.4 An estimated 39% of the global adult population was overweight or obese in 2014, representing a doubling since 1975.5 The concept that childhood and adolescent BMI changes may predict adult obesity as well as adult fat mass and distribution is interesting, given that BMI can easily be calculated from standardized growth charts, which include height and weight. Studies have reported that both BMI and obesity track from childhood to adulthood; the closer to adulthood, the stronger the tracking.6,7 BMI for children and teenagers is age and sex specific and is often referred to as BMI-for-age. It is also associated with individual well-being on both a physical and emotional level.8
Studies on BMI changes during orthodontic treatment have been conducted for only short periods (1–3 months).9, 10, 11 Very few data have indicated long-term follow up of BMI levels. Therefore, this cohort study was conducted to scientifically validate the changes in BMI and to clarify patients’ qualms about weight loss. The aim of this study was to determine whether long-term changes occur in the BMI, self-esteem, and food habits of the patients during the first year of orthodontic treatment.
Materials and Methods
The study was approved by our Institutional Ethics Committee (ref. No. 0425/DE/2010). To determine the power and size of the sample, we used G-power software (Heinrich-Heine-University, Dusseldorf, North Rhine-Westphalia, Germany). On the basis of the inputs, error probability = 0.05, effect size f = 0.50, power (1-∗ err prob) = 0.95, and number of groups = 6, we determined that the required sample size was 90 with a power of 0.96. A convenience sampling method was applied to determine the required sample size.
Inclusion criteria
Patients 16–25 years of age who planned to undergo orthodontic treatment to correct malocclusion were included.
Exclusion criteria
Patients with a history of previous orthodontic treatment; patients with any systemic disease, physical disability, or stress; patients taking any long term medications for obesity, such as sibutramine, orlistat, or metformin; patients receiving steroid therapy; athletes, patients enrolled in a gym or following a diet for weight reduction; and patients who acquired a systemic disease during orthodontic treatment were excluded.
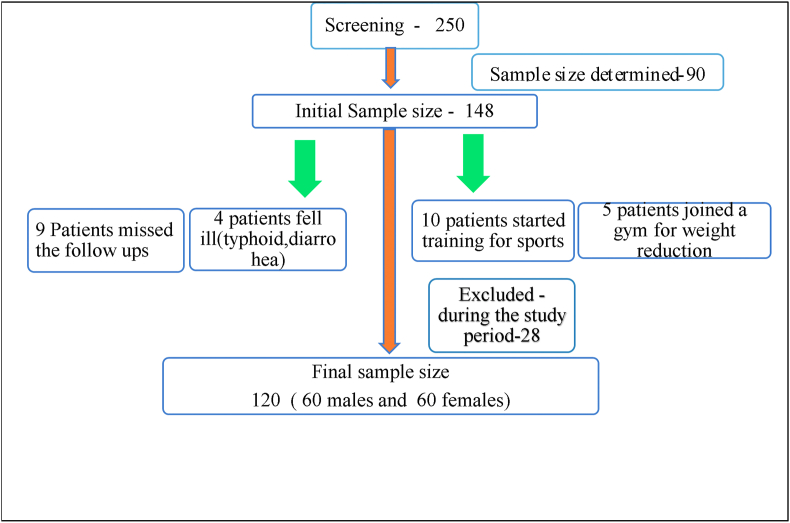
A total of 250 patients 16–25 years of age with planned fixed orthodontic treatment at the Department of Orthodontics, Government Dental College and Hospital, South India, were screened (Figure 1). Initially, 148 patients were enrolled in the study. At the end of 2 months, ten patients had joined sports activities, and five had joined a gym for weight loss. At the end of 5 months, nine patients had missed their follow-ups because of exams or vacations, and four patients had become ill. Those patients were excluded from the study. The final sample size was 120, with 60 males and 60 females (Table 1). Informed consent was obtained from all patients.
Figure 1.
Sampling flowchart.
Table 1.
