Abstract
Mental health problems among children and adolescents are increasingly reported amidst the coronavirus disease (COVID-19) pandemic. In this umbrella review, we aimed to synthesize global evidence on the epidemiologic burden and correlates of child and adolescent mental health (CAMH) problems during this pandemic from existing systematic reviews and meta-analyses. Adopting the Joanna Briggs Institute (JBI) methodology, we evaluated 422 citations and identified 17 eligible reviews with medium to high methodological quality. Most of the reviews reported a high prevalence of anxiety, depression, sleep disorders, suicidal behavior, stress-related disorders, attention-deficit/hyperactivity disorder, and other mental health problems. Also, factors associated with CAMH such as age, gender, place of residence, educational attainment, household income, sedentary lifestyle, social media and internet use, comorbidities, family relationships, parents' psychosocial conditions, COVID-19 related experiences, closure of schools, online learning, and social support were reported across reviews. As most studies were cross-sectional and used nonrepresentative samples, future research on representative samples adopting longitudinal and intervention designs is needed. Lastly, multipronged psychosocial care services, policies, and programs are needed to alleviate the burden of CAMH problems during and after this pandemic.
Keywords: Mental health, Psychiatry, Psychology, COVID-19, Pandemic, Child health, Adolescent health, Systematic review, Meta-analysis, Umbrella review
1. Introduction
The world has become acquainted with the coronavirus disease 2019 (COVID-19) pandemic that has triggered a wide range of biological, psychological, and socioeconomic consequences globally (Bashir et al., 2020; Bialek et al., 2020; Fauci et al., 2020). A growing body of empirical research informs a high burden of mental health problems in recent times that is increasingly recognized as a psychiatric epidemic synergistically occurring alongside this pandemic (Hossain et al., 2020; Robinson et al., 2022). Several reviews suggested a heavy psychosocial impact of COVID-19 pandemic resulting in mental health problems such as anxiety, depression, posttraumatic stress disorders (PTSD), and sleep disorders (Hessami et al., 2020; Ren et al., 2020; Robinson et al., 2022; Şimşir et al., 2021; Wu et al., 2021). An umbrella review of eight systematic reviews and meta-analyses found that preventive measures such as quarantine and isolation for infection prevention may have immediate and prolonged mental health impacts (Hossain et al., 2020a). This evidence suggests ongoing and future mental health crises associated with this pandemic that should be investigated and addressed across various population groups globally.
Mental health problems in childhood and adolescence are unique as they have versatile correlates and may have long-term health biopsychosocial consequences (Bassuk et al., 2015; Lund et al., 2018; Yoshikawa et al., 2012). The global prevalence of mental health disorders in children and adolescents has been inconsistent yet high across previous syntheses of research (Polanczyk et al., 2015; Silva et al., 2020). Specifically, several childhood mental health problems, including depression and anxiety, have become highly prevalent over the past years (Bassuk et al., 2015; Polanczyk et al., 2015; Silva et al., 2020; Wu et al., 2021). For example, a recent study found that the incidence of depression or anxiety in ages 6 to 17 has risen from 5.4% in 2003 to 8.4% in 2011–2012 in the US (Bitsko et al., 2018). Another study that was published in 2010 reported that 1 in 5 US children experience a serious or debilitating mental health problem in their lifetime (Merikangas et al., 2010). Similar studies from Canada (Gadermann et al., 2022; Spady et al., 2001), Europe (Deighton et al., 2019; Kovess-Masfety et al., 2016), and Australia (Kamieniecki, 2001; Sawyer et al., 2018) suggest comparative high burden of child and adolescent mental health (CAMH) problems. Moreover, countries with limited resources, mostly those in the global south, often lack high-quality evidence on mental health epidemiology. Yet, emerging literature from many low- and middle-income countries suggests a high burden of CAMH problems in those contexts that is a global mental health concern (Hossain and Purohit, 2019; Patel, 2007; Patel et al., 2008). These numbers are expected to increase amidst and after the COVID-19 pandemic.
The impacts of the COVID-19 pandemic on the mental health outcomes of children have drawn considerable attention amongst global researchers. Children and adolescents constitute the most vulnerable population affected by the preventive measures for COVID-19, such as the closure of schools, leading to reduced interaction with peers, and lessened opportunities for physical activity and exploration (Larsen et al., 2021; Rajmil et al., 2021). These effects are expected to have adverse impacts on the welfare and mental health of children through sleeping disorders, depression, stress and anxiety (M. Hossain et al., 2020; Larsen et al., 2021). Studies conducted across the globe provide evidence of the detrimental impact of the pandemic on the mental health of adolescents (Jones et al., 2021). During the COVID-19 pandemic lockdown, the percentage of Bangladeshi children who suffered from mental health disturbances ranged from 43% for subthreshold disturbances to 7.2% for severe disturbances (Yeasmin et al., 2020). In Turkey, children of health workers had significantly higher anxiety levels measured using the State-Trait Anxiety Inventory for Children (STAI-C) than non-health workers’ children (Almis et al., 2022). In Ireland, a qualitative study showed that adolescents and children experienced increased rates of social isolation, maladaptive behavior, anxiety, and depression during the pandemic (O'Sullivan et al., 2021). Moreover, the pandemic resulted in a significant psychosocial impact on Chinese adolescents and children in terms of emotional distress, with a prevalence of 24.9% for anxiety, 19.7% for depression, and 15.2% for stress (Tang et al., 2021). Another systematic review of Chinese studies showed that the prevalence of COVID-19 related posttraumatic stress, sleep disorders, anxiety, and depression were 48%, 44%, 26%, and 29%, respectively (Ma et al., 2021).
An increasing body of primary studies has facilitated the development of many such reviews that should be synthesized to provide an extensive overview of all CAMH problems and their associated factors. Such systematic overview of reviews, also known as umbrella reviews, have become increasingly useful in understanding the evidence landscape in a given domain (Aromataris et al., 2015). The findings of an umbrella review can offer a “bird's eye” view of a scientific field that may help evidence-based decision-making, synthesizing future evidence, and conducting primary research on least-explored areas of knowledge and practice (Aromataris et al., 2015; Dang and Hou, 2021; M. M. Hossain et al., 2020b). This umbrella review aimed to summarize the global evidence on the epidemiological burden and correlates of mental health problems among children and adolescents during the COVID-19 pandemic from existing systematic reviews and meta-analyses. The results of this review can help understand and address mental health problems among children and adolescents in this pandemic and future public health emergencies.
2. Methodology
2.1. Guidelines, data sources, and search strategy
In this umbrella review, we have followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline (Page et al., 2021) and the Joanna Briggs Institute (JBI) recommendations (Aromataris et al., 2020). The conduct of an umbrella review aims to address the broader scope of a scholarly topic and related issues presenting a wide picture of existing evidence. Umbrella reviews identify and examine evidence from existing systematically conducted reviews through a rigorous process. In this umbrella review, we conducted an extensive literature search in PubMed/MEDLINE, APA PsycInfo, Academic Search Ultimate, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Health Source- Nursing/Academic Edition, Health Policy Reference Center, and Web of Science using a set of keywords as outlined in Table 1 .
Table 1.
Keywords and search strategy.
| Search query | Search topic | Search keywords (titles, abstracts, general keywords, and subject headings) |
|---|---|---|
| 1 | Condition/ outcome of interest | “mental health” OR “mental wellbeing” OR “mental well-being” OR “mental disorder*” OR “mental illness” OR “psychiatr*” OR “psychological health” OR “psychological distress” OR “psychological impact” OR “psychological outcomes” OR “psychological consequence*” OR “psychological comorbid*” OR “psychosocial problem*” OR “behavioral problem*” OR “behavioral disorder*” OR “cognitive disorder*” OR “cognitive impairment*” OR “emotional distress” OR “depression” OR “depressive disorder*” OR “anxiety” OR “PTSD” OR “PTSS” OR “posttraumatic” OR “posttraumatic” OR “addiction” OR “substance use disorders” OR “mood disorder*” OR “affective disorder*” OR “DSM*” OR “psychosis” OR “psychotic” OR “oppositional defiant disorder” OR “hyperactiv*” OR “conduct disorder” OR “obsess*” OR “phobi*” OR “schizophren*” OR “bipolar disorder” OR “anorexia” OR “bulimi*” OR “challenging behav*” |
| 2 | Population | “child*” OR “adolescen*” OR “young people” OR “school students” OR “youth” OR “teen*” |
| 3 | Exposure/ Context | “Coronavirus” OR “COVID-19” OR “COVID19” OR “SARS-CoV-2” OR “2019 novel coronavirus” OR “2019-nCoV” |
| 4 | Phenomenon | “prevalence” OR “incidence” OR “rate” OR “diagno*” OR “disease burden” OR “epidemiolog*” OR “frequen*” OR “determinant*” OR “predictor*” OR “correlate*” OR “risk factors” OR “protective factors” OR “associated factors” |
| 5 | Study types | “systematic review” OR “systematic literature review” OR “meta-analy*” OR “metaanaly*” OR “quantitative review” OR “qualitative review” OR “meta-synthesis” OR “pooled prevalence” OR “pooled estimate*” OR “scoping review” OR “critical review” OR “integrative review” OR “evidence-based review” OR “synthesized evidence” |
| Final search query | Intersection of four topics | 1 AND 2 AND 3 AND 4 AND 5 |
3. Inclusion criteria
3.1. Participants
This review focused on children and adolescents irrespective of the age range adopted in systematic reviews and the primary studies included in the same. For studies with mixed participants such as adolescents with young adults or children as a part of other population groups, a decision was made prior to conducting the review about including a review if at least 70% of its studies focused on children or adolescents.
