Abstract
Background:
In Canada, healthcare professionals often rely on ad hoc interpreters, who are untrained volunteers recruited via intercom hospital announcements to interpret for patients with language barriers. This study analyzed the frequency of ad hoc interpreter requests via intercom announcements to estimate hospital interpretation needs.
Methods:
A retrospective cohort analysis from intercom requests for medical interpretation collected from five hospitals of the McGill University Health Center. Requests included date, time, language requested, hospital location, and extension for who placed the request.
Results:
A total of 1265 intercom requests were placed for 48 languages, with the top five languages being Mandarin (17.8%), Punjabi (10.1%), Inuktitut (9.8%), Arabic (7.3%), and Cantonese (6.4%). Almost 69.8% of requests were made during working hours, 13.2% on workday evenings, and 14.8% on weekends. Requests came from urgent care (42.3%), outpatient (29.5%), and inpatient (23.3%) settings.
Conclusion:
This is the first published study that measures interpretation needs via intercom requests. We propose that our method can be replicated to inform implementation of professional medical interpretation services. We conclude that linguistic interpretation needs are significant in the Montreal area, and likely in Canada in general and pose a barrier to effective medical care.
Keywords: Medical interpretation, language barriers, access to healthcare
Introduction
The relationship between physicians and patients is reliant foremost on communication. Healthcare providers (HCPs) must understand patients’ medical history, symptoms, and emotional status to provide effective care. Language barriers thus pose serious obstacles to medical care and have been described as a patient safety issue in Canada.1,2 Language barriers negatively affect medication compliance and patient satisfaction, leading to increased costs for medical systems.3,4 Furthermore, language barriers reduce access to healthcare and place patients at higher risk of adverse outcomes.5,6 Assessing needs for linguistic interpretation in local contexts is important to develop and implement resources to benefit a given population, and ultimately healthcare institutions.
In many healthcare settings, HCPs request an interpreter either at the request of the patient or due to difficulty communicating. 1 In the absence of professional interpretation services, healthcare institutions often rely on ad hoc interpreters. 1 Ad hoc interpreters are found via requests, often from the hospital operator over the hospital intercom. Individuals who can speak the requested language, either hospital personnel or member of the public, then can volunteer by contacting the HCP. This type of recruitment is seen as beneficial in situations where interpretation is urgently needed. 1 Phone interpretation is available in some Canadian hospitals, but often requires pre-booking and is typically available during business hours only. For these reasons, it is not a well-utilized option in many Canadian hospitals. 7
Ad hoc interpreters are not an optimal solution to linguistic barriers faced in large healthcare institutions. Untrained interpreters may be unaware of the need for confidentiality, may not know medical terminology, and patients may be unwilling to share sensitive information with individuals who are not HCPs. 8 When compared to no interpretation, untrained interpretation leads to greater miscommunication, increased medical errors, and reduced quality of care. 9 – 11 However, given that HCPs rely on ad hoc interpreters in the absence of established services, requests represent a proxy to assess the prevalence of language barriers and needs for interpretation in hospitals. Indeed, requests for ad hoc interpreters are logged and available for analysis. Yet there is no published evidence on the frequency and nature of ad hoc interpretation requests in hospitals.
This study aimed to retrospectively analyze intercom announcement records for ad hoc interpretation at five hospitals of the McGill University Health Center (MUHC), a university healthcare network that offers tertiary care to a multicultural metropolitan population of Montreal, Canada. The objective was to assess the interpretation needs in a healthcare setting, in terms of languages requested and their frequency, hospital and specific hospital service, as well as time of day and week of requests.
New contribution
This study provides a novel method to utilize intercom requests as a measurement of language interpretation needs at a multi-site university hospital center. These methods and subsequent data collected can be used to identify unmet interpretation needs. We propose that our method of using intercom requests to measure the need for interpretation services can be replicated at other healthcare institutions and can be used to inform implementation of adapted professional interpretation services.
Methods
This was a retrospective review of all intercom requests for ad hoc interpreters at five MUHC hospitals (the Montreal General Hospital, the Royal Victoria Hospital, the Montreal Chest Institute, the Montreal Children’s Hospital, and the Lachine Hospital) placed between 1 January 2018 and 1 December 2020. Each site differed in its demographics and patients served. The Montreal General and the Royal Victoria Hospitals are comprehensive adult tertiary care centers with 479 and 517 beds, respectively. 12 The Lachine Hospital is a comprehensive community hospital with 134 beds. 13 The Montreal Children’s Hospital is a tertiary pediatrics hospital with 144 beds. 14 Each of the above hospitals have emergency rooms, as well as inpatient wards and outpatient clinics. The Montreal Chest Institute is a specialty outpatient respiratory medicine institute.
