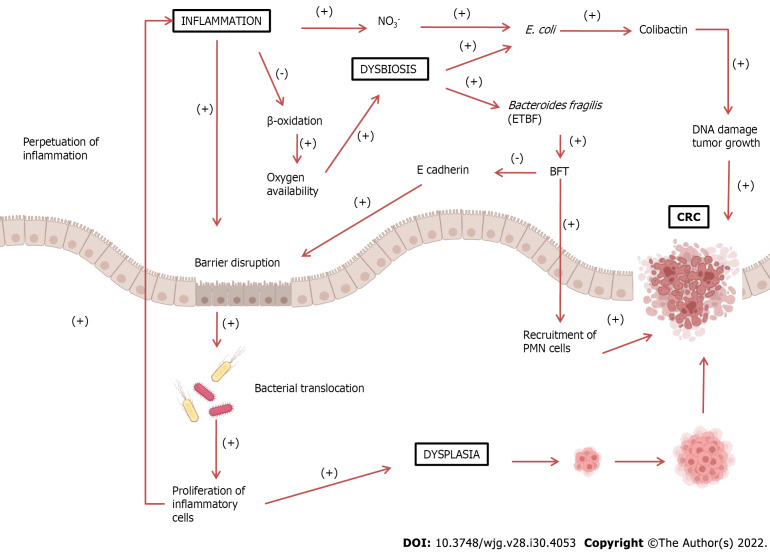
Figure 1.
Increased inflammatory response can lead to barrier disruption, allowing bacterial translocation into the intestinal lumen. These pathogens trigger an immune and inflammatory response, perpetuating the inflammatory process. Inflammatory cells can also cause dysplasia, leading to the development of colorectal cancer (CRC). Under normal conditions, epithelial cells, during β-oxidation, decrease oxygen availability, thus creating an anaerobic environment. During chronic inflammation, β-oxidation decreases, enhancing oxygen availability. This also leads to an increase in nitrate (NO3-) formation, leading to dysbiosis and growth of proteobacteria such as Escherichia coli (E. coli). E. coli produces colibactin, which could damage DNA and stimulate tumor growth. The growth of Bacteroidetes fragilis may also occur, which produces Bacteroides fragilis toxin (BFT). This toxin cleaves E-cadherin, a major constituent of the zonula adherens, which is responsible for cell adhesion, leading to further barrier disruption. Additionally, BFT also stimulates epithelial cells to recruit polymorphonuclear leukocytes (PMN) cells, promoting the development of CRC. BFT: Bacteroides fragilis toxin; ETBF: Enterotoxigenic Bacteroides fragilis; CRC: Colorectal cancer; PMN: Polymorphonuclear leukocytes.