3.2. Phenomenon of interest
This review studied a wide range of mental health problems, including but not limited to psychiatric disorders enlisted in the Diagnostic and Statistical Manual of Mental Disorders (DSM–5) and the International Classification of Diseases (ICD-10) Classification of Mental and Behavioral Disorders. To make the evidence inclusive of any problem that affects mental health and wellbeing, this review considered research that emphasized psychosocial problems alongside psychiatric conditions.
3.3. Context
The context of this review was the COVID-19 pandemic. Therefore, studies conducted during and in the context of this pandemic were considered eligible for this review. If a review used data collected beyond the scope of this pandemic, it was considered ineligible for inclusion. Moreover, studies with mixed data from COVID-19 and previous infectious outbreaks were reviewed carefully. In such cases, a study was considered eligible if at least 70% of the respondents on included studies informed evidence in the context of COVID-19.
3.4. Types of studies
Any review article with a systematic approach to retrieve and synthesize evidence was considered eligible for inclusion in this umbrella review. This decision was made considering methodological differences within systematically conducted review articles. Therefore, systematic literature reviews, scoping reviews, and meta-analyses were included, whereas primary studies or narrative reviews without a clear review method were excluded. Moreover, articles were included in the full text was available in the English language. Lastly, studies published from January 1, 2020, to December 31, 2021, were primarily included in this review, and the search was last updated on March 12, 2022.
4. Study selection
We collated and uploaded all identified citations were to the cloud-based screening tool Rayyan. Two reviewers independently reviewed those citations using the above-mentioned criteria. All conflicts were addressed through a discussion, and the opinion of a third reviewer was taken whenever it was necessary. Articles that appeared to be qualified at this stage were considered for full-text review, and a final set of articles meeting all eligibility criteria was retained for data extraction and synthesis.
5. Data extraction and synthesis
We used a standardized data extraction form that included key variables of interest such as the bibliographic information of each article, the type of the reviews, number of primary studies, databases accessed in respective reviews, characteristics of the study samples and populations, epidemiologic measures used in those studies, and finally, the burden of mental health problems and factors associated with the same. Two reviewers (FN and AD) conducted the data extraction independently in the supervision of a third reviewer (ST). The extracted data were further reviewed for accuracy and quality by another reviewer (MMH). As this review included a wide range of systematically conducted reviews with and without quantitative synthesis, there was marked heterogeneity in the methods and outcomes of the included reviews. For this reason, a narrative synthesis of overall evidence on the burden of and factors associated with mental health problems in children and adolescents during the COVID-19 pandemic was presented in this review.
6. Assessment of methodological quality
In this umbrella review, we used the JBI checklist for the critical appraisal of systematic reviews and research syntheses to assess the methodological quality of studies included in this umbrella review (Aromataris et al., 2020, 2015). This checklist has ten items evaluating different methodological aspects of a systematically conducted review, including the appropriateness of the search strategies, the approach to synthesizing evidence, potentials sources of biases, and prospects for future research and policymaking. We used this ten-items checklist and allocated one point for each item. So, the overall score of a study can range from zero to ten. In this review, studies receiving zero to four, five to seven, and eight to ten points were categorized as the low, medium, and high-quality studies, respectively. The epidemiologic burden of CAMH and other key findings of this review were similar across reviews irrespective of their methodological quality.
7. Results
7.1. Overview of the included studies
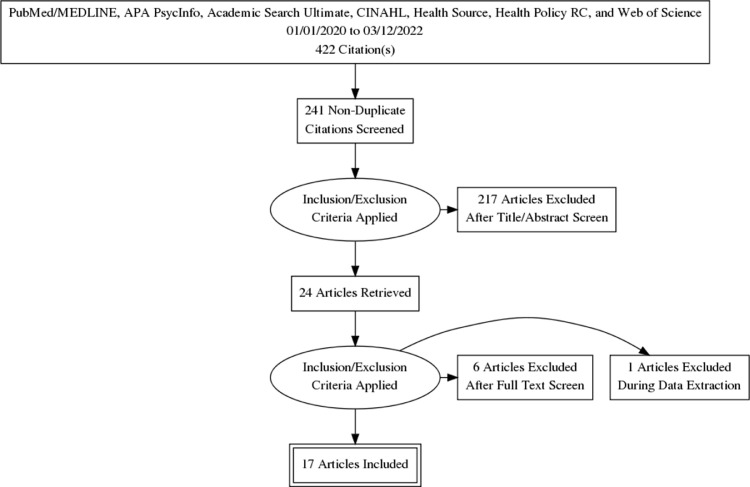
We found a total of 422 citations using the search strategy described earlier (See Fig. 1 for the review process). After eliminating 181 duplicate citations, we retained 241 unique citations and reviewed their titles and abstracts. A total of 24 citations met our preliminary criteria and were retained for full-text review. After full-text evaluation, 17 systematic reviews (Bussières et al., 2021; Chai et al., 2021; Chawla et al., 2021; Cunning and Hodes, 2022; Elharake et al., 2022; Jones et al., 2021; Ma et al., 2021; Marchi et al., 2021; Nearchou et al., 2020; Oliveira et al., 2022; Panchal et al., 2021; Panda et al., 2021; Racine et al., 2021; Samji et al., 2021; Sanja et al., 2021; Sharma et al., 2021; Viner et al., 2022), including 6 meta-analytic reviews (Bussières et al., 2021; Chai et al., 2021; Ma et al., 2021; Racine et al., 2021; Sanja et al., 2021; Sharma et al., 2021) met all criteria of this umbrella review and were selected for further analysis (see Table 2 ).
Fig. 1.
Flow diagram of the umbrella review process.
Table 2.
Overview of evidence from existing systematic reviews and meta-analyses on CAMH problems during COVID-19.
| Author and year ofPublication | Name(s) and timeframe of searchingDatabases | Number of primarystudies; type of review(meta-analysis orsystematic review) | Sample sizes in the includedprimary studies (total or rangeas reported in respectivereviews) | Methodological quality score and rating | Characteristics of the study populations(demographics, recruitmentstrategy, and location) | Burden of mental health (prevalence, rate, correlates or any quantitative measures of epidemiologic burden) | Factors associated with children and adolescent mental health in respective studies |
|---|---|---|---|---|---|---|---|
| Nearchou et al. (2020) | APA PsycInfo, MEDLINE, CINAHL, Scopus, PubMed, Embase, ERIC, and the WHO Global Health database till June 2020 |
12; Systemic Review | Sample size range from 17 to 8072. | 8 (High) | The study focused on human participant ≤18 years old; applied quantitative cross-sectional design; data collected through online and open access forum; conducted in China, Italy, Poland, Turkey, and United State | The prevalence of depression and anxiety in young people ranged from 22.6% to 43.7%. and 18.9% to 37.4% respectively. Moreover, among children and adolescent 22%−62.2% were found to have Covid-19 related emotional reaction as well as 2.39%−22% in terms of having somatic syndrome | Factors like fear of affecting with Covid-19, social distancing, Covid-19 circumstances, and emergencies were found to be associated with mental health outcome. However, some positive domains were found such as belongingness, relationship with peer, hope, meaning of life, life satisfaction. |
| Panda et al. (2021) | MEDLINE, Embase, Web of Science, CENTRAL, medRxiv and bioRxiv till August 2020 | 15; Systemic Review | Sample size range from 50 to 8079 | 9 (High) | The study included children up to 18 year and their caregiver; participants are recruited through direct and online interview; studies were cross-sectional design from France Italy, China, India Hong Kong, Brazil, Turkey, Bangladesh and Korea were reported | Studies had found 79.4% children were found to have psychological state due to the pandemic while 22.5%, 35.2%, 21.3% suffered from fear of covid-19 infection, boredom, and sleep disturbance respectively. Overall, 34.5%, 41.7%, 42.3% and 30.8% of children were found to be suffering from anxiety, depression, irritability, and inattention. Similarly, 52.3% and 27.4% of caregivers developed anxiety and depression, respectively. | Studies found multiple associated factors like female, urban citizen, clinical depression level, family member infected with covid-19, non-medical occupation, poor academic records, addicted to internet or smartphone. On the other hand, higher exercise, knowledge on covid-19, prevention, and control measures, having siblings found to be protective factors. |
| Bussières et al. (2021) | MEDLINE, ERIC, APA PsycInfo, and Google Scholar till June 2021 | 28; Meta-Analysis | Sample size ranges from 12 to 8124; total of 14,209 participants. | 10 (High) | Children aged 5–13 years old (including pre-existing conditions like ASD, epilepsy, obesity) were recruited; The quantitative synthesis of cross sectional, longitudinal and retrospective studies done; most study were from European countries followed by middle east then America | Studies found that children demonstrated longer sleeping hours (g = 0.324; 95% CI [0.10, 0.55]; p = 0.004; k = 9) and higher levels of both internalized (g = 0.215; 95% CI [0.06, 0.37]; p < 0.001; k = 19) and externalized (g = 0.141 (95% CI [0.08, 0.21]; p < 0.01; k = 15) symptoms during lockdown. effect sizes in studies where the child was the informant (g = 0.57; 95% CI [−0.36, 1.50]; p = 0.23; k = 3) | |
| Chai et al. (2021) | PubMed, Web of Science, APA PsycInfo, Google Scholar, and the China National Knowledge Infrastructure (CNKI) till March 2021 |