Demographics of the participants.
| Overall age distribution | 16–25 years |
| Males (mean age) | 16–19 years: 16.97, SD: 0.94 |
| 20–25 years: 22.25, SD: 1.88 | |
| Females (mean age) | 16–19 years: 17.07, SD: 0.96 |
| 20–25 years: 23.1 SD: 1.64 | |
| Gender distribution | Males: 60; females: 60 |
| Work status | 68: undergraduate/school students |
| 40: postgraduate students | |
| 12: employed | |
| Socio-economic status | Middle and lower middle class |
| Malocclusion | Dental class I, class II, class III |
Data collection
BMI
The data collected were height in centimeters to the nearest 0.5 cm, measured with an audiometer (Seca 217, CA 91710, Chino, USA), and weight in kilograms to the nearest 0.5 kg, measured with a weighing machine (Seca 813, CA 91710, Chino, USA). We used the standard equation given by the US Centers for Disease Control and Prevention (CDC.gov) to calculate BMI (weight in kilograms/square of height in meters). The interpretation of BMI for adults and teens was performed according to the growth charts given by the CDC12 (Table 2).
Table 2.
Interpretation of BMI for different age groups.
| Interpretation of BMI for ages 20 and above | Interpretation of BMI for ages 2–19 |
|---|---|
| <18.5: underweight | <5th percentile: underweight |
| 18.5–24.9: normal or healthy weight | 5th percentile to 85th percentile: healthy weight |
| 25.0–29.9: overweight | 85th to <95th percentile: overweight |
| >30.0: obese | ≥95th percentile: obese |
Based on growth charts from the Centers for Disease Control and Prevention (CDC.gov).
Self-esteem
Self-esteem was scored with the Rosenberg Scale.13 This scale consists of five positive and five negative items. The score ranges from 0 to 30. Scores between 15 and 25 suggest a normal range. Scores below 15 indicate low self–esteem.
Food habits
Changes in food habits were studied with a modified food habits assessment (FHA) questionnaire.14 This closed-ended questionnaire consists of 15 items evaluating eating difficulties. Our decision to use a closed-ended model was based on having a well-defined variable or a construct and the ease of converting the results into numbers for analysis in a spreadsheet. From 0 to 30, the scoring was yes = 2 and no = 1. Higher values denoted more difficulties in eating.
Data were collected at the beginning of the treatment (pre-treatment), and at the end of the 1st, 2nd, 3rd, 6th, and 12th months, denoted T0, T1, T2, T3, T4, and T5, respectively.
Primary outcome measure
The primary outcome was the BMI score, calculated from the height and weight of the patients measured at various intervals (T0 to T5).
Secondary outcome measure
The secondary outcomes were the self-esteem scores and FHA questionnaire scores measured with the Rosenberg scale and the FHA questionnaire from T0 to T5.
Bias
To avoid selection bias, we included only orthodontic patients. The use of standard measurement instruments, World Health Organization classification of BMI, Rosenberg scale, and a validated questionnaire minimized information bias (misclassification bias). The scores and calculations were rechecked at random by two blinded clinicians to eliminate measurement bias.
In this study, a confounding factor was the height of the patients. Changes in height can occur due to growth in patients 16–19 years of age, thus influencing the BMI values. To reduce the confounding factor, patients 20–25 years of age who were in the post growth period with relatively stable height were also included.
Statistical analysis
Data were entered in Excel sheets for statistical analysis in SPSS software (version 22, IBM corporation). The BMI values were assessed for normality with the Shapiro–Wilk test and Levine's test for homogeneity of variance. Repeated measures ANOVA followed by Tukey's HSD post-hoc test was used to assess the significant differences at the indicated time intervals (T0, T1, T2, T3, T4, and T5). The Rosenberg scale and FHA questionnaire scores for female and male participants during the different treatment intervals did not pass normality tests, and the test for significance (P = 0.05) was performed with the Kruskal–Wallis test and Dunn's multiple comparisons post-hoc test.