The intercom system allows for hospital-wide announcements. Anyone may submit a request for an announcement through a call-in system. The MUHC call center keeps the data concerning all requests and provided us with all verbatim requests concerning interpreter recruitment. We extracted data from raw intercom messages, including the date and time of the request, the language requested, the hospital the request came from, and when provided, the extension to which a volunteer could call to answer the request. No patient data were used in this analysis, and ethics exemption was granted by the MUHC Research Ethics Board (REB). Microsoft Excel (Microsoft Corporation, Redmond, WA) was used to manage all interpreter requests and data analysis.
Requests that did not include a specific language were excluded. Furthermore, repeat requests (requests placed sequentially in time with matching locations, languages, and call-back extension) were treated as double entries and removed from the analysis. Often, language requests were spelled phonetically or misspelled in the raw intercom request (e.g. “Mandarine” instead of “Mandarin”), and we corrected them manually. As well, when a language request was vague or related to a country, the national or most widely spoken language in that country was used in our analysis. For example, requests for “Chinese” were assumed to be “Mandarin,” and “Ethiopian” was assumed to refer to “Amharic.” Finally, as some patients requested multiple languages, the total number of calls and total number of languages were different. This allowed for analysis by call (not counting each individual language requested) as well as analysis by the languages requested across all calls (counting multiple languages per call individually).
Interpreter requests were analyzed by language requested and phone extension provided. Extensions were cross-referenced to a hospital location or medical service type. These locations and services were further categorized into inpatient services, outpatient clinics, urgent-care settings, or imaging centers. Requests were also analyzed for time placed and categorized based on whether the call was placed during hospital business hours (Monday to Friday, 8 AM to 4 PM, excluding holidays), during non-working weekday hours (Monday to Friday, after 4 PM and before 8 AM), during weekends, or MUHC-specific statutory holidays.
As all data were anonymized and any patient information was unidentifiable and the study did not directly involve human participants, the institutional review board determined that approval was not necessary. Nonetheless, the study adhered fully to the Declaration of Helsinki.
Results
A total of 1265 interpreter requests were placed between January 2018 and December 2020. In 2018, there were 545 interpreter requests across all sites, while there were 456 requests in 2019. Only 264 interpreter requests were placed between 1 January and 27 November 2020. On average, 1.49 requests were placed per day in 2018, 1.25 in 2019, and 0.80 between 1 January and 27 November 2020. Almost half of requests (n = 568; 44.9%) were placed from the Royal Victoria Hospital, about a quarter were placed from, respectively the Montreal General Hospital (n = 334; 26.4%) and the Montreal Children’s Hospital (n = 316; 25.0%), and a minority of calls came from the Lachine Hospital (n = 24; 1.9%) and from the Montreal Chest Institute (n = 23; 1.8%). Supplementary Table 2 shows a stratification of languages included in requests by hospitals.
A total of 883 (69.9%) intercom requests placed were during working hours (8 AM to 4 PM, Monday to Friday excluding statutory holidays), while 188 (14.9%) were requested during weekends. A total of 164 (13.0%) requests were placed on weekdays outside of working hours (Monday to Friday before 8 AM or after 4 PM). Finally, 29 (2.3%) requests were placed on statutory holidays. Supplementary Table 4 displays the languages requested stratified by time of request.
Also, more than half of calls (n = 828/1265; 65.5%) could be mapped to a location in the hospital; the rest did not include a recognized location. Of the mapped calls, 354 (42.8%) calls were placed for the emergency room and related emergency services, 245 (29.6%) were placed for outpatient clinics, and 190 (23.0%) for inpatient locations in the hospital. Around 28 (3.4%) were placed for medical imaging locations in the hospital (i.e. radiology imaging centers), while 11 (1.3%) were classified as “Other” locations in the hospital, such as security and cafeteria locations. The languages requested stratified by the specific locations in the hospital are shown in Supplementary Table 3.
