INTRODUCTION
Stress and burnout among healthcare workers are at alarming levels.1 The Mini Z (Zero Burnout Program) worklife measure for clinicians was derived from validated instruments with the factor structure published in JGIM in 2016.2 The 1.0 version included 4 work conditions (work ambience (chaos), work control, teamwork effectiveness, and values alignment), 3 clinician reactions (stress, satisfaction, and burnout), and 3 items related to electronic medical record (EMR) stress (time pressure, home EMR time, and EMR proficiency). This paper investigates the psychometric structure of the 2.0 version which (1) changes EMR proficiency to EMR frustration, (2) aligns positive scores for calculation of a summary (joy) score, and (3) has two 5-item subscales (supportive work environment and work pace/EMR stress). Mini Zs have been adapted for residents, nurses, and administrators, and administered to thousands of healthcare workers in multiple languages across 5 continents. Concurrent validity of the burnout item was assessed with the Maslach Burnout Inventory (MBI) emotional exhaustion (EE) subscale.3 A subsequent study assessed convergent validity of the remaining items against EE and depersonalization MBI subscales.4 To provide a brief, valid measure for healthcare organizations to address clinician satisfaction and burnout, we determined the reliability and validity of the Mini Z 2.0’s two-subscale structure.
METHODS
A convenience sample of 7675 respondents (67% physicians, 59% female, and 72% white, in 80 organizations from 23 states) was assembled for the analysis from the American Medical Association burnout assessment program. Cronbach’s alpha and McDonald’s Omega coefficients assessed internal consistency (values > 0.7 acceptable to good for group-level measurement, as in PROMIS Measurement Standards, 2013). An inter-correlation matrix assessed item correlations. Confirmatory factor analysis models were constructed for the Mini Z 2.0 (5 items in each subscale), with confirmatory analysis examining significance of the loadings, as well as modification indices in a revised version with different subscale configurations based upon optimal factor scores and an overall unidimensional composite. For model fit, assessed using the comparative fit index (CFI), Tucker-Lewis index (TLI), standardized root mean residual (SRMR), and root mean square error of approximation (RMSEA), cut values5 indicating good fit included CFI and TLI > 0.95, SRMR < 0.05, and RMSEA < 0.08. Latent structural regression models assessed convergent validity of the new factors in relation to the PHQ2 depression index, and two items of self-rated home EMR use.
RESULTS
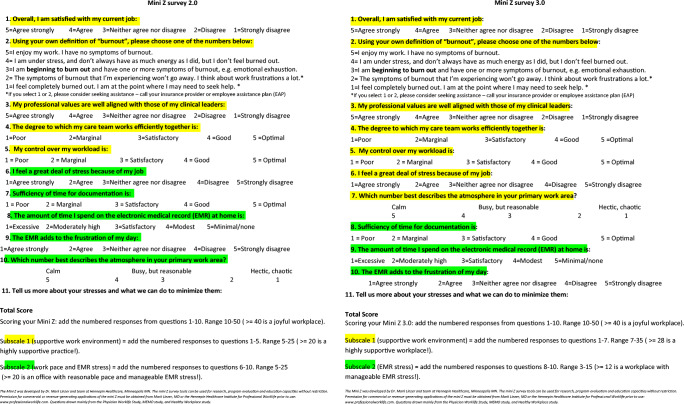
Table 1 demonstrates internal consistency and confirmatory factor analysis loadings for the two 5-item factor structure (alphas 0.75–0.83, omegas 0.82–0.86). In models 1 and 2, “supportive work environment” includes satisfaction, burnout, values alignment, teamwork, and work control, while “work pace/EMR stress” includes stress, chaos, home EMR, documentation time pressure, and EMR frustration; a bifactor analysis demonstrated good performance as either two domains or a 10 item measure. A subsequent confirmatory analysis (models 3 and 4) with a 7-item subscale (the original 5 items plus stress and chaos), and 3 EMR items (Fig. 1), had better fit indices (improved CFI, TLI, RMSR, and RMSEA) and reasonable performance of a bifactor model. A general factor model (model 5) showed good performance as a 10-item single domain. An inter-correlation matrix demonstrated good correlations (r > 0.3) between 80% of items (ps < 0.001). Convergent validity determinations (supplemental figures) confirmed a two-subscale structure, with better model fit for the 7- and 3-item structure versus the 5 and 5. The PHQ2 depression questions correlated with the supportive work environment factor, but not the EMR subscale.
Table 1.