12; Meta-Analysis | Total sample size 34,276. Sample size ranges from 396 to 8079. | 9 (High) | The studies recruited Chinese children and adolescents; all data collected through online measures; Studies were conducted in China | The pooled prevalence of mental problems was 28% (95% confidence interval, CI: 0.22–0.34) while for depression it was 22% (95% CI: 0.16–0.30) and for anxiety it was 25% (95% CI: 0.20–0.32) | The percentage of boy participants was found to be an associated moderator factor. |
| Chawla et al. (2021) | PubMed, Cochrane, WHO global health research till March 2021 | 102; Systemic review | Sample size ranges from 61 to 10,000. | 9 (High) | The children/ adolescents with psychological effects, communication issues, stress or sleep disturbances were recruited; Age of participants ranges from pre-schoolers to 24; Online survey and telephone interview were conducted; Most of the studies were cross sectional or retrospective design and recruited participants from China |
Studies found mostly 10%−30% participants suffered from different level of depression and anxiety. | Being women and older aged found to be aggravating factor for anxiety and depression. Furthermore, factors like reduced physical activity, increased internet use, screen time and social media use, sedentary lifestyle were associated with severe anxiety. According to most of the studies, reduced sleep latency, increased sleep time as well as reduced sleep quality was correlated with the condition. |
| Cunning et al. (2022) | PubMed, MEDLINE, APA PsycInfo, AMED, BNI, CINAHL, Embase, EMCare and HMIL till January 2021 | 6; Systemic review | Sample size ranges from 101 to 600 participants | 5 (Medium) | The children and adolescent under age 21 having symptoms of OCD were included in this study; recruitment strategies were not specified, the studies were conducted in Denmark, Israel, the USA, Turkey, and Iran | The prevalence of OCD among adolescents ranged from 44.6% to 73% causing exaggerating symptoms | Being female seemed to be an exaggerating factor with slightly higher prevalence (72.1%) than men. Studies found some more associated factors like family history of ADHD, financial strain, or new unemployment, increased age, family accommodation. |
| Sanja et al. (2021) | Ovid MEDLINE, Embase, Global Health and APA PsycInfo till November 2020 | 27; Meta-Analysis | Total sample size 52,797. | 7 (Medium) | The study recruited children and adolescents from 6 to 19 years old (54.12% were female); recruitment strategies were not specified; conducted in Asia (20%), Europe (50%), America (20%0, Africa (5%), Oceania (5%) | After pandemic, the prevalence of anxiety is 49.5% and severe anxiety is 20.5% (p < 0.0001), for depression it is 16% among adolescents | Factors to increase anxiety and depression level are female gender (32.2%, M = 2.85, SE = 0.06), smartphone and internet addiction, low family income, perceived threats, higher grades at school, loneliness, social distancing, poor academic records, social stigma, friends or family conflict, emotion-focused coping. |
| Jones et al. (2021) | EBSCOhost, MEDLINE, APA PsycInfo, APA Psych articles, Socindex, and CINAHL till January 2021 |
16; Systemic Review | Sample sizes varied from 102 to 9554. | 8 (High) | 13–17 years old adolescents along with mental illness were included in this study; 75% studies conducted through online measures, and 25% not clearly reported; recruited in China, UK, the USA, Canada, Germany, Japan, Denmark and Philippine | The pandemic increased the likelihood of anxiety (OR = 2.29, 95% CI: 1.94–2.48 for low support, OR = 3.18, 95% CI: 2.54–3.98 for moderate support) and 31% of the adolescents reported of depression. Also 16.3% adolescents suffered from psychological impairment and experienced higher rates of posttraumatic stress disorder (PTSD) (effect size beta = 0.16∼0.27) and higher rates of anxiety (effect size beta = 0.32∼0.47) | Factors which worsened the condition by social media (OR = 1.8, 95% CI: 1.29–2.8) and internet addiction (OR = 3.1 95% CI: 1.2–7.7). Female gender, social distancing, negative coping skills, adolescents with diagnosed OCD (44.6%) found to worsen the condition. |
| Ma et al. (2021) | PubMed, APA PsycInfo, and Web of Science, and two Chinese academic databases: China National Knowledge Infrastructure (CNKI) and Wanfang September 2020 | 23; Systemic review & 20; Meta-Analysis. | Sample size vary from 46 to 9554; total sample size 57,927. | 10 (High) | The studies focused on the children and adolescents age up to 18 years, with suicidal behavior, suicidal ideation and attempt; computer-based simulation studies with no human participants, most study were from China 2 study from turkey | The prevalence of depression ranged from 10 to 71% with a pooled prevalence of 29% (95%CI: 17%, 40%). The prevalence of anxiety ranged from 7%−55% with a pooled prevalence of 26% (95%CI: 16%, 35%). Prevalence of sleep disorder was between 32%−56%, with a pooled prevalence of 44% (95%CI: 21%, 68%). The pooled prevalence of PTSD was 48% (95%CI: −0.25, 1.21, p = 0.200) |
Females gender with age between 13 and 18 year were found to be higher risk factors for both anxiety s (29.1%, 95%CI: 17.1%, 41.1%, p < 0.001) and depression (33.9%, 95%CI: 24.6%, 43.1%, p < 0.001). |
| Marchi et al. (2021) | PubMed, APA PsycInfo, Web of Science, CINHAL, and Social Science Premium Collection till December 2020 | 59; Systematic scoping review | 7 (Medium) | The study focused on child and adolescent below 18 years old; Study was identified in an iterative way; most of the study were took in China and United states | The prevalence of depression and anxiety among children and adolescents ranges from 2%−44%. And these symptoms seemed to reach peak around April-May with the decline by May-June 2020 | The protective factors found to be associated with the symptoms were strong resilience, positive emotion regulation, physical activity, parental self-efficacy, family functioning, social support. On the other hand, negative factors to impact were emotional reactivity, experiential avoidance, exposure to excessive information, internet use, closure of schools, social isolation, decline support from friend, family's crisis related hardships (such as job loss, income loss, caregiving burden, and illness). | |
| Panchal et al. (2021) | Embase, Ovid, Global Health, APA PsycInfo, Web of Science, and pre-print databases till April 1, 2021 |
61; Systemic review | Sample size ranges from 15 to 7772. | 9 (High) | The children and adolescent ≤19 years old (female 49.7%) exposed to covid 19 lockdown were included in this study; most study involved participant through self-report; studies were conducted across 5 continents, Europe (n = 35), Asia (n = 22), Australia(n = 1), North America (n = 1), South America (n = 1). | The prevalence of anxiety and depression ranges from 1.85 to 49.5% and 2.2% to63.8% respectively, Irritability ranged from 16.7%−73.2% and anger from 30%−51.1%. Symptoms of ADHD ranges from 55.9% to 76.6% (p < 0.001); sleeping disorder observed among 55.6% adolescents and 20% children. In addition, The prevalence of non-suicidal self-injury (OR = 1.35, (p < 0.001), suicide ideation (OR = 1.32, p = 0.008), suicide planning (OR = 1.71, p < 0.001), suicide attempts (OR = 1.74, p < 0.001) | Risk factors to increase anxiety and depression are lack of routine (p < 0.001), female sex (p < 0.001), adolescence (p = 0.005), excessive COVID-19 information (p < 0.05), media exposure (OR = 2.4), previous r psychiatric treatment (OR = 4.4), increased social media usage s (OR = 1.83, p = 0.001), suffering from Autism Spectrum Disorder, high amount of COVID-19 cases in the area (OR = 2.3, p < 0.001), first-line job responsibilities related to COVID-19 (p < 0.05). The protective was found to be all types of routine, family communication, social support, appropriate play, leisure and physical activity. |
| Racine et al. (2021) | PsycInfo, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, and MEDLINE till February 2021. | 29; Meta- Analysis | Total sample size 80,879; sample size ranges from 168 to 8079. | 9 (High) | Participants up to 18 years old (mean age 13 years) were included in this study; recruitment strategies were not specified; Studies were performed in East Asia (n = 16), Europe (n = 4), North America (n = 6), South America (n = 2) and middle east (n = 1) | The pooled prevalence rate for depression and anxiety are 25.2% (95% CI, 0.21–0.30) and 20.5% (95% CI, 0.17–0.24) respectively. The rate in European countries is higher (k = 4; rate = 0.34; 95% CI, 0.23–0.46; P = 0.01) in comparison to East Asian countries (k = 14; rate = 0.17; 95% CI, 0.13–0.21; P < 0.001) | For depression, the rate is increased with the increased months of year (b = 0.26; 95% CI,0.06–0.46), increased child age (b = 0.08; 95% CI, 0.01–0.15), for female (b = 0.03; 95% CI, 0.01–0.05). Again, For anxiety, the rate is increased with the increased months of year (b = 0.27; 95% CI, 0.10- 0.44), for female (b = 0.04; 95% CI, 0.01–0.07). |
| Samji et al. (2021) | MEDLINE, PsycInfo, PubMed, Embase, CINAHL, Web of Science, medRxiv, PsyArxiv, and Scopus till February 2021. |
116; Systemic review | Total sample size 127,923. | 8 (High) | The studies include youth up to 18 years of age, one third of the studied focused on neurodiverse conditions such as ASD, ADH and OCD; studies were performed in East Asia, north America, south Asia, Australia, West Asia, South America, Southeast Asia, Sub-Saharan Africa and North Africa | The prevalence of depression and anxiety raged from 13%−64% and 8%−74% respectively. Moreover, prevalence of suicidal ideation ranged from 6%−37% and non-suicidal self-injury increased from 32% to 42% | Older age and female gender were positively associated the symptoms. Studies found some more aggravating factors like more screen time, internet use, social media, physical and social distancing, pandemic control measures, increased time at home, lack of daily routine, online learning of children, adverse childhood experiences (family abuse, neglect, and household dysfunction), covid-19 news, suffering from ASD, ADHD. However, some protective factors may improve the symptoms like engaging in hobbies, listening to music, praying, maintaining a routine, physical activity, Increasing knowledge and awareness of COVID-19 prevention and control measures. |
