Abstract
Background
Despite the advancements made in the management of the physical complications of open lower-limb fractures, few studies have been performed which investigate the association of such injuries with affective disorders. The complications resulting from this injury may result in significant psychological distress.
Aim
To evaluate the risk factors associated with the development of affective disorders, in patients with open lower-limb fractures.
Methods
A systematic review protocol was registered with PROSPERO and reported in accordance with the Preferred Reporting for Items for Systematic Reviews and Meta-Analyses. A comprehensive literature search was performed to gather relevant papers. Two independent reviewers screened titles and abstracts according to the inclusion and exclusion criteria.
Results
2488 were screened according to the inclusion and exclusion criteria resulting in seven articles eligible for inclusion. Of the seven articles, two assessed for PTSD, one assessed for depression and PTSD concurrently, two assessed for anxiety and depression concurrently, and two assessed for psychological distress. With the exception of two studies, open lower limb fracture patients were included with other lower-limb injuries in their analysis. Furthermore, not all variables were available in all included studies. Risk factors identified included post-operative pain, mechanism and severity of injury, age of patient, social support and social deprivation.
Conclusions
Further studies are required within this area. However, addressing risk factors such as pain management, poor social support and inappropriate coping mechanisms, may reduce the incidence of affective disorders by equipping patients with necessary psychosocial resources.
Keywords: Trauma, Open lower-limb fractures, Affective disorders, Depression, PTSD, Anxiety
Highlights
-
•
Patients with strong social support have, in general, a lower risk of depression and psychological distress.
-
•
Poverty is a risk factor in general for psychological distress.
-
•
Negative affect may play an important role in determining physical function during the recovery period.
-
•
In most patients, symptoms of psychological distress improve over time.
-
•
Not all patients may display symptoms of psychological distress immediately post-injury.
1. Introduction
Open lower-limb fractures are difficult injuries to treat, particularly in the presence of neurovascular damage and extensive soft-tissue loss [1,2]. The incidence rate of open long bone fractures is 11.5 per 100,000 person-years, of which the majority are open fractures of the tibia, with an estimated annual incidence of 3.4 per 100,00 [3,4]. Furthermore, these injuries most frequently occur in young adult males and elderly females. Previous studies estimate that roughly 50% of cases presenting are secondary to road traffic accidents or falls from a great height [[3], [4], [5]]. However, despite an improved understanding of managing the physical complications of open lower-limb fractures, few studies investigate the association of such injuries with subsequent affective disorders, such as anxiety, depression, and post-traumatic stress disorder (PTSD). These psychological disorders are known to correlate with disability following injury [6,7].
Psychological distress is a known complication following traumatic injury. A prospective analysis performed in 2010 demonstrated that the incidence of PTSD following severe lower-limb trauma was approximately 30% of their patient cohort [8]. A further study demonstrated similar results, with approximately a third of severely injured adults screening positive for a possible psychological disorder up to 2 years post-injury [9]. Additionally, patients who developed PTSD following trauma were found to have additional depressive symptoms within days of the injury [10].
This study aims to evaluate the risk factors associated with the development of affective disorders, in patients with open lower-limb fractures.
2. Methods
2.1. Search strategy and selection criteria
A systematic review protocol was registered with PROSPERO (CRD42021284854). This review is reported in accordance with the Preferred Reporting for Items for Systematic Reviews and Meta-Analyses (PRISMA) [11]. Comprehensive electronic search strategies were developed for each database using a combination of relevant keywords and index headings. A total of five bibliographic databases were searched (EMbase, MEDLINE, PsycInfo, CINAHL Plus and Cochrane Central Register of Controlled Trials). The search strategy was modified so that the index headings relevant to each specific database were selected. The search strategy was peer-reviewed by an information specialist. Forward and backward citation searches were conducted on articles identified as eligible for full text review. Full search strategies and results are contained in Supplement 1.
Duplicate papers were identified and removed in Endnote 20 before being uploaded to Rayyan for screening. Two independent reviewers screened titles and abstracts according to the inclusion and exclusion criteria (Table 1). The remaining articles were downloaded in full-text format and re-screened. Discussion with a senior author to achieve consensus resolved any conflicts between the two reviewers.
Table 1.
Inclusion & exclusion criteria of study.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Primary research paper investigating salvageable open lower limb fractures and anxiety/depression/PTSD | Systematic/narrative reviews, case reports, book chapters, abstracts, comments or notes |
| Any scoring system for anxiety/depression/PTSD | Animal studies |
| English language studies only | Non-English language papers |
| Studies unrelated to open lower limb fractures and anxiety/depression/PTSD |
2.2. Data extraction
The following information was extracted from full-text articles onto a customised Microsoft Excel spreadsheet: 1) Study characteristics, including author, year of publication, sample size, country, study design, study timeframe, and the assessment tools used; 2) Patient demographics; 3) Injury characteristics; and 4) Outcome data, including the prevalence and severity of affective disorders.