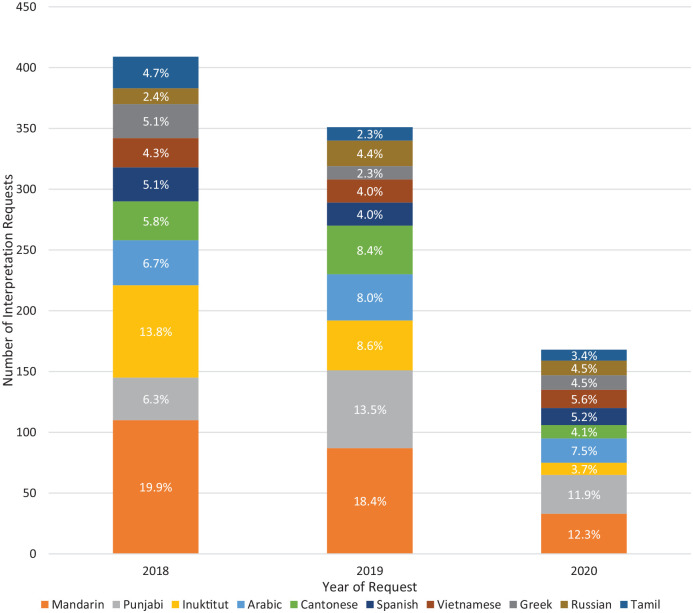
Some of these requests contained multiple languages. Therefore, there were 1294 languages requested across the 1265 calls requested including a total of 48 unique languages. Of these, the five most requested languages were Mandarin (230/1294 requests, 17.8%), Punjabi (131/1294 requests, 10.1%), Inuktitut (127/1294 requests, 9.8%), Arabic (95/1294 requests, 7.3%), and Cantonese (83/1294 requests, 6.4%). This proportion of the five most requested languages as compared to all requests, stratified by year, is shown in Figure 1. A list of the top-10 most requested languages, stratified by year is available in Table 1. A list of all languages requested stratified by year is available in Supplementary Table 1. All data reported in tables use the total number of languages requested (1294) rather than the total number of calls placed (1265).
Figure 1.
Number of interpretation requests stratified by year.
Total number of interpretation requests for the 10 most requested languages. Percentage of yearly requests per language is shown.
Table 1.
The top-10 most requested languages requested, stratified by year.
| Language | Number of requests | 2018 (%) | 2019 (%) | 2020 (%) |
|---|---|---|---|---|
| Mandarin | 230 (17.8) | 110 (19.9) | 87 (18.4) | 33 (12.3) |
| Punjabi | 131 (10.1) | 35 (6.3) | 64 (13.5) | 32 (11.9) |
| Inuktitut | 127 (9.8) | 76 (13.8) | 41 (8.6) | 10 (3.7) |
| Arabic | 95 (7.3) | 37 (6.7) | 38 (8.0) | 20 (7.5) |
| Cantonese | 83 (6.4) | 32 (5.8) | 40 (8.4) | 11 (4.1) |
| Spanish | 61 (4.7) | 28 (5.1) | 19 (4.0) | 14 (5.2) |
| Vietnamese | 58 (4.5) | 24 (4.3) | 19 (4.0) | 15 (5.6) |
| Greek | 51 (3.9) | 28 (5.1) | 11 (2.3) | 12 (4.5) |
| Russian | 46 (3.6) | 13 (2.4) | 21 (4.4) | 12 (4.5) |
| Tamil | 46 (3.6) | 26 (4.7) | 11 (2.3) | 9 (3.4) |
| Total | 928 (71.7) | 409 (74.1) | 351 (74.1) | 168 (62.7) |
Percentages use the number of language requests in that language and year as the numerator, and the total of language requests per year as the denominator.
Discussion
The goal of this analysis was to use a novel method of estimating the interpretation needs at university-affiliated teaching hospitals by analyzing intercom calls for ad hoc interpreters. We offer a first quantitative description of ad hoc interpretation at MUHC hospitals in Montreal, QC and highlight how these data can be used to inform implementation of professional interpretation services. To our knowledge, this is a first such description of the utility of intercom data.
In brief, over 3 years, 1265 intercom requests were placed for interpretation across five MUHC hospitals. The results show significant linguistic diversity at these hospitals, with 48 languages requested, the five most common being Mandarin, Punjabi, Inuktitut, Arabic, and Cantonese. These top languages represent 51.5% of all language requests. Most of the requests were made from urgent-care settings and during weekday working hours. Our findings show that ad hoc medical interpretation at MUHC hospitals is being used for a wide variety of languages despite the growing evidence against its efficacy.6,8–10 This further highlights the importance of implementing professional interpretation services at healthcare institutions.