| Sharma et al. (2021) | MEDLINE, Embase, and Web of Science | 16; Meta-Analysis | Total sample size 21,018; sample sizes ranges from 37 to 7736. | 10 (High) | Studies includes children, adolescents and youth age ranging from 6 months to 29 years; all the studies recruited through online surveys; location of the studies were not specified. | The pooled prevalence of any sleep disturbance in children during the COVID-19 pandemic was 54% (95%CI: 50%−57%). The pooled prevalence of children with worsening of sleep quality and sleep duration were 27% (95% CI: 12%−49%) and 16% (95%CI: 5%−40%) respectively. The pooled prevalence of children not meeting sleep duration recommendation was 49% (95%CI: 39%−58%) | The positive factors to improve sleep quality are harmonious family atmosphere, increased parent-children communication, good parenting practice, younger parent, parents in physical activity, parents discouraging screen time, parents encouraging children to sleep. The associated negative factors were poor maternal factors (poor sleep pattern, poor self-control, poor control of emotion, Maternal COVID-19 anxiety), decreased outdoor activities, female gender etc. |
| Elharake et al. (2022) | PubMed and Collabovid; January 2020- July 2021 | 5; Systematic review | Sample size ranged from 584 to 4342 | 7 (Medium) | Five studies included children and 16 studies included college students with varying ages; studies were from China, India, France, Jordan, Nigeria, Switzerland, and the US | The prevalence of depression (11.78% - 22.6%), anxiety (18.9% - 24.9%), PTST (14%) and stress (15.2%) were reported among children-based samples. Among the college students, 4.18% - 50.3% had depression, 7.7% - 79.66% had anxiety, 24.7% - 71% had stress, and 30.8% - 67.05% had PTSD symptoms. | Risk factors associated with adverse mental health outcomes in children included lower parents educational attainment and having a family member infected with COVID-19. Moreover, among college students, several factors such as family financial challenges, food insecurity (less than three meals per day), living in rural areas, closed on infected with COVID-19 were associated with poor mental health outcomes. |
| Oliveira et al. (2022) | Embase, Epistemonikos, LILACS, APA PsycInfo, PubMed, Scopus, Web of Science, WHO Covid database, and Google Scholar; up to February 1, 2021 | 19; Systematic review | More than 35,543 children and adolescents were included | 9 (High) | 17 cross-sectional and two cohort studies were conducted using internet based approaches; nine countries were represented- most studies were from China | The prevalence of fear (61.9%), helplessness (66.1%), worry (68.5%), emotional problems (27.4%), anxiety (17.6% - 43.7%), depression (6.3% - 71.5%), stress (7% - 25%), PTSD (85.5%), suicidal ideation (29.7% - 31.3%) behavioral problems (5.7% −13.9%) were reported across the included studies | Differences were observed between age groups (6–18 years versus 2–8 years) and responders (parents versus self-reported) |
| Viner et al. (2022) | PubMed, PsycInfo, Web of Science Social Citation Index, Australian Education Index, British Education Index, Education Resources Information centre, WHO Global Research Database on COVID-19, MedRxiv, PsyArXiv, Research Square, and COVID-19 Living Evidence; up to September 1, 2020 |
36; Systematic review | Studies included 79,781 children and 18,028 parents | 9 (High) | Five cohort studies, 9 pre-post studies, one modeling, and 21 cross-sectional studies were included; 13 studies were from LMICs (8 from China), 11 from UK, 4 from the US, 5 from Italy, and one study each from several countries | No significant increase in UK suicide rates; however, COVID-19 related problems were associated with 48% of the reported suicide deaths. The prevalence of anxiety (boys: 44%, girls: 53.3%, overall: 10%−21.8%), depression (boys: 21.9%, girls: 19.4%, overall: 17% - 28.6%), emotional difficulties (37%), suicidal ideation (17.5% in 16–18 years compared to 6% of pre-COVID estimates), conduct problems (43%), hyperactivity/inattention (41%), insomnia (23.2%), low life satisfaction (18% of 2001), low wellbeing (26.9% of 1201), child protection referral fell by 36% (156 per quarter in 2019 to 99 in 2020)56 to 39% (incidence rate ratio for 2020 compared with 2018/2019 was 0.61 [95%CI, 0.43–0.86]) |
School closure during lockdown was studied in the included studies highlighting the psychosocial impacts of such measures. Most studies found mental and emotional difficulties in this period, whereas a study with preexisting mental health problems in children found a significant reduction in emotional difficulties during lockdown. Child abuse reporting and referral services declines leading to low reporting. Increased social media and internet use, lack of healthy food consumption, and low-level of family education were reported across samples. |
7.2. Characteristics of the included studies
Seventeen reviews included in this umbrella review used different databases for retrieving primary studies. The number of databases ranged from 2 to 11 with a median number of 5 databases, whereas MEDLINE and WHO COVID-19 databases are the leading sources of information across multiple reviews.
The number of primary studies included in different reviews ranged from 5 to 102. Moreover, the sample size across studies ranged from 12 to 1199,320 in systematic reviews, whereas a meta-analytic review used a pooled sample of 80,879 participants (Racine et al., 2021). The majority of the primary studies were cross-sectional, and online data collection measures were widely used across studies. China was the most common source of primary studies, followed by the North American and European countries. Limited primary studies were reported from LMICs such as India, Brazil, Bangladesh, and countries from Sub-Saharan Africa (Elharake et al., 2022; Panchal et al., 2021; Panda et al., 2021; Racine et al., 2021; Samji et al., 2021; Sanja et al., 2021).
The methodological quality of the reviews was assessed using the JBI critical appraisal checklist (See Supplementary Material). Most of the reviews (n = 13) included in this umbrella review were of high quality (Bussières et al., 2021; Chai et al., 2021; Chawla et al., 2021; Jones et al., 2021; Ma et al., 2021; Nearchou et al., 2020; Oliveira et al., 2022; Panchal et al., 2021; Panda et al., 2021; Racine et al., 2021; Samji et al., 2021; Sharma et al., 2021; Viner et al., 2022), whereas the remaining (n = 4) reviews had medium quality (Cunning and Hodes, 2022; Elharake et al., 2022; Marchi et al., 2021; Sanja et al., 2021). None of the reviews were identified to have low methodological quality as per the JBI checklist.
8. Epidemiological burden of CAMH during COVID-19
8.1. Anxiety
Thirteen reviews reported a varying burden of anxiety among children and adolescents during this pandemic (Chai et al., 2021; Chawla et al., 2021; Jones et al., 2021; Ma et al., 2021; Marchi et al., 2021; Nearchou et al., 2020; Oliveira et al., 2022; Panchal et al., 2021; Racine et al., 2021; Samji et al., 2021; Sanja et al., 2021; Sharma et al., 2021; Viner et al., 2022). The prevalence of anxiety ranged from 1.85% to 74% across primary studies included in the reviews. For example, studies reported in the review by Panchal et al. (2021) found the prevalence of anxiety ranging from 1.85% to 49.5%. Another review by Samji et al. (2021) reported the prevalence of anxiety between 8% and 74%. A meta-analytic review by Racine et al. (2021) found that 20.5% (95% CI: 17% - 24%) participants had anxiety disorders during this pandemic.
8.2. Depression
Among the included studies, thirteen reviews and meta-analyses evaluated a high prevalence of depression among children and adolescents ranging from 2% to 71.5% (Chai et al., 2021; Chawla et al., 2021; Elharake et al., 2022; Jones et al., 2021; Ma et al., 2021; Marchi et al., 2021; Oliveira et al., 2022; Panchal et al., 2021; Panda et al., 2021; Racine et al., 2021; Samji et al., 2021; Sanja et al., 2021; Viner et al., 2022). For example, Marchi et al. (2021) found that the prevalence of depression was between 2% and 4% across the reviewed literature. Another review by Oliveira et al. (2022) reported the prevalence of depression between 6.3% and 71.5%. A meta-analytic review by Ma et al. (2021) reported the pooled prevalence of depression as 29% (95% CI: 17% - 40%) among children and adolescents.
8.3. Sleep disorders
Seven reviews reported varying magnitude of sleep disorders among children and adolescents during this pandemic (Bussières et al., 2021; Chawla et al., 2021; Ma et al., 2021; Panchal et al., 2021; Panda et al., 2021; Sharma et al., 2021; Viner et al., 2022). For example, Panchal et al. (2021) reported that the prevalence of sleep disorders was 20% and 55.9% among children and adolescents, respectively. Another review by Sharma et al. (2021) reported a pooled prevalence of any sleep disorders as 54% (95% CI: 50% - 57%), whereas the pooled prevalence of worsening sleep quality was 27% (95% CI: 12% - 49%) and the pooled estimate of abnormal sleep duration was 16% (95% CI: 5% - 40%).