2.3. Synthesis
A meta-analysis was not considered for this review because of the wide variability of studies in relation to research design, study population, and affective disorders. However, a narrative synthesis was performed to synthesise the findings of the different studies. The results of the studies were discussed and structured into themes, depending on the identified risk factors of affective disorders. These risk factors formed the framework for our narrative synthesis. All articles that were included in this review were published before. The quality and risk of bias of the studies eligible for inclusion were evaluated using the Newcastle-Ottawa Scale (NOS) [12]. Studies with NOS scores 0–3, 4–6 and 7–8 were considered as low, moderate and high quality, respectively.
The methodological quality of this systematic review was evaluated by our team by utilising A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR-2) [13]. This tool is comprised of 16 items, with 7 critical items, and 9 non-critical items. For non-critical items, we assigned 1 point for 'Yes', 0.5 for ‘Partial Yes', and 0 for ‘No’. For critical items, the score was double. The total AMSTAR-2 score was 23 points [14,15]. This study was registered with the Research Registry, unique identifying number: reviewregistry1393 [16].
3. Results
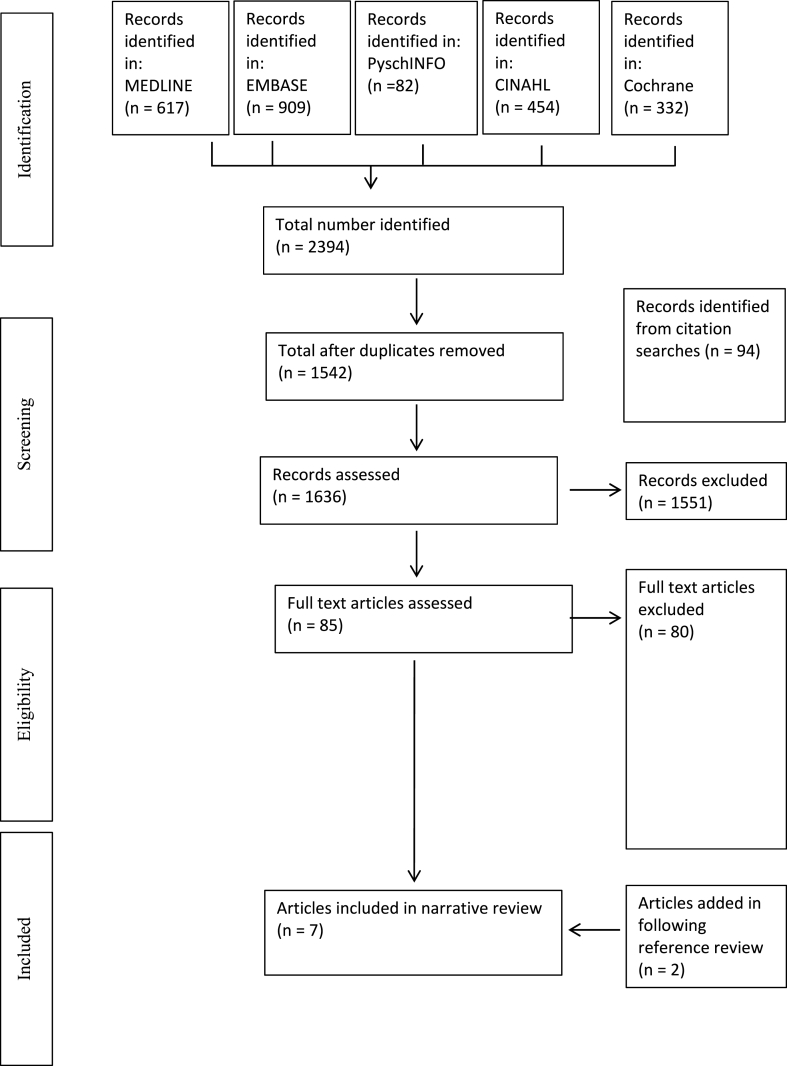
2394 published articles were identified following a comprehensive literature search. An additional 94 articles were added from citation searches. These articles were filtered for relevance and duplication, resulting in 85 articles. A full-text assessment was then performed, which reduced the number of articles to five. Further articles were identified through searching bibliographies, resulting in seven articles eligible for inclusion in this systematic narrative synthesis [8,9,[17], [18], [19], [20], [21]]. With regards to quality of evidence, all of the studies which were eligible for inclusion were considered to be of moderate quality. The AMSTAR-2 score for this systematic review was 11.5 points. Table 2 summarises the studies included in this study, and their NOS total scores. The PRISMA flow diagram is summarised in Fig. 1. .