Results
BMI
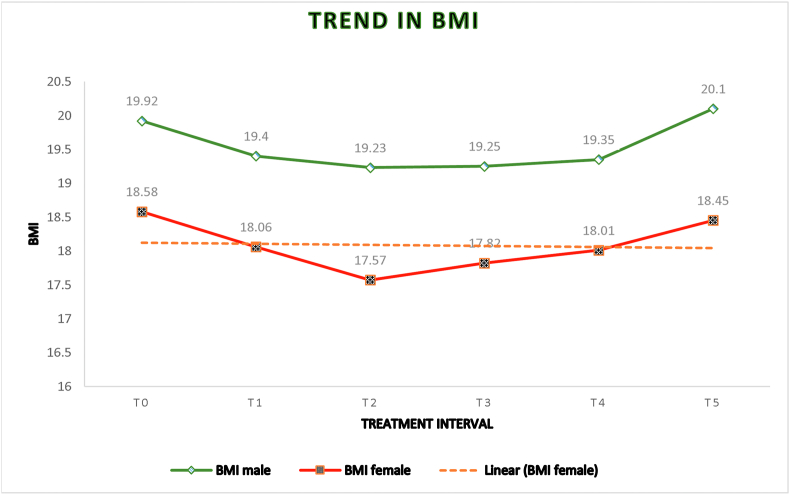
Of 120 patients, 50% had normal BMI, 44.2% were underweight, 5.8% were overweight, and none were obese at the pre-treatment level. At the end of the study period, 55% of patients had normal BMI, 40% were underweight, 5% were overweight, and none were obese (Table 3). A total of 51.3% of females and 35.5% of males had a decrease in their BMI with respect to pre-treatment levels. A total of 41.3% of females and 50.3% of males showed increases in their BMI levels. A total of 7.4% of females and 14.2% of males did not show changes in their BMI levels. Overall, 43.4% of patients had a decrease in BMI, 45.8% had a mild to moderate increase in BMI, and 10.8% maintained their BMI at the end of 12 months of orthodontic treatment. The BMI showed a biphasic tendency in both genders (Table 4). The BMI began to decrease immediately after T0 and continued to decrease up to 3 months (T1 and T2). Thereafter, the mean BMI began to increase slowly (T3, T4, and T5). The decrease in BMI was statistically significant during T1, T2, T3, and T4 with respect to baseline T0 in females, and during T1, T2, and T3 with respect to baseline T0 in males. In both genders, the values at the end of T5 (18.48 for females and 20.13 for males) did not statistically differ from those at T0 (18.58 for females and 19.92 for males) (Table 5). The height ranged from a minimum of 1.44 m to a maximum of 1.64 m. The change in height averaged of 2–4 cm. The changes in BMI scores for males (p = 0.96) and females (p = 0.77) between T0 and T5 were not significant.
Table 3.
Distribution of BMI categories according to age (in years).
| Age group | BMI category | Males (N = 44) |
Females (N = 50) |
||
|---|---|---|---|---|---|
| T0 | T5 | T0 | T5 | ||
| 16–19 years | Underweight | 19 | 18 | 28 | 27 |
| Normal | 22 | 23 | 21 | 22 | |
| Overweight | 3 | 3 | 1 | 1 | |
| Obese | 0 | 0 | 0 | 0 | |
| Age group | BMI category | Males (N = 16) |
Females (N = 10) |
||
|---|---|---|---|---|---|
| T0 | T5 | T0 | T5 | ||
| 20–25 years | Underweight | 4 | 2 | 2 | 1 |
| Normal | 11 | 13 | 6 | 8 | |
| Overweight | 1 | 1 | 2 | 1 | |
| Obese | 0 | 0 | 0 | 0 | |
N = number of patients. Distribution of patients under different categories of BMI according to different age groups. T0: beginning of treatment; T5: end of the study.
Table 4.
Average values of BMI, Rosenberg scale (RBS), and food habits questionnaire (FHA) for males and females at different levels. N = 60 M/60 F.
| Levels | BMI Female | BMI Male | RBS Female | RBS Male | FHA Female |
FHA Male |
|
|---|---|---|---|---|---|---|---|
| T0 | Mean | 18.58 | 19.92 | 14.83 | 15.53 | 20.33 | 20.33 |
| std. deviation | 2.67 | 3.22 | 1.76 | 2.08 | 2.4 | 2.45 | |
| T1 | Mean | 18.06 | 19.42 | 15.1 | 16.03 | 17.56 | 17.83 |
| std. deviation | 2.76 | 3.24 | 1.84 | 1.77 | 2.31 | 1.83 | |
| T2 | Mean | 17.57 | 19.23 | 15.1 | 16.06 | 17.6 | 17.26 |
| std. deviation | 2.78 | 3.12 | 1.84 | 1.65 | 2.08 | 2.19 | |
| T3 | Mean | 17.82 | 19.39 | 15.63 | 16.56 | 17.7 | 15.33 |
| std. deviation | 2.87 | 3.35 | 1.62 | 1.61 | 2.13 | 1.47 | |
| T4 | Mean | 18.09 | 19.55 | 18.7 | 17.23 | 17.06 | 13.73 |
| std. deviation | 2.73 | 3.24 | 2.4 | 1.47 | 2.27 | 1.56 | |
| T5 | Mean | 18.48 | 20.13 | 20.23 | 17.6 | 16.5 | 13.7 |
| std. deviation | 2.69 | 3.08 | 2.47 | 1.58 | 2.09 | 1.51 | |
T0, T1, T2, T3, T4, and T5 indicate the start, and the end of the first, second, third, sixth, and twelfth months, respectively. BMI gradually decreased in females from T0 to T4 and increased from T4 to T5. BMI in males did not differ drastically from T0 and returned to the initial values at the end of study period. The average self-esteem score was normal in males and moved to a higher level, whereas females had lower self-esteem initially but showed a marked improvement at the end of the study period. FHA scores showed a gradual improvement for females and a significant improvement for males from T3.