By utilizing the intercom data, we can inform implementation of professional interpretation services in several ways. First, since five top languages represented over half of the requests, recruitment of interpreters speaking those languages could be a reasonable first step in addressing language barriers at the MUHC. Of note, the top-5 requested languages (Mandarin, Punjabi, Inuktitut, Arabic, and Cantonese) partially differ from the top-5 non-official languages of Montreal (Arabic, Spanish, Italian, Creole, and Mandarin), highlighting the importance of conducting hospital-level needs assessments rather than relying on the demographics of hospital’s catchment area. 15 Second, the urgent-care setting would be an appropriate site for initial service implementation, as 42.8% of the requests were made in that setting. An important consideration here is the mode of interpretation. Given the nature of the urgent-care setting, it is hard to predict the time and the language of the request and interpretation over the phone, or virtual interpretation might be more suitable. Finally, making professional interpreters available during working hours would address two-thirds of interpretation needs.
It is worth discussing several other trends in the data. The difference in the number of requests per hospital setting, hospital service, and working hours, may be explained by several factors, including the difference in patient volume, types of services offered (i.e. patients are more likely to bring friends or family to interpret for them to scheduled appointments as compared to emergency services), and access to interpretation services (i.e. Montreal Children’s Hospital offers an in-house interpretation service). In addition, the reduced number of interpretation requests in 2020 was likely due to the COVID-19 pandemic. This could in part be explained by reduced number of patients physically coming to the hospitals. Another contributing factor could have been HCPs’ reluctance to use in-person ad hoc interpreters amid the pandemic. Furthermore, as significant parts of healthcare service delivery moved online, the utility and usability of ad hoc interpretation was likely reduced. For this reason, our analysis likely underestimated the number of interpretation requests in 2020 and may suggest a need for remote interpretation services, for example, through videoconferencing or phone.
Limitations
It is important to keep in mind that intercom data likely underestimates the prevalence of language barriers. First, there is no evidence-based approach to determining the need for interpretation; therefore, many patients with language barriers are likely to be undetected. Second, we know that HCPs often rely on family members and colleagues who speak the language of the patient, data which are not captured by intercom method. 1 Third, many HCPs might not be aware or feel uncomfortable using the intercom system to request an ad hoc interpreter. Therefore, it is likely that our data only capture a subset of interpretation needs.
While these data help to elucidate the need for language interpretation at MUHC hospitals, it is limited in depth. Due to its retrospective nature, the data do not demonstrate the clinical circumstances that led to the request nor comments on whether the patient attempted to communicate first in English or French and was not understood. Similarly, the data do not indicate whether medical staff attempted to use a professional interpretation service before turning to the intercom system as the last resort. Furthermore, the data collected do not indicate whether the ad hoc interpretation request was answered or comment on the quality of the interpretation. In addition, our ability to effectively localize the origins of requests was limited as pertinent data were not available for all requests, which could have skewed the analysis stratified by location. To improve the depth of the data collected via intercom system, personnel collecting requests should be trained to consistently record data on the location and service requesting interpretation. Furthermore, an effort to collect data on effectiveness of the requests should be done. In the context of the COVID-19 pandemic, having interpreters available on call via telemedicine would ensure that interpretation requests can be readily met and reduce the risk of infectious disease spread.
Conclusion
This article presents a novel and reproducible method of analyzing interpretation requests to evaluate the interpretation needs in the hospital setting. These methods can be implemented in any hospital regardless of the request system. Results of such analysis can be used to design quality improvement interventions and guide implementation of professional interpretation services that can directly improve the quality of care offered to patients with language barriers. Specifically, at the MUHC, these data suggest the need for the implementation of interpretation services in urgent-care settings during working hours to address the five most common languages of Mandarin, Punjabi, Inuktitut, Arabic, and Cantonese.
Supplemental Material
Supplemental material, sj-docx-1-map-10.1177_27550834221105215 for Assessing needs for linguistic interpretation in hospital settings: A retrospective analysis of ad hoc interpreter requests by Nishaant Bhambra, Morgan Spencer Gold, Darya Naumova, Kenzy Abdelhamid, David Lessard and Bertrand Lebouché in Medicine Access @ Point of Care
Acknowledgments
D.L. is supported by the Canadian Institutes for Health Research Strategy for Patient-Oriented Research (CIHR SPOR) Mentorship Chair in Innovative Clinical Trials, owned by B.L.