Table 2.
Summary of studies included within systematic narrative synthesis, and their Newcastle-Ottawa Scale (NOS) total score.
| Study reference | Screening tool | Outcome measured | NOS |
|---|---|---|---|
| J. Messner 2020 | Child Revised Impact of Events Scale | PTSD | 5 |
| W. Bhat 2014 | The Posttraumatic Stress Disorder Checklist Scale |
PTSD | 6 |
| C. Doukas 2013 | The Revised Center for Epidemiologic Studies Depression Scale The military version of the PTSD Checklist |
Depression PTSD |
5 |
| A.Karladani 2001 | Beck Depression Inventory The State-Trait Anxiety Inventory |
Depression Anxiety |
6 |
| P. Ladlow 2016 | General Anxiety Disorder 7-item scale Patient Health Questionnaire |
Anxiety Depression |
5 |
| S. Wegener 2011 | Brief Symptom Inventory | Assesses the psychological symptom status (obsessive compulsive, anxiety, depression) | 5 |
| McCarthy 2003 | Brief Symptom Inventory | Assesses the psychological symptom status (obsessive compulsive, anxiety, depression) | 5 |
Fig. 1.
Prisma flow diagram.
3.1. Pain and psychological wellbeing implications on physical function
Wegener et al. demonstrated higher levels of psychological distress in comparison to population norms in their patient cohort (P < 0.05 to 0.01) [22]. They also reported that negative affect played an important role in determining physical function. Decreased levels of function were exhibited at 6-, 12- and 24-month time points in patients with negative emotions. Their study also demonstrated that higher pain levels resulted in lower levels of functioning at the 6- and 12-month time points although not at the 24-month time point. Their team concluded that negative affect mediated the impact of pain on physical function. They theorised that pain influenced function through the negative affect which accompanies it. This reduced the relationship between pain and function over time, and as the recovery process proceeded, physical function became mostly influenced by negative emotions, thus explaining why pain primarily impacted function early on in recovery. Table 3 demonstrates negative affect outcomes in this patient cohort.
Table 3.
Negative affect outcomes in this patient cohort [11].
| Brief symptom inventory (0–1) | Reference data | 3 months | 6 months | 12 months | 24 months |
|---|---|---|---|---|---|
| Anxiety score | 0.35 | 0.61** | 0.52** | 0.49* | 0.54** |
| Obsessive-compulsive score | 0.43 | 0.63** | 0.64** | 0.65** | 0.76** |
| Depression score | 0.28 | 0.64** | 0.55** | 0.52** | 0.62** |
| Interpersonal sensitivity score | 0.32 | 0.49* | 0.45* | 0.49* | 0.55** |
*p < 0.05 when compared to reference data by Student's t-test.
**p < 0.01 when compared to reference data by Student's t-test.
3.2. Mechanism and severity of injury, and psychological wellbeing
Messner et al. investigated the incidence of psychological trauma in a cohort of 32 patients with open lower-limb fractures [19]. Scores for psychological assessment were only available for 21 patients at their most recent follow-up, of which 8 patients were at high risk of experiencing symptoms of PTSD [23]. No association was identified between the severity of the injury and worse scores on psychological assessment. McCarthy et al. similarly found that injury severity was not found to be associated with psychological distress following musculoskeletal injury. Table 4 summarises the factors that were found to be associated with screening positive for a likely psychological disorder in the longitudinal, multivariate logistic regression analysis.
Table 4.
Longitudinal Logistic Regression Results of Modeling Screening Positive for a Psychological Disorder (the adjusted odds ratios represent the increase in the odds of screening positive) [7].
| Predictor | Odds ratio (95% confidence interval) for likely psychological disorder |
|---|---|
| Age | |
| 15–24 years (vs ≥ 55years) | 5.61 (2.76–11.39) |
| 25–54 years (vs ≥ 55years) | 6.11 (3.13–11.91) |
| Low-to-medium social support (vs high) | 1.86 (1.36–2.54) |
| Non-Caucasian (vs Caucasian) | 1.55 (1.11–2.16) |
| Low-to-medium self-efficacy (vs high) | 1.46 (1.08–1.97) |
| Poverty status | |
| Near-poor (vs. non-poor) | 1.34 (0.90–2.01) |
| Poor (vs. non-poor) | 1.44 (1.03–2.01) |
| High neuroticism (vs. low-to-average) | 1.38 (1.02–1.87) |
| Likely drinking problem (vs no or possible) | 1.36 (0.99–1.88) |
Bhat et al. utilised the Posttraumatic Stress Disorder Checklist Scale (PCL-S). A score of 30 or above is considered to be PTSD positive. Nineteen patients rated their PCL-S scores >30, of which 12 patients were younger than 50 years old, and 7 patients older than 50 years old. Their study demonstrated that younger patients had higher PCL-S scores when compared to older patients [8]. They thought this may have been a surrogate for the mechanism of injury as these patients tended to have sustained their injury from higher velocity mechanisms when compared to older patients.