Table 5.
Comparison of statistical significance of BMI, RBS, and FHA at various treatment levels.
| Levels | Levels | BMI Female | BMI Male | RBS Female | RBS Male | FHA Female | FHA Male |
|---|---|---|---|---|---|---|---|
| T0 | T1 | P∗ | P∗∗ | NS | NS | P∗∗∗ | P∗∗∗ |
| T2 | P∗∗∗ | P∗∗∗ | NS | NS | NS | P∗ | |
| T3 | P∗∗∗ | P∗∗∗ | NS | NS | NS | NS | |
| T4 | P∗ | NS | P∗∗∗ | P∗∗∗ | NS | NS | |
| T5 | NS | NS | P∗∗∗ | P∗∗∗ | NS | NS | |
| T1 | |||||||
| T2 | P∗ | NS | NS | NS | NS | NS | |
| T3 | NS | NS | NS | NS | NS | NS | |
| T4 | NS | NS | P∗∗∗ | P∗ | NS | P∗∗ | |
| T5 | NS | NS | P∗∗∗ | P∗∗ | P∗∗∗ | P∗∗∗ | |
| T2 | |||||||
| T3 | NS | NS | NS | NS | NS | NS | |
| T4 | NS | NS | P∗∗∗ | P∗ | NS | P∗∗∗ | |
| T5 | NS | NS | P∗∗∗ | P∗∗ | P∗∗∗ | P∗∗∗ | |
| T3 | |||||||
| T4 | NS | NS | P∗∗ | NS | NS | P∗∗∗ | |
| T5 | NS | NS | P∗∗∗ | NS | P∗∗∗ | P∗∗∗ | |
| T4 | |||||||
| T5 | NS | NS | NS | NS | NS | P∗ |
P∗: significant; P∗∗: highly significant; P∗∗∗: extremely significant; NS: not significant. BMI scores showed no significant changes between T0 and T5 in both genders. The Rosenberg scale showed significant changes between T0 and T5 in females and males. FHA scores showed significant changes from T0 to T1, and T1 to T5 in males and females. BMI and FHA scores showed no significant changes between T0 (at the beginning of the treatment) and T5 (at the end of 12 months).
Self-steem
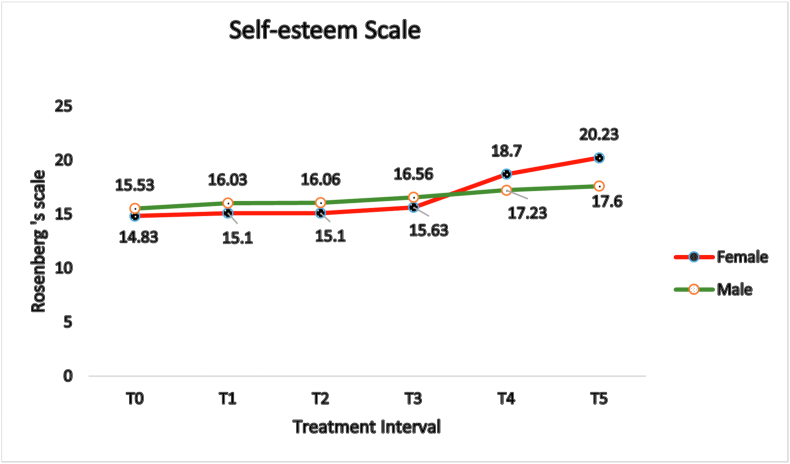
The mean Rosenberg scores (RBSs) during T4 and T5 (18.7 and 20.2) in females showed significant differences with respect to T0, T1, T2, and T3 (14.8, 15.1, 15.1, and 15.6) (Table 4). The scores rapidly increased from T3 (15.6) to T4 (18.7). However, in males, the mean steadily increased from T0 to T5 (15.5, 16.0, 16.0, 16.5, 17.2, and 17.6). In both genders, the mean RBS began to increase immediately after T0 and continued to T5. A significant difference in RBS values was observed among different treatment intervals in males as well as in females (p < 0.0001) (Table 5).