Standardized Confirmatory Factor Analysis (CFA) Loadings for the MINI Z
| Original model | Revised model | ||||||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||
| Items | Factor 1 | Factor 2 | Bifactor | Factor 1 | Factor 2 | Bifactor | General factor |
| Satisfaction | 0.808 | 0.677 | 0.806 | 0.668 | 0.784 | ||
| Burnout | 0.848 | 0.826 | 0.831 | 0.826 | 0.810 | ||
| Values | 0.718 | 0.555 | 0.720 | 0.545 | 0.695 | ||
| Teamwork | 0.655 | 0.543 | 0.658 | 0.536 | 0.632 | ||
| Control | 0.716 | 0.722 | 0.717 | 0.724 | 0.689 | ||
| Stress | 0.822 | 0.815 | 0.772 | 0.806 | 0.751 | ||
| Chaos | 0.611 | 0.639 | 0.605 | 0.630 | 0.581 | ||
| EMR time pressure | 0.791 | 0.593 | 0.953 | 0.591 | 0.742 | ||
| Home EMR time | 0.684 | 0.434 | 0.758 | 0.430 | 0.647 | ||
| EMR frustration | 0.538 | 0.387 | 0.629 | 0.386 | 0.504 | ||
| Model fit | |||||||
| CFI | 0.863 | 0.982 | 0.954 | 0.982 | 0.841 | ||
| TLI | 0.819 | 0.968 | 0.939 | 0.967 | 0.795 | ||
| RMSEA | 0.190 | 0.080 | 0.110 | 0.081 | 0.202 | ||
| SRMR | 0.074 | 0.022 | 0.040 | 0.022 | 0.083 | ||
| Cronbach alpha | 0.83 | 0.75 | 0.85 | 0.85 | 0.78 | 0.85 | 0.85 |
| Omega | 0.86 | 0.82 | 0.86 | 0.90 | 0.83 | 0.86 | 0.90 |
| Reliability attrition | 3.5% | 8.5% | 5.5% | 6.0% | 5.5% | ||
Note: Only single domain estimates are provided for bifactor models (sub-domains are not reported). The following values indicate good model fit5: CFI and TLI > 0.95, SRMR < 0.05, and RMSEA < 0.08. The bifactor model indicates a single general factor with sub-domains; the general factor model indicates a single overall domain
CFI comparative fit index, TFI Tucker-Lewis index, SRMR standardized root mean residual, RMSEA root mean square error of approximation, EMR electronic medical record
Figure 1.
Mini Z items: original 2.0 factor structure (5 and 5-item subscales) vs new 3.0-factor structure (7 and 3 items)
DISCUSSION
In a 10-question instrument, the Mini Z provides information on satisfaction, burnout, and remediable work conditions. Due to the clinical utility of this parsimonious worklife measure,6 its use has expanded rapidly. In this analysis, we confirm a two domain structure, with a satisfactory unidimensional composite. Thus, organizations can portray an overall “joy score” and use the two original subscales which have good internal consistency. We have also determined that a different configuration of subscale items (now called the Mini Z 3.0) has better performance, with a 7-item subscale of work conditions and clinician reactions, and a 3-item EMR-related subscale. One limitation is that no independent measure of home EMR use was available; another is that the Mini Z 3.0 will need validation against the MBI.
Supplementary Information
(DOCX 3.26 mb)
Acknowledgements
This work was supported through the AMA.
Declarations
Conflict of Interest
Dr. Linzer reports support through Hennepin Healthcare for training wellness champions and burnout reduction studies from the AMA, ACP, IHI, Optum Office for Provider Advancement, and the ABIM Foundation. He is supported for burden of treatment and shared decision-making studies through NIH, co-leads a program in Learning Health Systems for AHRQ, and consults on a grant for Harvard University in diagnostic accuracy and work conditions. Ms. Poplau is supported by the AMA for this work through Hennepin Healthcare Research Institute. Dr. Goelz is supported through Hennepin Healthcare by IHI and the AMA, and Dr. Brown was paid for time on this project by the AMA. Dr. Sinsky is employed by the American Medical Association. The opinions expressed in this article are those of the authors and should not be interpreted as American Medical Association policy.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Prasad K, McLoughlin C, Stillman M, et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine. 2021;35:100879. doi: 10.1016/j.eclinm.2021.100879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linzer M, Poplau S, Babbott S, et al. Worklife and Wellness in Academic General Internal Medicine: Results from a National Survey. J Gen Intern Med. 2016;31:1004–1010. doi: 10.1007/s11606-016-3720-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20:75–79. doi: 10.1002/smi.1002. [DOI] [Google Scholar]
- 4.Olson K, Sinsky C, Rinne ST, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach Burnout Inventory. Stress Health. 2019;35:157–175. doi: 10.1002/smi.2849. [DOI] [PubMed] [Google Scholar]
- 5.Hu LT, Bentler PM. Cutoff criteria for fit indexes in Covariance Structure Analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 6.Lee JS, Karliner LS, Julian KA, Linzer M, Feldman MD. Change in faculty perceptions of burnout and work life in and academic general medicine clinic: a pre-post study. J Gen Intern Med. 2019;34(10):1973–1974. doi: 10.1007/s11606-019-05083-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 3.26 mb)