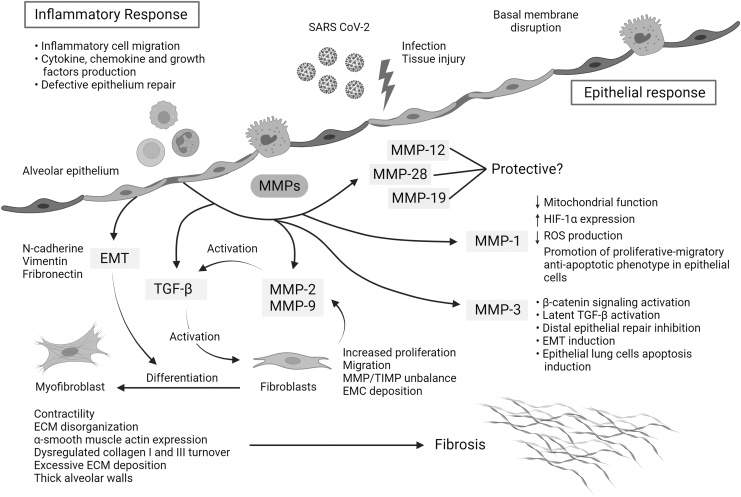
FIG. 2.
Mechanisms of action of MMPs and TGF-β that link hyperinflammation and pulmonary fibrosis in severe COVID-19. The replication rate of SARS-CoV-2 and associated lung epithelial cell death may trigger a cytokine storm, hyperinflammation, and epithelial dysfunction. During severe COVID-19, the initial acute inflammatory response might be followed by epithelial cell hyperplasia, where key mediators such as MMPs drive epithelial and endothelial injury and uncontrolled fibroblast proliferation. Moreover, some MMPs can activate other profibrotic mediators such as TGF-β, which also contributes to fibroblast accumulation, differentiation to myofibroblasts, ECM disorganization, dysregulated collagen I and III turnover, excessive ECM deposition, and thick alveolar walls. MMPs can also be involved in the regulation of other pathways, such as MMP-1, implicated in the reduction of mitochondrial function, the reduction of reactive oxygen species, and the overexpression of HIF-1α, and MMP3 in latent TGF-β activation, β-catenin signaling activation, and lung epithelial cell apoptosis, among others. The art pieces used in this figure were modified from Servier Medical Art by Servier and Biorender, licensed under a Creative Commons Attribution 3.0 Unported License.