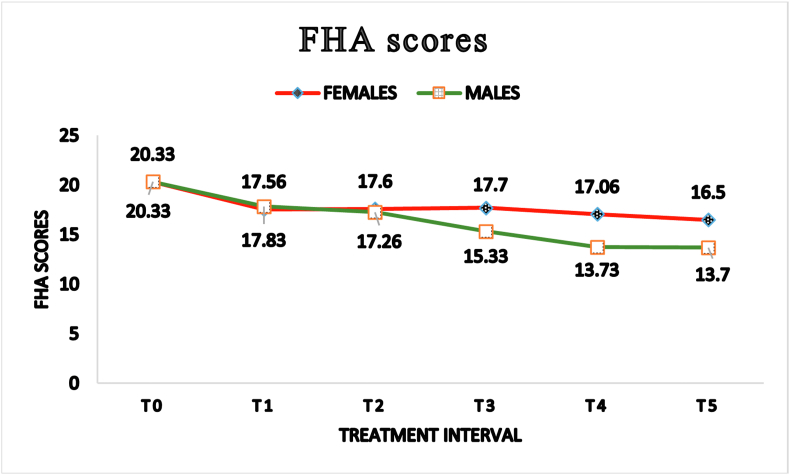
FHA
The mean FHA values were 20.33 at T0 and 16.5 at T5 in females, and were 20.33 at T0 and 13.7 at T5 in males (Table 4). In females, the changes in the mean FHA values were significant from T0 to T5 but were not significant at other levels (T1, T2, T3, and T4) with respect to T0. Males showed no significant changes from T0 to T1, T2, and T3, but showed significant changes from T0 to T4 and T5 (Table 5).
Discussion
BMI
Placement of separators, placement of initial arch wires, adjustments, and activation of orthodontic appliances can cause discomfort and pain for 2–3 days, which decreases by the fifth or sixth day.15 This pain affects patients’ eating patterns. Patients may avoid hard foods and restrict food intake because of the conditioned and nociceptive reflexes elicited by arch wire activation.16 Michelotti et al., in an electromyography study with separators, have found a decrease in motor output and pressure pain threshold in the mastication muscles.17 This finding may be considered a protective mechanism against further damage to the masticatory system. Similarly, Krishnan has concluded that the placement and activation of arch wires cause pain and may affect dietary habits and daily life activities.2 Interference with arch wires may result in reduced intake of food and a loss of pleasure in eating. In general, the changes in dietary patterns might result in an increase or decrease in weight.