8.4. Trauma and stress-related disorders
Four reviews examined the burden of posttraumatic stress disorders in different samples of children and adolescents (Elharake et al., 2022; Jones et al., 2021; Ma et al., 2021; Oliveira et al., 2022). For example, Ma et al. (2021) found a pooled prevalence of PTSD as 48%, whereas another review by Jones et al. (Jones et al., 2021) found that adolescents experienced a high effect size of PTSD (beta = 0.16 to 0.27). Another review by Elharake et al. (2022) found that 30.8% to 67.05% of the study samples had PTSD symptoms among young people amidst the COVID-19 pandemic. Moreover, three reviews have reported a varying burden of psychological distress and stress-related disorders (Elharake et al., 2022; Oliveira et al., 2022; Panda et al., 2021). For example, Oliveira et al. (2022) reported that 7% to 25% of children and adolescents experienced stress-related disorders amidst this pandemic.
8.5. Suicidal thoughts, ideations, and behavior
Four reviews studied the burden of suicidal thoughts, ideations, and self-harm behavior among children and adolescents during this pandemic (Oliveira et al., 2022; Panchal et al., 2021; Samji et al., 2021; Viner et al., 2022). For example, Panchal et al. (2021) reported a high prevalence of suicide ideation (OR = 1.32, p = 0.008), suicide planning (OR = 1.71, p < 0.001), suicide attempts (OR = 1.74, p < 0.001), and non-suicidal self-harm (OR = 1.35, p < 0.001). Another review by Samji et al. (2021) found that the prevalence of suicidal ideation ranged from 6% to 37%, and non-suicidal self-increased from 32% to 42% during this pandemic. Viner et al. (2022) found that the prevalence of suicidal ideation increased to 17.5% among adolescents aged 16–18 years compared to 6% of pre-COVID estimates.
8.6. Attention-deficit/hyperactivity disorder
Several empirical studies reported the burden of attention-deficit/hyperactivity disorder in children and adolescents during this pandemic that was synthesized in three reviews (Panchal et al., 2021; Panda et al., 2021; Viner et al., 2022). Viner et al. (2022) found that 41% of the participating children had hyperactivity/inattention, whereas Panchal et al. (2021) reported that the symptoms of ADHD ranged from 55.9% to 76.6% (p < 0.001) among children and adolescents across multiple studies. Panda et al. (2021) found that 30.8% of the participating children had attention-deficit symptoms alongside other mental health problems.
8.7. Other mental health problems
Several other mental health problems were reported in multiple reviews. Cunning et al. (Cunning and Hodes, 2022) reported that the prevalence of OCD among adolescents ranged from 44.6% to 73% causing exaggerating symptoms. Moreover, emotional disorders were reported by three reviews that found 22% to 62.2% of children and adolescents experienced emotional difficulties during this pandemic (Nearchou et al., 2020; Oliveira et al., 2022; Viner et al., 2022). A review by Nearchou et al. (2020) found that 2.39% to 37% of participants had somatic syndrome. Furthermore, psychological problems such as fear of COVID-19 (Oliveira et al., 2022; Panda et al., 2021), boredom (Panda et al., 2021), irritability (Panchal et al., 2021; Panda et al., 2021), internalized and externalized problems (Bussières et al., 2021), helplessness (Oliveira et al., 2022), conduct problems (Viner et al., 2022), and low life satisfaction (Viner et al., 2022) were reported across reviews. In addition, child protection referral fell by 36% (156 per quarter in 2019 to 99 in 2020) to 39% (incidence rate ratio for 2020 compared with 2018/2019 was 0.61 [95%CI, 0.43–0.86]), suggesting a potential burden of child abuse and related mental health problems (Viner et al., 2022). Overall mental and psychosocial health problems deteriorated across all reviews that included children, adolescents, and their family caregivers in respective empirical studies.
9. Correlates of mental health problems in children and adolescents during COVID-19
Multiple factors associated with mental health problems were identified across multiple reviews that affected the mental health of children and adolescents during this pandemic. The age of the children and adolescents was reported to be associated with mental health problems in different studies. For example, Chawla et al. (2021) found that older children and adolescents was an aggravating factor for anxiety and depression. Increased age was also reported as a risk factor by Cunning and Hodes (2022), Samji et al. (2021), and Ma et al. (2021). Specifically, Racine et al. (2021) found that increased child age was associated with a higher burden of depression (b = 0.08, 95% CI: 0.01 – 0.15). Moreover, differences in mental health outcomes were observed between participants aged 2–8 years and those aged 6–18 years in a review by Oliveira et al. (2022).
Gender was associated with mental health outcomes as reported in several reviews. Chai et al. (2021) reported the percentage of boys was a moderator of mental health outcomes across study samples. In contrast, several reviews reported girls had a higher burden of mental health problems during this pandemic. For example, female gender was associated with increased anxiety and depression level (32.2%, M = 2.85, SE = 0.06) as reported by Sanja et al. (2021). Another review by Panchal et al. (2021) found that the female gender was significantly associated with anxiety and depression (p < 0.001). Racine et al. (2021) reported that female participants had higher rates of depression (b = 0.03, 95% CI: 0.01 – 0.05).
Urban residence was found to be associated with mental health outcomes in a review by Panda et al. (2021), whereas Elharake et al. (2022) reported poor mental health outcomes in college students living in rural areas. Moreover, the time of the study appeared to affect the study outcomes. For example, Racine et al. (2021) found that later months of the year was associated with higher burden of anxiety (b = 0.27, 95% CI: 0.10 – 0.44) and depression (b = 0.26, 95% CI: 0.06 – 0.46). Furthermore, poor academic records were associated with adverse mental health outcomes in one review (Panda et al., 2021), whereas another review found that higher academic grades were associated with anxiety and depression (Sanja et al., 2021).
Several reviews synthesized evidence on behavioral and lifestyle-related factors associated with mental health problems. For example, Chawla et al. (2021) found that a sedentary lifestyle, increased screen time, and lack of exercise were associated with depression and anxiety. Physical activity and regular exercise were associated with improved mental health across multiple reviews (Chawla et al., 2021; Marchi et al., 2021; Panchal et al., 2021; Panda et al., 2021; Samji et al., 2021; Sharma et al., 2021). Staying home for increased duration and lack of daily routine affected mental health in many children and adolescents, as reported by Panchal et al. (2021) and Samji et al. (2021). A Review by Viner et al. (2022) found that a lack of healthy food consumption was associated with adverse mental health outcomes among children amidst this pandemic. Moreover, better emotional regulation and psychological resilience were associated with improved mental health outcomes. Furthermore, better knowledge about the pandemic was associated with better mental health among children and adolescents (Marchi et al., 2021), whereas excessive information was negatively associated with mental health, as reported by Panchal et al. (2021).
Individual behaviors such as hobbies, praying, and listening to music were reported to be associated with positive mental health (Samji et al., 2021). Internet and smartphone addiction appeared to be a common risk factor associated with mental health problems reported in several reviews (Chawla et al., 2021; Jones et al., 2021; Marchi et al., 2021; Panchal et al., 2021; Panda et al., 2021; Samji et al., 2021; Sanja et al., 2021; Sharma et al., 2021; Viner et al., 2022). Moreover, the past history of mental health problems was associated with adverse mental health outcomes, as reported in several reviews (Cunning and Hodes, 2022; Jones et al., 2021; Panchal et al., 2021; Samji et al., 2021; Viner et al., 2022). Severe events related to COVID-19 affected mental health among many children and adolescents. For example, Panda et al. (2021) found that having a family member who was infected with COVID-19 was associated with adverse psychological outcomes. Another review by Panchal et al. (2021) reported an increased number of COVID-19 cases within the same geographic area affected mental health (OR = 2.3, p < 0.001) in children and adolescents.
Several family issues were reported to be associated with mental health outcomes during this pandemic. Nearchou et al. (2020) found that belongingness and better relationships with closed ones were associated with improved mental health. Parental self-efficacy and family functioning were protective factors for mental health, as reported by Marchi et al. (2021). Moreover, adverse childhood and family experiences such as household dysfunction, family neglect, and child abuse were associated with poor mental health outcomes (Samji et al., 2021). Moreover, the parents education and responsiveness were associated with the mental health of children and adolescents (Elharake et al., 2022; Oliveira et al., 2022; Sharma et al., 2021; Viner et al., 2022). In addition, family financial crises affected the mental health of children and adolescents in many reviews. For example, unemployment and financial constraints affected families and the mental health of young people (Cunning and Hodes, 2022). Elharake et al. (2022) found that family financial challenges and food insecurity (less than three meals per day) affected mental health in children and college students.
School closure was associated with a wide range of mental health outcomes, as studied in a review by Viner et al. (2022) and Marchi et al. (2021). Specifically, Viner et al. (2022) found that child abuse referral reports declined during this pandemic due to school closure suggesting interrupted services in those contexts. As many institutions transitioned to online learning systems, Samji et al. (2021) found such online learning to be associated with adverse mental health outcomes in children and adolescents.
Social factors such as social isolation and distancing, social stigma, and social support were associated with overall mental health outcomes in many reviews (Jones et al., 2021; Marchi et al., 2021; Panchal et al., 2021; Samji et al., 2021; Sanja et al., 2021). For example, social distancing was associated with adverse mental health outcomes in a review by Jones et al. (2021). Moreover, Samji et al. (2021) reported that social distancing was associated with poor mental health outcomes. Both social stigma and social distancing were related to a higher burden of anxiety in a review by Sanja et al. Furthermore, Panchal et al. (2021) and Marchi et al. (2021) found social support to have a protective role on mental health outcomes in children and adolescents.