3.3. Age and psychological wellbeing
Bhat et al. demonstrated that patients >50 years old had statistically lower PCL-S scores than younger patients at the 2-month follow-up (p = 0.013). Additionally, the <25-year-old age group scored significantly higher PCL-S scores than the older age groups. Results were significantly lower at the 4-month follow-up regardless of age (p = 0.021). Age of the patient was negatively correlated with PCL-S scores (−0.277). Table 5 summarises PCL-S scores of this patient cohort depending on age.
Table 5.
| Score <30 | Score >30 | |
|---|---|---|
| <50 years old | 15 | 12 |
| >50 years old | 26 | 7 |
| Total | 41 | 19 |
Similarly, McCarthy et al. found that patients between the ages of 15 and 54 were five to six times more likely to screen positive for a psychological disorder than patients older than 55 years of age following a lower-limb threatening injury [9].
3.4. Psychological well-being over time following injury
Symptoms of psychological distress may persist over time, as demonstrated in the study by McCarthy et al., where psychological distress symptoms persisted throughout the 24-month follow-up period [9]. However, Bhat et al. demonstrated that PCL-S scores improved over time. Results were significantly lower at the 4-month follow-up, in comparison to the 2-month follow-up, regardless of age (p = 0.021). Similarly, Wegener et al. noted improvements in psychological distress over time in patients with lower-limb injuries [17].
3.5. Ethnicity, social deprivation and psychological distress
McCarthy et al. demonstrated that race and poverty were associated with psychological distress [9]. They found that non-Caucasian patients were more likely to experience psychological distress in their study. However, when this patient cohort was further examined, they found that they were more likely to lack health insurance and were also less likely to have completed high school when compared with Caucasian patients. Therefore, the race of the patient may have only acted as a surrogate for reduced access to medical and educational resources for this patient cohort.
3.6. Social support and psychological wellbeing
Doukas et al. investigated the incidence of depression and PTSD in a cohort of 324 service members deployed to Afghanistan or Iraq. Of 324 patients in the study, 142 patients had limb salvage without amputation (126 unilateral and 16 bilateral salvage). They found that the strength of social support was a strong correlate of both physical and psychosocial functioning (p < 0.01) [20]. With regards to the unilateral limb salvage group, Table 6 summarises the demographic details. Unfortunately, the demographics for bilateral lower-limb salvage were not available. Table 6 also summarises the interpretation of the social support scores for this patient cohort, alongside the age of participants, educational level, and marital status. Table 7, Table 8 summarise the outcomes relevant to this review.
Table 6.
Mental health outcomes for the limb salvage groups [15].
| Mental health outcome | Limb salvage |
|---|---|
| PHQ-9* | 3± 5 (0–17) |
| <5 (% of patients) | 76 |
| >10 (% of patients) | 14 |
| >15 (% of patients) | 5 |
| GAD-7* | 3± 4 (0–16) |
| <5 (% of patients) | 71 |
| >10 (% of patients) | 5 |
| >15 (% of patients) | 5 |
* Mean & standard deviation, with range in parenthesis.
Table 7.
Demographic information of patient cohort [14].
| All participants (N = 324) | Unilateral lower-limb salvage (N = 126) | |
|---|---|---|
| Mean time to interview (months) | 37.5 | 39.5 |
| Age (%) | ||
| 18–24 years | 24.2 | 24 |
| 25–29 years | 36.2 | 35.2 |
| ≥30 years | 39.6 | 40.8 |
| Male (%) | 97.2 | 97 |
| Educational level | ||
| High school or less (%) | 36.1 | 41.3 |
| Marital status (%) | ||
| Married | 57.7 | 54.8 |
| Never married | 28.7 | 30.9 |
| Separated/divorced/widowed | 13.6 | 14.3 |
| Social support (%) | ||
| Low (0−70) | 26.8 | 31.8 |
| Moderate (71–80) | 35.8 | 34.9 |
| High (81–100) | 37.4 | 33.3 |
Table 8.