Body mass index is often used as a screening instrument for weight-related disorders such as obesity. Several factors influence BMI values, including age, gender, ethnicity, socio-economic status, physical activity, and diet. The rising trend in BMI may indicate unfavorable societal and environmental conditions that promote inactivity, excessive energy intake, and malnutrition.18 Lilja et al. have demonstrated greater BMI gain in young adulthood,19 and Whitlock et al. have noted a linear relationship of BMI with age.20 Being underweight is also associated with health problems, similarly to being overweight or obese. In children and adolescents, being underweight increases the risk of several infections, particularly in developing countries.21
In the present study, we recorded and analyzed the BMI of participants from T0 to T5 over 12 months during orthodontic treatment. Jan et al. have studied the changes in BMI for 2 months and concluded that orthodontic treatment causes weight loss, and the treatment can be used to prevent obesity and improve personality.9 Ajwa et al. have arrived at a similar conclusion regarding a change in BMI between the first and second treatment visits.10 Additionally, they have claimed that their results can be used as guidance for structured diet planning. Drawing such emphatic conclusions seems premature without observing sequential changes in BMI. Our observations were similar to those in a study by Sandeep et al.,11 whose period of observation was 3 months. Our study involved a longer observation period of 12 months to gain a better understanding of BMI changes over the course of the treatment. Our results during the first 2 months were similar to those in the above studies, but the change In the trend was evident in the following months. Patients require time for adaptation after being introduced to the new challenge of combating discomfort and pain. As observed in our study, this adaptation occurs only from the third month onward. The patients showed a positive trend in weight gain, reverting to their pre-treatment BMI scores. The overall mean revealed that males had a higher BMI (19.9) than females (18.58) (Table 4). BMI changes in males were minimal, and no significant changes were observed from T0 to T4 and T5, similarly to the findings in Sandeep et al.11 Several patients even showed increases in BMI scores (Table 5). Because BMI does not distinguish between fat and muscle, the higher BMI scores and minimal changes in males were attributable to the development of greater muscle mass than that in females during the developmental ages or could also have been due to males reverting to old food habits more quickly than females, as observed in this study. In contrast, the changes in BMI were relatively greater in females, similarly to findings from a study by Yi et al.22 Females showed a sharp dip in the graph, whereas males showed gradual changes. However, both values returned closer to their initial values at the end of the study period (Figure 2). We observed that patients might show increases in their BMI values but still fall under the same BMI category (underweight or normal). The current study revealed that the BMI changes are temporary, as affirmed by the patients. Because orthodontic treatment generally occurs over long periods, conclusions based on observations over a short period might be deceptive. Dietary changes based on a short observation period might not be advisable. Hence, considering fixed orthodontic appliances for weight reduction regimens is questionable and should be advised with caution, particularly in males.
Figure 2.
BMI trend in females and males.
Self-esteem
Malocclusion is known to affect self-respect and self-esteem, and thus overall quality of life. Similarly to the observations of Jung et al., our findings indicated a marked improvement in the patients’ self-esteem.23 The changes were greater in females than in males. The average self-esteem score in males was 15.3 at T0 and gradually increased to 20.2 at T5, whereas females initially had lower self-esteem but showed marked improvements in self-esteem at the end of the study period (14.8–20.23) (Figure 3). Interestingly, females considered their facial esthetics more important to their self-esteem than males of the same age. This finding may be related to a higher number of female patients opting for orthodontic treatments than males, similarly to the results of a study by Lagorsse et al.24
Figure 3.
Rosenberg's self-esteem scale.
FHA questionnaire
Our food habit questionnaire revealed that patients experienced difficulty only in the initial months, and by the end of the third month, they were able to return to their regular eating habits. Similarly to studies Jawad et al. and Soni et al., our study indicated that patients’ eating habits improved significantly with time, as they learned how to manage their fixed appliances, and developed the skills to bite and chew firmer and harder food items with their appliance.14,25 They reverted to their old eating habits, similarly to findings in studies by Azaripour et al. and Negrutiu et al.26,27 Consequently, the patients regained lost weight from the third month of treatment. Feldmann et al. have concluded that masticatory ability decreases during the first 24 h after the insertion of a fixed appliance and returns to baseline after 4–6 weeks.28 We concur with those results and ascribe the improvement in our patients' eating habits to this effect (Figure 4). Many of our patients reported eating fewer snacks and eating healthier foods, similarly to the findings of a study by Sandeep et al.11 Improvements in self-esteem were also attributable to patients eating healthier food.
Figure 4.
Food Habit Questionnaire scores.
Limitations of the study
Non-availability of obese patients: We attribute the lack of obese patients partly to the geographic location of the government hospital and to the socio-economic conditions (lower middle class) of the outpatients visiting the hospital. The inclusion of patients from all BMI categories would have strengthened the study.
Duration of the study period: The duration of orthodontic treatment differs among patients. In our study, we could not continue with a longer follow-up because of the differences in treatment duration, dropout, and missed follow-ups, thus leading to a decreased sample size at the end of the year.
Prospects of the study:
-
1.
Studies involving BMI analysis for the entire treatment period would limit conflicting opinions on this subject.
-
2.
Studies with similar types of treatment plans would provide better insight into the difficulty level for eating and oral hygiene maintenance.
Conclusion
-
•
BMI decreased in the first 3 months and gradually recovered by the end of the first year of treatment. Hence, changes in BMI during orthodontic treatment can be considered temporary and to have no significant overall impact at the end of 1 year.