10. Discussion
This umbrella review provides a systematic overview of global evidence on CAMH during the COVID-19 pandemic from existing systematic reviews and meta-analyses. To the best of our knowledge, this is one of the few umbrella reviews on mental health in COVID-19 (Fernandez et al., 2021; Sahebi et al., 2021) and the first one emphasizing CAMH. The findings of this review may facilitate mental and child health policymaking and practice and inform further research strengthening the global knowledge base. In this review, we found a varying burden of several mental health problems such as anxiety, depression, sleep disorders, PTSD, suicidal behavior, psychological distress, and other psychosocial challenges among children and adolescents. Moreover, we identified several critical factors associated with mental health problems in this young population. Individual social demographic factors associated with mental health outcomes included older age of the children and adolescents, female gender, location of the residence, educational attainment, sedentary lifestyle, lack of routine activities, spending more time at home, social media addiction, Internet overuse, knowledge about pandemic or excessive information, emotional regulation, resilience, self-efficacy, physical activity and exercise behavior, recreational activities, spending time on hobbies, and history of mental health problems. Furthermore, several family-related factors associated with mental health were identified, which included belongingness and relationship with family members, parents’ education, household income and economic hardship, adverse childhood and family experience, and challenging family relationships. In addition, community and social factors related to mental health included social distancing practices, social support, social stigma, closure of the schools, online learning activities, and COVID-19 related life events and preventive measures. These factors influenced mental health outcomes among children and adolescents in different contexts as identified in existing reviews and respective primary studies included within those reviews.
Most studies reported a high prevalence of CAMH problems across contexts suggesting a heavy psychosocial impact of this pandemic that is consistent with other reviews conducted in different populations (Bourmistrova et al., 2022; Fernandez et al., 2021; Hossain et al., 2020; Li et al., 2021; Sahebi et al., 2021). Socioecological perspectives may inform the complex epidemiology of these crises emerging at different levels. Children and adolescents experienced an unusual interruption in their everyday lives that included prolonged stay within home, altered relationship dynamics with their caregivers and family members, less-frequent interactions with peers and relatives, lack of access to outdoor activities, changed nutritional and lifestyle behaviors and other changes at the household level (de Figueiredo et al., 2021; Settersten et al., 2020). These problems compounded the effects of community and social changes associated with this pandemic, which included social distancing, closure of schools and institutions, and interruption of health and social services (Barach et al., 2020; Nguyen et al., 2021; Viner et al., 2022). Lastly, universal challenges such as socioeconomic problems and health hazards of COVID-19 impacted children, adolescents, and their families that also affected mental health and wellbeing (Hossain et al., 2020; Marchi et al., 2021; Preston and Rew, 2022). Taken together, a variety of psychosocial stressors emerged during this pandemic, whereas mental health promotion and protective services were mostly disrupted or unavailable. These factors affected biopsychosocial health and wellbeing across populations resulting in a high burden of CAMH problems that require clinical, public health, social, and policy considerations.
The overall evidence on the epidemiologic burden of CAMH and associated factors reflected high heterogeneity that can be attributed to several factors. First, earlier studies on psychosocial impacts were conducted in China (Cunning and Hodes, 2022; Ma et al., 2021), whereas a majority of overall studies were from the US, UK, Canada, and several high-income countries (Bussières et al., 2021; Elharake et al., 2022; Racine et al., 2021; Viner et al., 2022). Although the synthesized evidence inform a global phenomenon of elevated psychosocial burden of CAMH problems, the current evidence gap reflects a lack of research equity that must be addressed. Most reviews informed a scarcity of evidence from the global south reflecting a critical knowledge gap in those contexts, which requires scholarly efforts to improve research quantity and quality in those regions. Another key challenge in the presented evidence is a critical lack of comparative statistics that could inform psychiatric epidemiologic changes in study populations. The availability of baseline and comparative data could have provided a better understanding of the mental health impacts amidst this pandemic. Moreover, online measures of collecting data and non-standardized scales were widely used in cross-sectional studies reported across reviews (Chawla et al., 2021; Cunning and Hodes, 2022; Elharake et al., 2022; Marchi et al., 2021; Nearchou et al., 2020), which may not provide representative estimates on CAMH impacts of COVID-19. Furthermore, cross-sectional studies may not inform temporal changes in mental health outcomes or how much psychosocial burden can be attributable to the pandemic or associated factors. Therefore, standardized measurements approaches should be used in representative samples and preferably in longitudinal and interventions studies that more accurately reflect the psychosocial impacts locally and globally. A brief overview of the recommendations for future research on CAMH is provided in Table 3 -A.
Table 3.
Evidence-based recommendations for future research, policymaking, and practice.
| Recommendations for future research, policymaking, and practice | |
|---|---|
|
|
|
|
The current evidence on CAMH problems amidst COVID-19 necessitates multipronged efforts to alleviate the immediate and future health and social consequences of this burden. The policymakers and practitioners need to evaluate the evidence-based guidelines and recommendations that may fit the mental health needs of children and adolescents in different contexts, as listed in Table 3-B. At the individual level, awareness of mental health and pandemic safety should be strengthened, addressing the fear of infection and health hazards (Chai et al., 2021; Cunning and Hodes, 2022; Panda et al., 2021; Sanja et al., 2021). Moreover, positive psychology-based targeted interventions should be promoted alongside public mental health interventions (Elharake et al., 2022; Mohd et al., 2022; Nearchou et al., 2020). Furthermore, parents, teachers, and other caregivers should be engaged in mental health promotion (Chai et al., 2021; Chawla et al., 2021; Marchi et al., 2021; Panda et al., 2021). As many scholars suggest, those formal and informal caregivers may require psychoeducational and behavioral support to stay healthy and contribute to interpersonal and community health efforts (Chawla et al., 2021; Marchi et al., 2021; Panchal et al., 2021). Also, healthcare professionals and social workers should be empowered to offer psychosocial care services to the affected children and adolescents in diverse settings (Panchal et al., 2021; Sanja et al., 2021). Institutional care services should be made available and accessible to address the growing burden of mental health epidemics accompanying COVID-19 pandemic (Mohd et al., 2022; Nearchou et al., 2020). Health systems and services must the strengthened to actualize these efforts at the societal level (Cunning and Hodes, 2022; Mohd et al., 2022; Sanja et al., 2021). Lastly, a stronger policy commitment is needed to improve social determinants of mental health in children and adolescents that may enable them to overcome the current mental health problems and develop resilience to better psychosocial outcomes in the future (Elharake et al., 2022; Panchal et al., 2021; Racine et al., 2021).
11. Limitations
This umbrella review has several limitations that must be addressed in future evidence syntheses. First, we included major databases but did not include preprint servers and other potential sources that may contain eligible reviews. Second, we identified multiple reviews with different methods and synthesized them narratively. A patient-level data synthesis from individual studies could have provided a more accurate and less overlapping view of the evidence landscape. Third, as systematic reviews and meta-analyses included primary studies published before conducting those reviews, a synthesis of the reviews is likely to miss insights from the most recent primary studies. Fourth, most primary studies included in this review were cross-sectional in nature, which is a limitation of the synthesized evidence as well. We call for longitudinal research that may strengthen the evidence base in primary research and future evidence synthesis. Lastly, heterogeneity and publication biases were not assessed in this narrative umbrella study. Understanding those and addressing the same should be prioritized in future meta-research.
12. Conclusions
Psychosocial stressors associated with the COVID-19 pandemic have resulted in a wide range of mental health problems in children and adolescents. The current evidence suggests a high burden of anxiety, depression, psychological distress, PTSD, sleep disorders, suicidal behavior, addiction disorders, and other psychosocial problems that require evidence-based measures to address the same. Also, many of these problems may persist and develop further mental health crises that should be addressed by adopting multifaceted psychiatric, psychological, and public health efforts. In this regard, context-specific risk assessment and management approaches should prioritize population mental health needs and address current gaps in mental health services. Transdisciplinary mental health research, policymaking, and practice should be emphasized to mitigate the mental health impacts of this pandemic and ensure optimal mental, physical, and social health of children and adolescents locally and globally.
Funding information
No funding was received at any stage of conceptualizing or conducting this umbrella review.
Declaration of the Competing Interest
The authors of this manuscript declared no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2022.114814.
Appendix. Supplementary materials
References
- Abrams E.M., Szefler S.J. COVID-19 and the impact of social determinants of health. Lancet. Respir. Med. 2020;8:659. doi: 10.1016/S2213-2600(20)30234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almis H., Han Almis B., Bucak I.H. Mental health of children of health workers during the COVID-19 pandemic: a cross-sectional study. Clin. Child Psychol. Psychiatry. 2022;27:104–111. doi: 10.1177/13591045211016527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aromataris, E., Fernandez, R., Godfrey, C., Holly, C., Khalil, H., Tungpunkom, P., 2020. JBI Manual for Evidence Synthesis - JBI Global Wiki [WWW Document]. JBI. URL https://jbi-global-wiki.refined.site/space/MANUAL/3283910768/Chapter+10%3A+Umbrella+reviews (accessed 3.19.22).