The incidence of depression, PTSD and pain which interfered with daily activity in unilateral and bilateral lower-limb salvage patient cohort [14].
| All patients | Unilateral lower-limb salvage | Bilateral lower-limb salvage | |
|---|---|---|---|
| Number of participants | 324 | 126 | 16 |
| Presence of depressive symptoms (%) | 38.3 | 43.6 | 37.5 |
| Possible major depression (%) | 13 | 15.1 | 12.5 |
| Screened positive for PTSD (%) | 17.9 | 26.8 | 12.5 |
| Pain interfering with daily activity (%) | 19.9 | 27 | 12.5 |
McCarthy et al. also found that the lack of social support was strongly related to screening positive for psychological disorders [9]. Similarly, Bhat et al. also found a positive correlation between high PCL-S scores and lack of social support [8].
4. Discussion
Despite our improved understanding in the management of open lower-limb fractures, limited research has been performed on the likely psychological distress that may arise from the injury.
The persistence of pain and psychological distress may negatively impact physical function. Studies have demonstrated that both psychological distress and pain prospectively predict levels of physical function; and that reduced physical function may predict increased levels of pain and psychological distress, creating a worsening cycle [[24], [25], [26], [27]]. Wegener et al. demonstrated that negative affect played an important role in determining physical function over time [17]. Their findings were similar to Katz et al., who found that pain intensity was de-coupled from function as time progressed, whilst the relationship between negative affect and disability was strengthened [28]. However, it is important to note that pain is likely a subjective experience, consisting of various dimensions [29]. For example, pain has been described to have both a sensory dimension and an affective dimension. The sensory dimension correlating to the intensity of the pain, and the affective dimension correlating to the unpleasant feeling attributed to the pain [30]. Wegener et al. measured pain using the single-item pain intensity visual analog scale, which may not have been able to capture all the dimensions of pain [31].
Similar to other studies, Messner et al. and McCarthy et al. did not find an association between injury severity and psychological distress symptoms [[32], [33], [34]]. However, their strict exclusion criteria produced a homogenous study sample in terms of overall injury and lower-limb injury severity, resulting in little variability. Consequently, it was not surprising to find that injury severity was not associated with psychological distress outcomes. If injuries such as Gustilo-Anderson type 1 and 2 were included in their study, an association between severity of injury and psychological distress may have been observed.
In recent decades, the rates of depression and suicidal behaviours have steadily increased among young people [35]. The peak age of onset of psychological disorders is during adolescence and early adulthood [36]. This may explain why younger patients were more likely to screen positive for a psychological disorder [8,9]. However, the mechanism of injury may provide an alternative reason for this. Bhat et al. found that younger patients were more likely to have sustained their injury through higher velocity mechanisms. These injuries understandably may result in a lengthier hospital stay, and require complex surgical procedures.
The paucity of longitudinal data did not allow for an in-depth analysis of the incidence of psychological symptoms over time. However, similar to other studies, Bhat et al. and Wegner et al. demonstrated that the severity of psychological distress would be worse initially, but would improve over time [8,17,37]. It is, however, worth noting that not all patients may display symptoms of psychological distress immediately post-injury. In delayed-onset PTSD, patients may initially have subthreshold symptoms after the traumatic event and will not meet the criteria for the diagnosis of PTSD until at least six months following the event [38].
Studies included in this review were not able to demonstrate the effects of pre-existing psychiatric illness on the incidence and recovery from post-injury distress. Premorbid psychiatric history and family history of psychiatric illness have been reported in the literature to be associated with prolonged recovery and poor psychiatric and clinical outcomes post-injury [[39], [40], [41], [42]]. Positive effects on recovery from trauma have already been observed in patients with head injuries and critical illness, following the appropriate management of their co-morbid psychological illness [43,44]. Therefore, the appropriate management of the co-morbid psychological illnesses of patients presenting with open lower-limb fractures may result in improved recovery from trauma.
Patients with strong social support have, in general, a lower risk of depression and psychological distress [45]. Horgan and MacLachlan suggested that higher levels of active coping and increased levels of social support contribute to better mental health outcomes post-injury in patients with lower-limb amputations [46]. Bhat et al., Doukas et al., and McCarthy et al. all demonstrated that a lack of social support was a risk factor for psychological disorders [8,9,20]. Furthermore, McCarthy et al. demonstrated that poverty was a risk factor in general for psychological distress, which reaffirmed the findings of other studies [[47], [48], [49]].
5. Limitations
With the exception of two studies, open lower limb fracture patients were included with other lower-limb injuries in their analysis. The heterogeneous nature of the injuries reduced the generalisability of our results. Additionally, variables, such as severity of injury, education level, gender, race, social support, length of hospital stay, complications, and requirement for further surgical management were not available in all included studies. These factors have been demonstrated to influence post-operative recovery and the incidence of psychological disorders [9,20].
The majority of the studies included were retrospective in nature, therefore introducing a degree of observer bias. Furthermore, the time points of the psychological assessment were inconsistent between the studies. This did not allow for an accurate conclusion to be drawn regarding the incidence, progression, and recovery of psychological disorders over time.
