Figure 2.
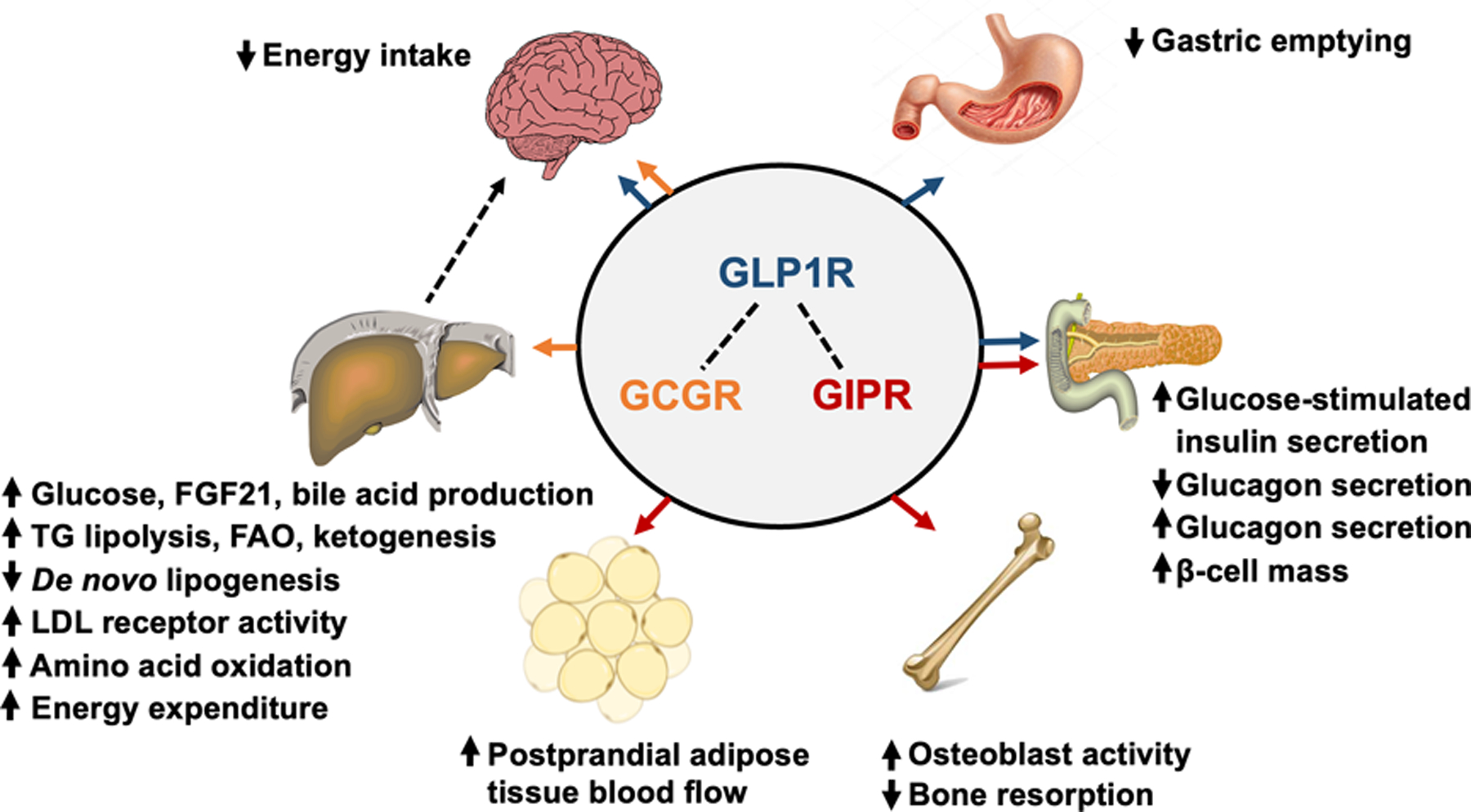
Multi-organ effects of GLP-1 (blue arrows), GIP (orange arrows), and glucagon (red arrows) receptor agonism. GLP1R agonists decrease energy intake through actions in the hypothalamus and brainstem, slow the rate of gastric emptying, enhance glucose-stimulated insulin secretion, inhibit glucagon secretion, and increase β-cell mass. GIPR agonists stimulate glucose-stimulated insulin secretion (however, the incretin effect of GIP is diminished or abolished in people with type 2 diabetes), stimulate glucagon secretion, increase β-cell mass, stimulate osteoblast activity while inhibiting bone resorption, and increase postprandial adipose tissue blood flow. GCGR agonists primarily act on the liver, and: i) increase glucose production by stimulating glycogenolysis and gluconeogenesis, ii) increase FGF21 production, iii) increase bile acid production, iv) decrease de novo lipogenesis, v) increase intrahepatic triglyceride lipolysis, fatty acid oxidation and ketogenesis, vi) increase amino acid oxidation, and vii) increase LDL receptor activity which decreases plasma LDL-C concentration. Although GCGR agonism increases energy expenditure in rodent models, short-term (72-hours) GCG infusion does not affect energy expenditure in people. GCGR agonism also decreases energy intake, and this effect requires the hepatic vagus nerve. Abbreviations: GLP-1, glucagon-like-peptide-1; GIP, glucose-dependent insulinotropic peptide; GLP1R, GLP-1 receptor; GIPR, GIP receptor; GCGR, glucagon receptor; FGF21, fibroblast growth factor-21; LDL, low-density lipoprotein; LDL-C, LDL cholesterol.
