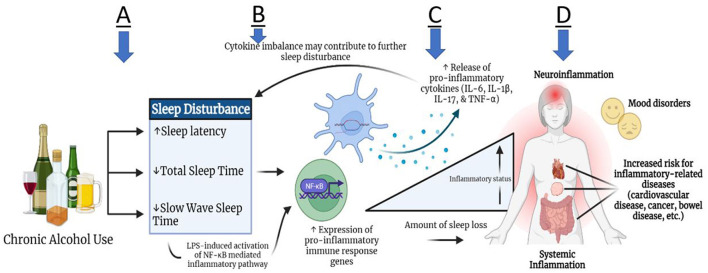
Figure 1.
Theoretical relationship between alcohol use and sleep disturbance with inflammation. Subsequent to chronic alcohol use, some individuals may experience increased sleep latency, as well as decreased total sleep time and slow wave sleep time (A). These sleep disturbances may contribute to heightened expression of pro-inflammatory immune response genes through the mechanism of toll-like receptor signaling, leading to leaked lipopolysaccharides (LPS) in plasma. LPS propagates the signal through different pathways, such as NF- κB, and induces cytokine production peripherally and in the brain (B). Pro-inflammatory cytokine production (IL-6, IL-1β, IL-17, TNF-α) can lead to systemic inflammation and neuro-inflammation (C,D). Due to the bidirectional link between the brain and periphery, the inflammatory activity can in turn lead to further altered sleep architecture. Ultimately, persistent inflammation can lead to an increased risk for inflammation-related comorbidities, such as cardiovascular disease, cancer, bowel diseases, and mood disorders (D).