The presence of psychological disorders prior to injury may limit the interpretation of study results. Without screening for pre-injury psychiatric disorders, the clinician will not be able to determine how much of this psychological distress was present prior to the injury and how much of it was caused by the injury itself.
6. Conclusion
Further studies are required to reach a valid conclusion within this area. The complexity of open lower-limb fractures necessitates that a multidisciplinary team manage this patient cohort from the outset. In addition to their medical and surgical needs, their psychological needs will need to be addressed in order to deliver holistic care. Baseline assessment of psychological health on admission will allow the clinician to monitor for change over time and plan appropriate treatment. This can be achieved either through standardised assessment tools, or through clinical evaluation by a mental health professional. Additionally, addressing risk factors such as pain management, poor social support and inappropriate coping mechanisms, may reduce the incidence of affective disorders by equipping patients with the necessary psychosocial resources to cope with the trauma and facilitate a successful recovery.
Ethical approval
No ethical approval was required for this project.
Sources of funding
We did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Munir Abukhder: Design of study, Screening papers, Data collection, Data analysis, Writing the paper, Thomas Dobbs, Design of study, Editing paper, Supervisor, Jessie Shaw, Screening papers, Data collection, Data analysis, Editing paper, Rhys Whelan, Development of search strategies, Emma Jones, Search strategy peer review.
Registration of research studies
The systematic review protocol was registered with PROSPERO (CRD42021284854).
Guarantor
Munir Abukhder.
Consent
Not required.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
We did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This research was undertaken as partial fulfilment of the requirements for the MSc Surgical Sciences at The University of Edinburgh.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104190.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Gustilo R.B., Anderson J.T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J. Bone Joint Surg. Am. 1976;58:453–458. [PubMed] [Google Scholar]
- 2.Eccles S., Handley B., Khan U., Nanchahal J., Nayagam S., McFadyen I., editors. Standards for the Management of Open Fractures. Oxford University Press; 2020. [DOI] [Google Scholar]
- 3.Larsen P., Elsoe R., Hansen S.H., Graven-Nielsen T., Laessoe U., Rasmussen S. Incidence and epidemiology of tibial shaft fractures. Injury. 2015;46:746–750. doi: 10.1016/j.injury.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 4.Court-Brown C.M., Rimmer S., Prakash U., McQueen M.M. The epidemiology of open long bone fractures. Injury. 1998;29:529–534. doi: 10.1016/S0020-1383(98)00125-9. [DOI] [PubMed] [Google Scholar]
- 5.Jenkins P.J., Keating J.F., Simpson A.H. Fractures of the tibial shaft. Surgery. 2010;28:489–493. doi: 10.1016/j.mpsur.2010.07.006. [DOI] [Google Scholar]
- 6.Crichlow R.J., Andres P.L., Morrison S.M., Haley S.M., Vrahas M.S. Depression in orthopaedic trauma patients. Prevalence and severity. J. Bone Joint Surg. Am. 2006;88 doi: 10.2106/JBJS.D.02604. 1927–33. [DOI] [PubMed] [Google Scholar]
- 7.Vranceanu A.-M., Bachoura A., Weening A., Vrahas M., Smith R.M., Ring D. Psychological factors predict disability and pain intensity after skeletal trauma. J. Bone Joint Surg. Am. 2014;96:e20. doi: 10.2106/JBJS.L.00479. [DOI] [PubMed] [Google Scholar]
- 8.Bhat W., Marlino S., Teoh V., Khan S., Khan U. Lower limb trauma and posttraumatic stress disorder: a single UK trauma unit's experience. J. Plast. Reconstr. Aesthetic Surg. 2014;67:555–560. doi: 10.1016/j.bjps.2013.12.039. Churchill Livingstone. [DOI] [PubMed] [Google Scholar]
- 9.Mccarthy M.L., Mackenzie E.J., Edwin D., Bosse M.J., Castillo R.C., Starr A. Psychological distress associated with severe lower-limb injury. J. Bone Joint Surg. Am. 2003;85:1689–1697. doi: 10.2106/00004623-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Nyberg E., Stieglitz R.D., Frommberger U., Berger M. [Psychological disorders after severe occupational accidents] Versicherungsmedizin. 2003;55:76–81. [PubMed] [Google Scholar]