-
•
The self-esteem of the patients significantly improved during the course of orthodontic treatment.
-
•
Changes in diet patterns were observable only during the first few months of orthodontic treatment, after which the patients resumed their regular eating habits. Hence, considering fixed orthodontic appliances for a weight loss regimen is questionable and should be advised with caution, particularly in males.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This was a self-funded study.
Conflict of interest
Both authors (VG and SG) certify that they have no affiliations with, or involvement in, any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed herein. All authors declare no conflicts of interest.
Ethical approval
Institutional Ethical Committee, Government. Dental College and Hospital, TN Dr. MGR Medical University, Tamilnadu, India approved this study (ref. No. 0425/DE/2010) on 24 April 2013.
Authors contributions
VG conceived and designed the study; supervised the data collection; analyzed and interpreted data; wrote the initial and final drafts of the article; and gave final approval of the draft. SG designed and conducted research; provided research materials; collected, organized, analyzed, and interpreted data; wrote the initial and final drafts of the article; and gave final approval of the draft. All authors agree to be accountable for all aspects of the work in ensuring that questions associated with the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Vaneesa de Couto N., Ana Claudia de Castro F.C., Mauricio de Alemeida C., Danilo Pinelli V., Renata Rodrigues de A.P. Impact of orthodontic treatment on self-esteem and quality of life of adult patients requiring oral rehabilitation. Angle Orthod. 2016;86(5):839–845. doi: 10.2319/072215-496.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krishnan V. Orthodontic pain from causes to management—a review. Eur J Orthod. 2007;29(2):170–179. doi: 10.1093/ejo/cjl081. [DOI] [PubMed] [Google Scholar]
- 3.Keim R.G. Managing orthodontic pain. J Clin Orthod. 2004 Dec;38(12):641–642. [PubMed] [Google Scholar]
- 4.Eknoyan G. Adolphe Quetelet (1796-1874)—the average man and indices of obesity. Nephrol Dial Transplant. 2008 Jan;23(1):47–51. doi: 10.1093/ndt/gfm517. Epub 2007 Sep 22. PMID: 17890752. [DOI] [PubMed] [Google Scholar]
- 5.Di Cesare M., Bentham J., Stevens G.A., Zhou B., Danaei G., Lu Y., et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016 Apr 2;387(10026):1377–1396. doi: 10.1016/S0140-6736(16)30054-x. PMID: 27115820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell P.T., Katzmarzyk P.T., Malina R.M., Rao D.C., Perusse L., Bouchard C. Stability of adiposity phenotypes from childhood and adolescence into young adulthood with contribution of parental measures. Obes Res. 2001 Jul 9;(7):394–400. doi: 10.1038/oby.2001.51. [DOI] [PubMed] [Google Scholar]
- 7.Freedman D.S., Khan L.K., Serdula M.K., Dietz W.H., Srinivasan S.R., Berenson G.S. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005 Jan;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 8.Nuttall F.Q. Body mass index: obesity, BMI and health: a critical review. Nutr Today. May/June 2015;50(3):117–128. doi: 10.1097/NT.0000000000000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jan H., Bashir U., Naureen S., Anwar A. Personality improvement through orthodontics. Pak Oral Dental J. 2009 Dec;29(2):275–278. [Google Scholar]
- 10.Ajwa N., Makhdoum L., Alkhateeb H., Alkhumayes H. The impact of orthodontic appliance on body weight changes, dietary habits, and self-perceived discomfort in early stages of orthodontic treatment. Global J Health Sci. 2018 Aug;10(9):11–17. [Google Scholar]
- 11.Sai Sandeep K., Singaraju G.S., Reddy K.V., Mandava P., Bhavikati V.N., Reddy R. Evaluation of body weight, body mass index, and body fat percentage changes in early stages of fixed orthodontic therapy. J Int Soc Prev Community Dent. 2016 Jul-Aug;6(4):349–358. doi: 10.4103/2231-0762.186796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age.