Footnotes
Author contribution(s): Nishaant Bhambra: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing.
Morgan Spencer Gold: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing.
Darya Naumova: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing.
Kenzy Abdelhamid: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing.
David Lessard: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing.
Bertrand Lebouché: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing—original draft; Writing—review & editing.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: B.L. reports grants for investigator-initiated studies from ViiV Healthcare, Merck, and Gilead; consulting fees from ViiV Healthcare, Merck, and Gilead. He is the holder of a Canadian Institutes for Health Research, Strategy for Patient-Oriented Research Mentorship Chair in Innovative Clinical Trials for HIV Care and supported by a Senior Salary Award from Fonds de recherche du Québec-Santé (FRQS) (#311200) and the career award, LE 250, from the Quebec's Ministry of Health for researchers in Family Medicine. All other authors have no conflict of interest to declare.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Nishaant Bhambra  https://orcid.org/0000-0003-4966-6578
https://orcid.org/0000-0003-4966-6578
Supplemental material: Supplemental material for this article is available online.
References
- 1. Bowen S. Language barriers in access to health care. Ottawa, ON, Canada: Health Canada Ottawa, 2001. [Google Scholar]
- 2. Bowen S. The impact of language barriers on patient safety and quality of care. Ottawa, ON, Canada: Société Santé en Français, 2015, pp. 603–623. [Google Scholar]
- 3. David RA, Rhee M. The impact of language as a barrier to effective health care in an underserved urban Hispanic community. Mt Sinai J Med 1998; 65(5–6): 393–397. [PubMed] [Google Scholar]
- 4. Hampers LC, Cha S, Gutglass DJ, et al. Language barriers and resource utilization in a pediatric emergency department. Pediatrics 1999; 103(6 Pt. 1): 1253–1256. [DOI] [PubMed] [Google Scholar]
- 5. Impact of language barriers on patient satisfaction in an emergency department SpringerLink (Internet), https://link-springer-com.proxy3.library.mcgill.ca/article/10.1046/j.1525-1497.1999.00293.x [DOI] [PubMed]
- 6. Implications of language barriers for healthcare: a systematic review (Internet), https://www-ncbi-nlm-nih-gov.proxy3.library.mcgill.ca/pmc/articles/PMC7201401/ (accessed 10 November 2021). [DOI] [PMC free article] [PubMed]
- 7. Press TC. Hospital patients in Canada lacking English need access to interpreters, study says CBC News (Internet). CBC, 2019, https://www.cbc.ca/news/canada/british-columbia/patients-lacking-english-need-equal-access-to-interpreters-in-canada-study-1.5346763 (accessed 10 March 2022).
- 8. Health Canada. Language barriers in access to health care (Internet), 2003, https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-accessibility/language-barriers.html (accessed 29 May 2021).
- 9. Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev 2005; 62(3): 255–299. [DOI] [PubMed] [Google Scholar]
- 10. Flores G, Laws MB, Mayo SJ, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics 2003; 111(1): 6–14. [DOI] [PubMed] [Google Scholar]
- 11. Flores G, Abreu M, Barone CP, et al. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med 2012; 60(5): 545–553. [DOI] [PubMed] [Google Scholar]
- 12. These are the 20 best hospitals in Canada: report: Longwoods.com (Internet), https://www.longwoods.com/newsdetail/13457 (accessed 6 June 2021).
- 13. Lachine Hospital and Camille Lefebvre Pavilion (Internet). McGill University Health Centre, https://muhc.ca/lachine (accessed 6 June 2021).
- 14. Montreal Children’s Hospital (Internet). Montreal Children’s Hospital, https://www.thechildren.com/ (accessed 6 June 2021).
- 15. Government of Canada SC. Census profile, 2016 census: Montréal [Census metropolitan area], Quebec and Canada [Country] (Internet), 2017, https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=CMACA&Code1=462&Geo2=PR&Code2=01&Data=Count&SearchText=Montreal&SearchType=Begins&SearchPR=01&TABID=1&B1=All (accessed 10 May 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-map-10.1177_27550834221105215 for Assessing needs for linguistic interpretation in hospital settings: A retrospective analysis of ad hoc interpreter requests by Nishaant Bhambra, Morgan Spencer Gold, Darya Naumova, Kenzy Abdelhamid, David Lessard and Bertrand Lebouché in Medicine Access @ Point of Care