- 11.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J., Akl E., Brennan S., Chou R., Glanville J., Grimshaw J., Hróbjartsson A., Lalu M., Li T., Loder E., Mayo-Wilson E., McDonald S., McGuinness L., Stewart L., Thomas J., Tricco A., Welch V., Whiting P., Moher D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst. Rev. 2021;10(1):89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells G., Shea B., O'Connell D., Peterson J., Welch V., Losos M., et al. 2013. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses.http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Google Scholar]
- 13.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng Q., Lai F., Li B., Xu J., Long J., Peng S., et al. Association between prospective registration and quality of systematic reviews in type 2 diabetes mellitus: a meta-epidemiological study. Front. Med. 2021;8 doi: 10.3389/fmed.2021.639652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suls J., Mogavero J.N., Falzon L., Pescatello L.S., Hennessy E.A., Davidson K.W. Health behaviour change in cardiovascular disease prevention and management: meta-review of behaviour change techniques to affect self-regulation. Health Psychol. Rev. 2020;14:43–65. doi: 10.1080/17437199.2019.1691622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Review Registry Unique Identifying Number. 2022. https://www.researchregistry.com/browse-the-registry#registryofsystematicreviewsmeta-analyses/registryofsystematicreviewsmeta-analysesdetails/62c5e0126908bb001e766f81/ [Google Scholar]
- 17.Wegener S.T., Castillo R.C., Haythornthwaite J., MacKenzie E.J., Bosse M.J. Psychological distress mediates the effect of pain on function. Pain. 2011;152:1349–1357. doi: 10.1016/j.pain.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 18.Karladani A.H., Granhed H., Fogdestam I., Styf J. 2001. Salvaged Limbs after Tibial Shaft Fractures with Extensive Soft-Tissue Injury: A Biopsychosocial Function Analysis. [DOI] [PubMed] [Google Scholar]
- 19.Messner J., Harwood P., Johnson L., Itte V., Bourke G., Foster P. Lower limb paediatric trauma with bone and soft tissue loss: ortho-plastic management and outcome in a major trauma centre. Injury. 2020;51:1576–1583. doi: 10.1016/j.injury.2020.03.059. [DOI] [PubMed] [Google Scholar]
- 20.Doukas C., Ret) W.C., Hayda C., Ret) R.A., Frisch H.M., Andersen C.R.C., Mazurek C.M.T., Ficke C.J.R., et al. The military extremity trauma amputation/limb salvage (METALS) study. J. Bone Joint Surg. Am. 2013;95:138–145. doi: 10.2106/JBJS.K.00734. [DOI] [PubMed] [Google Scholar]
- 21.Ladlow P., Phillip R., Coppack R., Etherington J., Bilzon J., McGuigan M.P., et al. Influence of immediate and delayed lower-limb amputation compared with lower-limb salvage on functional and mental health outcomes post-rehabilitation in the U.K. Military. J. Bone Joint Surg. 2016;98 doi: 10.2106/JBJS.15.01210. 1996–2005. [DOI] [PubMed] [Google Scholar]
- 22.Derogatis L.R. National Computer Systems; Minneapolis: MN: 1993. BSI: Brief Symptom Inventory. [Google Scholar]
- 23.Perrin S., Meiser-Stedman R., Smith P. The children's revised impact of event scale (CRIES): validity as a screening instrument for PTSD. Behav. Cognit. Psychother. 2005;33:487–498. doi: 10.1017/S1352465805002419. [DOI] [Google Scholar]
- 24.Dionne C.E., Koepsell T.D., von Korff M., Deyo R.A., Barlow W.E., Checkoway H. Predicting long-term functional limitations among back pain patients in primary care settings. J. Clin. Epidemiol. 1997;50:31–43. doi: 10.1016/s0895-4356(96)00313-7. [DOI] [PubMed] [Google Scholar]
- 25.Leveille S.G., Guralnik J.M., Ferrucci L., Hirsch R., Simonsick E., Hochberg M.C. Foot pain and disability in older women. Am. J. Epidemiol. 1998;148:657–665. doi: 10.1093/aje/148.7.657. [DOI] [PubMed] [Google Scholar]
- 26.Covic T., Adamson B., Spencer D., Howe G. A biopsychosocial model of pain and depression in rheumatoid arthritis: a 12-month longitudinal study. Rheumatology. 2003;42:1287–1294. doi: 10.1093/rheumatology/keg369. [DOI] [PubMed] [Google Scholar]
- 27.Smedstad L.M., Vaglum P., Moum T., Kvien T.K. The relationship between psychological distress and traditional clinical variables: a 2 year prospective study of 216 patients with early rheumatoid arthritis. Br. J. Rheumatol. 1997;36:1304–1311. doi: 10.1093/rheumatology/36.12.1304. [DOI] [PubMed] [Google Scholar]