- 13.Rosenberg M. Revised edition. Wesleyan University Press; Middletown, CT: 1989. Society and the adolescent self-image. [Google Scholar]
- 14.Abed Al Jawad F., Cunningham S.J., Croft N., Johal A. A qualitative study of the early effects of fixed orthodontic treatment on dietary intake and behaviour in adolescent patients. Eur J Orthod. 2012 Aug;34(4):432–436. doi: 10.1093/ejo/cjr032. [DOI] [PubMed] [Google Scholar]
- 15.Bondemark L., Fredrikkson K., Ilros S. Separation effect and perception of pain and discomfort from two types of orthodontic separators. World J Orthod. 2004 Summer;5(2):172–176. PMID: 15615136. [PubMed] [Google Scholar]
- 16.Erdinc A.M.E., Dincer B. Any arch wire: perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004 Feb;26(1):79–85. doi: 10.1093/ejo/26.1.79. [DOI] [PubMed] [Google Scholar]
- 17.Michelotti A., Farella M., Martina R. Sensory and motor changes of the human jaw muscles during induced orthodontic pain. Eur J Orthod. 1999 Aug;21(4):397–404. doi: 10.1093/ejo/21.4.397. [DOI] [PubMed] [Google Scholar]
- 18.Reas D.L., Nygård J.F., Svensson E., Sørensen T., Sandanger l. Changes in body mass index by age, gender, and socio-economic status among a cohort of Norwegian men and women (1990–2001) BMC Public Health. 2007 Sep 30;7:269. doi: 10.1186/1471-2458-7-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lilja M., Eliasson M., Stegmayr B., Olsson T., Soderberg S. Trends in obesity and its distribution: data from the northern Sweden MONICA survey, 1986–2004. Obesity (Silver Spring) 2008 May;16(5):1120–1128. doi: 10.1038/oby.2008.230. [DOI] [PubMed] [Google Scholar]
- 20.Whitlock G., Lewington S., Sherliker P., Clarke R., Emberson J., Halsey J., et al. Body-mass index and cause-specific mortality in 900000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009 Mar 28;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. Epub 2009 Mar 18. PMID: 19299006; PMCID: PMC2662372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dobner J., Kaser S. Body mass index and the risk of infection - from underweight to obesity. Clin Microbiol Infect. 2018 Jan;24(1):24–28. doi: 10.1016/j.cmi.2017.02.013. Epub 2017 Feb 20. PMID: 28232162. [DOI] [PubMed] [Google Scholar]
- 22.Yi S.W., Ohrr H., Shin S.A., Yi J.J. Sex-age-specific association of body mass index with all-cause mortality among 12.8 million Korean adults: a prospective cohort study. Int J Epidemiol. 2015 Oct;44(5):1696–1705. doi: 10.1093/ije/dyv138. PMID: 26208807; PMCID: PMC4681110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jung M.H. An evaluation of self-esteem and quality of life in orthodontic patients: effects of crowding and protrusion. Angle Orthod. 2015 Sep;85(5):812–819. doi: 10.2319/091814.1. Epub 2015 Mar 16. PMID: 25774755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lagorsse A., Gebeile-Chauty S. Does gender make a difference in orthodontics? A literature review. Orthod Fr. 2018 Jun;89(2):157–168. doi: 10.1051/orthodfr/2018011. Epub 2018 Jul 24. PMID: 30040615. [DOI] [PubMed] [Google Scholar]
- 25.Soni V.K., Sharma L., Patel P. Comparative evaluation of changes observed in the weights of patients undergoing fixed orthodontic treatment in Jaipur population. Int J Pharm Sci Invent. 2013;2(5):66–69. [Google Scholar]
- 26.Azaripour A., Willershausen I., Hassan M., Ebenezer S., Willershausen B. Oral hygiene and dietary habits in adolescents with fixed orthodontic appliances: a cross-sectional study. J Contemp Dent Pract. 2016 Mar 1;17(3):179–183. doi: 10.5005/jp-journals-10024-1824. PMID: 27207195. [DOI] [PubMed] [Google Scholar]
- 27.Negrutiu B.M., Todor B.I., Moca A., Vaida L.L., Judea-Pusta C. Dietary habits and weight loss in orthodontic patients. HVM Bioflux. 2019;11(2):57–60. [Google Scholar]
- 28.Feldmann I., List T., Bondemark L. Orthodontic anchoring techniques and its influence on pain, discomfort, and jaw function--a randomized controlled trial. Eur J Orthod. 2012 Feb;34(1):102–108. doi: 10.1093/ejo/cjq171. Epub 2011 Feb 7. PMID: 21300723. [DOI] [PubMed] [Google Scholar]