- Aromataris E., Fernandez R., Godfrey C.M., Holly C., Khalil H., Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 2015;13:132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- Asbury K., Fox L., Deniz E., Code A., Toseeb U. How is COVID-19 affecting the mental health of children with special educational needs and disabilities and their families? J. Autism Dev. Disord. 2021;51:1772–1780. doi: 10.1007/S10803-020-04577-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashcroft R., Lam S., Kourgiantakis T., Begun S., Nelson M.L.A., Adamson K., Cadell S., Walsh B., Greenblatt A., Hussain A., Sur D., Sirotich F., Craig S.L. Protocol: preparing social workers to address health inequities emerging during the COVID-19 pandemic by building capacity for health policy: a scoping review protocol. BMJ Open. 2021;11:53959. doi: 10.1136/BMJOPEN-2021-053959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barach P., Fisher S.D., Adams M.J., Burstein G.R., Brophy P.D., Kuo D.Z., Lipshultz S.E. Disruption of healthcare: will the COVID pandemic worsen non-COVID outcomes and disease outbreaks? Prog. Pediatr. Cardiol. 2020;59 doi: 10.1016/J.PPEDCARD.2020.101254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Shahzad L. A brief review of socio-economic and environmental impact of Covid-19. Air Qual. Atmos. Heal. 2020;13:1403–1409. doi: 10.1007/S11869-020-00894-8/FIGURES/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassuk E.L., Richard M.K., Tsertsvadze A. The prevalence of mental illness in homeless children: a systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54:86–96. doi: 10.1016/J.JAAC.2014.11.008. e2. [DOI] [PubMed] [Google Scholar]
- Bialek S., Bowen V., Chow N., Curns A., Gierke R., Hall A., Hughes M., Pilishvili T., Ritchey M., Roguski K., Silk B., Skoff T., Sundararaman P., Ussery E., Vasser M., Whitham H., Wen J. Geographic differences in COVID-19 cases, deaths, and incidence — United States. MMWR. Morb. Mortal. Wkly. Rep. 2020;69:465–471. doi: 10.15585/mmwr.mm6915e4. February 12–April 7, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsko R.H., Holbrook J.R., Ghandour R.M., Blumberg S.J., Visser S.N., Perou R., Walkup J.T. Epidemiology and impact of health care provider-diagnosed anxiety and depression among US children. J. Dev. Behav. Pediatr. 2018;39:395–403. doi: 10.1097/DBP.0000000000000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldt K., Coenen M., Movsisyan A., Voss S., Rehfuess E., Kunzler A.M., Lieb K., Jung-Sievers C. Interventions to ameliorate the psychosocial effects of the COVID-19 pandemic on children-A systematic Review. Int. J. Environ. Res. Public Health. 2021;18:1–31. doi: 10.3390/IJERPH18052361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourmistrova N.W., Solomon T., Braude P., Strawbridge R., Carter B. Long-term effects of COVID-19 on mental health: a systematic review. J. Affect. Disord. 2022;299:118–125. doi: 10.1016/J.JAD.2021.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussières E.L., Malboeuf-Hurtubise C., Meilleur A., Mastine T., Hérault E., Chadi N., Montreuil M., Généreux M., Camden C., Roberge P., Lane J., Jasmin E., Kalubi J.C., Bussiéres E.L., Hurtubise K., Bach G., Chrysagis M., Turner M.P., Gauvin C., Hérault E. Consequences of the COVID-19 pandemic on children's mental health: a meta-analysis. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.691659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai J., Xu H., An N., Zhang P., Liu F., He S., Hu N., Xiao X., Cui Y., Li Y. The prevalence of mental problems for chinese children and adolescents during COVID-19 in China: a systematic review and meta-analysis. Front. Pediatr. 2021;9 doi: 10.3389/fped.2021.661796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawla N., Tom A., Sen M.S., Sagar R. Psychological impact of COVID-19 on children and adolescents: a systematic review. Indian J. Psychol. Med. 2021;43:294–299. doi: 10.1177/02537176211021789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunning C., Hodes M. The COVID-19 pandemic and obsessive–compulsive disorder in young people: systematic review. Clin. Child Psychol. Psychiatry. 2022;27:18–34. doi: 10.1177/13591045211028169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang Y., Hou Y. The prognostic value of late gadolinium enhancement in heart diseases: an umbrella review of meta-analyses of observational studies. Eur. Radiol. 2021;31:4528–4537. doi: 10.1007/S00330-020-07437-W/TABLES/2. [DOI] [PubMed] [Google Scholar]
- de Figueiredo C.S., Sandre P.C., Portugal L.C.L., Mázala-de-Oliveira T., da Silva Chagas L., Raony Í., Ferreira E.S., Giestal-de-Araujo E., dos Santos A.A., Bomfim P.O.S. COVID-19 pandemic impact on children and adolescents’ mental health: biological, environmental, and social factors. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;106 doi: 10.1016/J.PNPBP.2020.110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deighton J., Lereya S.T., Casey P., Patalay P., Humphrey N., Wolpert M. Prevalence of mental health problems in schools: poverty and other risk factors among 28 000 adolescents in England. Br. J. Psychiatry. 2019;215:565–567. doi: 10.1192/BJP.2019.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elharake J.A., Akbar F., Malik A.A., Gilliam W., Omer S.B. Mental health impact of COVID-19 among children and college students: a systematic review. Child Psychiatry Hum. Dev. 2022 doi: 10.1007/s10578-021-01297-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauci A.S., Lane H.C., Redfield R.R. Covid-19 — navigating the uncharted. N. Engl. J. Med. 2020;382:1268–1269. doi: 10.1056/NEJME2002387/SUPPL_FILE/NEJME2002387_DISCLOSURES.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez R., Sikhosana N., Green H., Halcomb E.J., Middleton R., Alananzeh I., Trakis S., Moxham L. Anxiety and depression among healthcare workers during the COVID-19 pandemic: a systematic umbrella review of the global evidence. BMJ Open. 2021;11 doi: 10.1136/BMJOPEN-2021-054528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadermann A.M., Gagné Petteni M., Janus M., Puyat J.H., Guhn M., Georgiades K. Prevalence of mental health disorders among immigrant, refugee, and nonimmigrant children and youth in British Columbia, Canada. JAMA Netw. Open. 2022;5 doi: 10.1001/JAMANETWORKOPEN.2021.44934. e2144934–e2144934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hessami, K., Romanelli, C., Chiurazzi, M., Cozzolino, M., 2020. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. 10.1080/14767058.2020.1843155. [DOI] [PubMed]
- Hossain M., Purohit N. Improving child and adolescent mental health in India: status, services, policies, and way forward. Indian J. Psychiatry. 2019;61:415. doi: 10.4103/PSYCHIATRY.INDIANJPSYCHIATRY_217_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain, M., Tasnim, S., Sultana, A., Faizah, F., Mazumder, H., Zou, L., Lisako, E., Mckyer, J., Ahmed, H.U., Ma, P., Alonzi, S., Silverstein, M.W., 2020. Epidemiology of mental health problems in COVID-19: a review [version 1; peer review: 2 approved] report report. 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed]
- Hossain M.M., Sultana A., Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol. Health. 2020;42 doi: 10.4178/EPIH.E2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain M.M., Sultana A., Tasnim S., Fan Q., Ma P., McKyer E.L.J., Purohit N. Prevalence of mental disorders among people who are homeless: an umbrella review. Int. J. Soc. Psychiatry. 2020;66:528–541. doi: 10.1177/0020764020924689. [DOI] [PubMed] [Google Scholar]
- Jones E.A.K., Mitra A.K., Bhuiyan A.R. Impact of COVID-19 on mental health in adolescents: a systematic review. Int. J. Environ. Res. Public Heal. 2021;18:2470. doi: 10.3390/IJERPH18052470. 2021, Vol.Page18, 2470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamieniecki G.W. Prevalence of psychological distress and psychiatric disorders among homeless youth in Australia: a comparative review. Aust. N. Z. J. Psychiatry. 2001;35:352–358. doi: 10.1046/j.1440-1614.2001.00910.x. [DOI] [PubMed] [Google Scholar]
- Katz C., Fallon B. Protecting children from maltreatment during COVID-19: struggling to see children and their families through the lockdowns. Child Abuse Negl. 2021;116 doi: 10.1016/J.CHIABU.2021.105084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovess-Masfety V., Husky M.M., Keyes K., Hamilton A., Pez O., Bitfoi A., Carta M.G., Goelitz D., Kuijpers R., Otten R., Koç C., Lesinskiene S., Mihova Z. Comparing the prevalence of mental health problems in children 6–11 across Europe. Soc. Psychiatry Psychiatr. Epidemiol. 2016;51:1093–1103. doi: 10.1007/S00127-016-1253-0/TABLES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen L., Helland M.S., Holt T. The impact of school closure and social isolation on children in vulnerable families during COVID-19: a focus on children's reactions. Eur. Child Adolesc. Psychiatry. 2021;1:1–11. doi: 10.1007/S00787-021-01758-X/TABLES/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li K., Tang F., Hanna S., Bass D., Shair S., Dicerbo L., Giordani B., Kavcic V., Perez S., Nuccio A., Stripling A. The impact of COVID-19 concerns on the mental health of older adults: a rapid review. Innov. Aging. 2021;5:727–728. doi: 10.1093/GERONI/IGAB046.2691. [DOI] [Google Scholar]