- 28.Katz J., Asmundson G.J.G., McRae K., Halket E. Emotional numbing and pain intensity predict the development of pain disability up to one year after lateral thoracotomy. Eur. J. Pain. 2009;13:870–878. doi: 10.1016/j.ejpain.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Malhotra A., Mackey S. Outcomes in pain medicine: a brief review. Pain Ther. 2012;1:5. doi: 10.1007/s40122-012-0005-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Talbot K., Madden V.J., Jones S.L., Moseley G.L. The sensory and affective components of pain: are they differentially modifiable dimensions or inseparable aspects of a unitary experience? A systematic review. Br. J. Anaesth. 2019;123:e263–e272. doi: 10.1016/j.bja.2019.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dworkin R.H., Turk D.C., Farrar J.T., Haythornthwaite J.A., Jensen M.P., Katz N.P., et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 32.Martin-Herz S.P., Zatzick D.F., McMahon R.J. Health-related quality of life in children and adolescents following traumatic injury: a review. Clin. Child Fam. Psychol. Rev. 2012;15:192–214. doi: 10.1007/s10567-012-0115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Winthrop A.L. Health-related quality of life after pediatric trauma. Curr. Opin. Pediatr. 2010;22:346–351. doi: 10.1097/MOP.0b013e3283394351. [DOI] [PubMed] [Google Scholar]
- 34.Holbrook T.L., Anderson J.P., Sieber W.J., Browner D., Hoyt D.B. Outcome after major trauma. J. Trauma Inj. Infect. Crit. Care. 1999;46:765–773. doi: 10.1097/00005373-199905000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Newport: ONS . 2014. Measuring National Well-Being - Exploring the Well-Being of Children in the UK.https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/measuringnationalwellbeing/2014-10-08 [Google Scholar]
- 36.Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatr. 2005;62:593. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 37.Kellezi B., Coupland C., Morriss R., Beckett K., Joseph S., Barnes J., et al. The impact of psychological factors on recovery from injury: a multicentre cohort study. Soc. Psychiatr. Psychiatr. Epidemiol. 2017;52:855–866. doi: 10.1007/s00127-016-1299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smid G.E., Mooren T.T.M., van der Mast R.C., Gersons B.P.R., Kleber R.J. Delayed posttraumatic stress disorder. J. Clin. Psychiatr. 2009;70:1572–1582. doi: 10.4088/JCP.08r04484. [DOI] [PubMed] [Google Scholar]
- 39.Zemek R., Barrowman N., Freedman S.B., Gravel J., Gagnon I., McGahern C., et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315:1014. doi: 10.1001/jama.2016.1203. [DOI] [PubMed] [Google Scholar]
- 40.Ellis M.J., Ritchie L.J., Koltek M., Hosain S., Cordingley D., Chu S., et al. Psychiatric outcomes after pediatric sports-related concussion. J. Neurosurg. Pediatr. 2015;16:709–718. doi: 10.3171/2015.5.PEDS15220. [DOI] [PubMed] [Google Scholar]
- 41.Vargas G., Rabinowitz A., Meyer J., Arnett P.A. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J. Athl. Train. 2015;50:250–255. doi: 10.4085/1062-6050-50.3.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morgan C.D., Zuckerman S.L., Lee Y.M., King L., Beaird S., Sills A.K., et al. Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J. Neurosurg. Pediatr. 2015;15:589–598. doi: 10.3171/2014.10.PEDS14356. [DOI] [PubMed] [Google Scholar]
- 43.Albert S.M., Im A., Brenner L., Smith M., Waxman R. Effect of a social work liaison program on family caregivers to people with brain injury. J. Head Trauma Rehabil. 2002;17:175–189. doi: 10.1097/00001199-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Delva D., Vanoost S., Bijttebier P., Lauwers P., Wilmer A. Needs and feelings of anxiety of relatives of patients hospitalized in intensive care units. Soc. Work. Health Care. 2002;35:21–40. doi: 10.1300/J010v35n04_02. [DOI] [PubMed] [Google Scholar]
- 45.Taylor S.E., Seeman T.E. Psychosocial resources and the SES-health relationship. Ann. N. Y. Acad. Sci. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- 46.Horgan O., MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disabil. Rehabil. 2004;26:837–850. doi: 10.1080/09638280410001708869. [DOI] [PubMed] [Google Scholar]
- 47.Backlund E., Sorlie P.D., Johnson N.J. A comparison of the relationships of education and income with mortality: the national longitudinal mortality study. Soc. Sci. Med. 1999;49:1373–1384. doi: 10.1016/S0277-9536(99)00209-9. [DOI] [PubMed] [Google Scholar]
- 48.Adler N.E., Ostrove J.M. Socioeconomic status and health: what we know and what we don't. Ann. N. Y. Acad. Sci. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- 49.Marmot M., Ryff C.D., Bumpass L.L., Shipley M., Marks N.F. Social inequalities in health: next questions and converging evidence. Soc. Sci. Med. 1997;44:901–910. doi: 10.1016/S0277-9536(96)00194-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.