- Lund C., Brooke-Sumner C., Baingana F., Baron E.C., Breuer E., Chandra P., Haushofer J., Herrman H., Jordans M., Kieling C., Medina-Mora M.E., Morgan E., Omigbodun O., Tol W., Patel V., Saxena S. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. 2018;5:357–369. doi: 10.1016/S2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- Ma L., Mazidi M., Li K., Li Y., Chen S., Kirwan R., Zhou H., Yan N., Rahman A., Wang W., Wang Y. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;293:78–89. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchi J., Johansson N., Sarkadi A., Warner G. The impact of the COVID-19 pandemic and societal infection control measures on children and adolescents’ mental health: a scoping review. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.711791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas K.R., He J.P., Burstein M., Swanson S.A., Avenevoli S., Cui L., Benjet C., Georgiades K., Swendsen J. Lifetime Prevalence of Mental Disorders in U.S. adolescents: results from the National comorbidity survey replication–adolescent supplement (NCS-A) J. Am. Acad. Child Adolesc. Psychiatry. 2010;49:980–989. doi: 10.1016/J.JAAC.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohd, W., Mohd, W., Wan, A., Yunus, M., Kauhanen, L., Sourander, A., Brown, J.S.L., Peltonen, K., Mishina, K., Lempinen, L., Bastola, K., Gilbert, S., 2022. Registered psychiatric service use, self ‑ harm and suicides of children and young people aged 0 –24 before and during the COVID ‑ 19 pandemic : a systematic review 3, 1–14. [DOI] [PMC free article] [PubMed]
- Nearchou F., Hennessy E., Flinn C., Niland R., Subramaniam S.S. Exploring the impact of covid-19 on mental health outcomes in children and adolescents: a systematic review. Int. J. Environ. Res. Public Health. 2020;17:1–19. doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen P.H., Kachwaha S., Pant A., Tran L.M., Walia M., Ghosh S., Sharma P.K., Escobar-Alegria J., Frongillo E.A., Menon P., Avula R. COVID-19 disrupted provision and utilization of health and nutrition services in uttar pradesh, india: insights from service providers, household phone surveys, and administrative data. J. Nutr. 2021;151:2305. doi: 10.1093/JN/NXAB135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Sullivan K., Clark S., McGrane A., Rock N., Burke L., Boyle N., Joksimovic N., Marshall K. A qualitative study of child and adolescent mental health during the COVID-19 pandemic in Ireland. Int. J. Environ. Res. Public Health. 2021;18:1062. doi: 10.3390/IJERPH18031062. 2021, Vol.Page 1062 18, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira J.M.D., Butini L., Pauletto P., Lehmkuhl K.M., Stefani C.M., Bolan M., Guerra E., Dick B., De Luca Canto G., Massignan C. Mental health effects prevalence in children and adolescents during the COVID-19 pandemic: a systematic review. Worldviews Evid. Based Nurs. 2022:1–8. doi: 10.1111/wvn.12566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/BMJ.N71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal U., Salazar de Pablo G., Franco M., Moreno C., Parellada M., Arango C., Fusar-Poli P. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur. Child Adolesc. Psychiatry. 2021 doi: 10.1007/s00787-021-01856-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda P.K., Gupta J., Chowdhury S.R., Kumar R., Meena A.K., Madaan P., Sharawat I.K., Gulati S. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J. Trop. Pediatr. 2021;67 doi: 10.1093/tropej/fmaa122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V. Mental health in low- and middle-income countries. Br. Med. Bull. 2007:81–82. doi: 10.1093/BMB/LDM010. 81–96. [DOI] [PubMed] [Google Scholar]
- Patel V., Flisher A.J., Nikapota A., Malhotra S. Promoting child and adolescent mental health in low and middle income countries. J. Child Psychol. Psychiatry. 2008;49:313–334. doi: 10.1111/J.1469-7610.2007.01824.X. [DOI] [PubMed] [Google Scholar]
- Polanczyk G.V., Salum G.A., Sugaya L.S., Caye A., Rohde L.A. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry. 2015;56:345–365. doi: 10.1111/JCPP.12381. [DOI] [PubMed] [Google Scholar]
- Preston A.J., Rew L. Connectedness, self-esteem, and prosocial behaviors protect adolescent mental health following social isolation: a systematic review. Issues Ment. Health Nurs. 2022;43:32–41. doi: 10.1080/01612840.2021.1948642. [DOI] [PubMed] [Google Scholar]
- Racine N., McArthur B.A., Cooke J.E., Eirich R., Zhu J., Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajmil L., Hjern A., Boran P., Gunnlaugsson G., Camargo O.K.de, Raman S. Original research: impact of lockdown and school closure on children's health and well-being during the first wave of COVID-19: a narrative review. BMJ Paediatr. Open. 2021;5 doi: 10.1136/BMJPO-2021-001043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren X., Huang W., Pan H., Huang T., Wang X., Ma Y. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 2020;91:1033–1045. doi: 10.1007/S11126-020-09796-5/FIGURES/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renov V., Risser L., Berger R., Hurley T., Villaveces A., DeGue S., Katz A., Henderson C., Premo K., Talis J., Chang J.C., Ragavan M. The impact of the COVID-19 pandemic on child protective services caseworkers and administrators. Child Abuse Negl. 2021 doi: 10.1016/J.CHIABU.2021.105431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. doi: 10.1016/J.JAD.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahebi A., Nejati-Zarnaqi B., Moayedi S., Yousefi K., Torres M., Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/J.PNPBP.2021.110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samji H., Wu J., Ladak A., Vossen C., Stewart E., Dove N., Long D., Snell G. Review: mental health impacts of the COVID-19 pandemic on children and youth – a systematic review. Child Adolesc. Ment. Health. 2021 doi: 10.1111/camh.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanja Đ., Ileana C.G., Vesna D., Ana Đ. Anxiety and depressive symptomatology among children and adolescents exposed to the COVID-19 pandemic - meta-analysis. Vojnosanit. Pregl. 2021:1–21. doi: 10.2298/VSP210521092D. [DOI] [Google Scholar]
- Sawyer M.G., Reece C.E., Sawyer A.C.P., Johnson S.E., Lawrence D. Has the prevalence of child and adolescent mental disorders in Australia changed between 1998 and 2013 to 2014? J. Am. Acad. Child Adolesc. Psychiatry. 2018;57:343–350. doi: 10.1016/J.JAAC.2018.02.012. e5. [DOI] [PubMed] [Google Scholar]
- Settersten R.A., Bernardi L., Härkönen J., Antonucci T.C., Dykstra P.A., Heckhausen J., Kuh D., Mayer K.U., Moen P., Mortimer J.T., Mulder C.H., Smeeding T.M., van der Lippe T., Hagestad G.O., Kohli M., Levy R., Schoon I., Thomson E. Understanding the effects of Covid-19 through a life course lens. Curr. Perspect. Aging Life Cycle. 2020;45 doi: 10.1016/J.ALCR.2020.100360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma M., Aggarwal S., Madaan P., Saini L., Bhutani M. Impact of COVID-19 pandemic on sleep in children and adolescents: a systematic review and meta-analysis. Sleep Med. 2021;84:259–267. doi: 10.1016/j.sleep.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva S.A., Silva S.U., Ronca D.B., Gonçalves V.S.S., Dutra E.S., Carvalho K.M.B. Common mental disorders prevalence in adolescents: a systematic review and meta-analyses. PLoS ONE. 2020;15 doi: 10.1371/JOURNAL.PONE.0232007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şimşir Z., Koç H., Seki T., Griffiths M.D. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. 2021;46:515–523. doi: 10.1080/07481187.2021.1889097. [DOI] [PubMed] [Google Scholar]
- Smitherman L.C., Golden W.C., Walton J.R. Health disparities and their effects on children and their caregivers during the coronavirus disease 2019 pandemic. Pediatr. Clin. North Am. 2021;68:1133. doi: 10.1016/J.PCL.2021.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spady D.W., Schopflocher D.P., Svenson L.W., Thompson A.H. Prevalence of mental disorders in children living in Alberta, Canada, as determined from physician billing data. Arch. Pediatr. Adolesc. Med. 2001;155:1153–1159. doi: 10.1001/ARCHPEDI.155.10.1153. [DOI] [PubMed] [Google Scholar]
- Tang S., Xiang M., Cheung T., Xiang Y.T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J. Affect. Disord. 2021;279:353–360. doi: 10.1016/J.JAD.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner R., Russell S., Saulle R., Croker H., Stansfield C., Packer J., Nicholls D., Goddings A.L., Bonell C., Hudson L., Hope S., Ward J., Schwalbe N., Morgan A., Minozzi S. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. 2022:1–10. doi: 10.1001/jamapediatrics.2021.5840. [DOI] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/J.JAD.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeasmin S., Banik R., Hossain S., Hossain M.N., Mahumud R., Salma N., Hossain M.M. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: a cross-sectional study. Child. Youth Serv. Rev. 2020;117 doi: 10.1016/J.CHILDYOUTH.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshikawa H., Aber J.L., Beardslee W.R. The effects of poverty on the mental, emotional, and behavioral health of children and youth. Am. Psychol. 2012;67:272–284. doi: 10.1037/A0028015. [DOI] [PubMed] [Google Scholar]
- Zemrani B., Gehri M., Masserey E., Knob C., Pellaton R. A hidden side of the COVID-19 pandemic in children: the double burden of undernutrition and overnutrition. Int. J. Equity Health. 2021;20 doi: 10.1186/S12939-021-01390-W. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.