Figure 1.
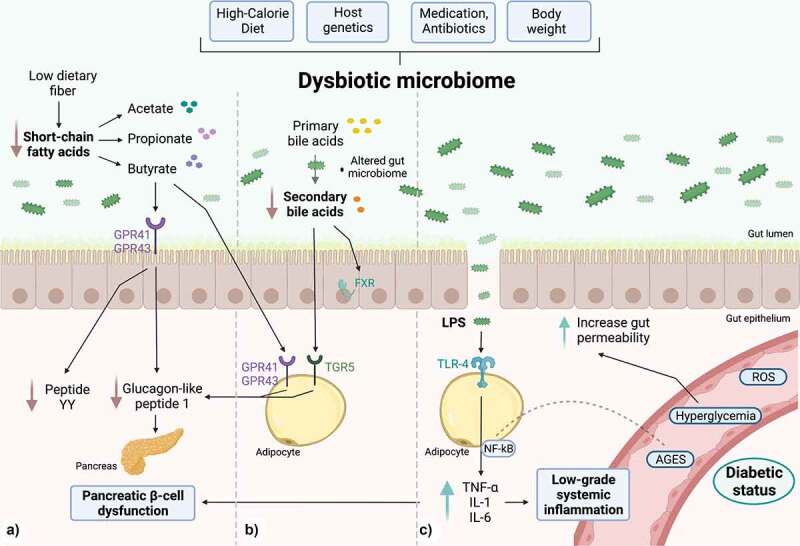
Gut microbiome-derived mechanisms are able to modulate the chronic inflammatory state in DT2. a) SCFAs, products of dietary fiber fermentation, promote GLP-1 and YY peptide secretion in L cells by activating G protein-coupled receptors such as GPR41 and GPR43. With a dysbiotic microbiome, there is an overall decline in the production of SCFAs, leading to a reduction in GLP-1 secretion, impairing pancreatic insulin secretion. b) Secondary bile acids derived from the intestinal microbiome act as mediator molecules through nuclear receptors such as the FXR receptor and the TGR5 membrane receptor, which in intestinal L cells improve glucose metabolism by stimulating GLP-1 production and promoting insulin secretion. Also, in muscle (not shown), they enhance mitochondrial activity and facilitate insulin sensitization. c) PAMPs, e.g., LPS can bind to the TLR4 receptor, and stimulate the expression of pro-inflammatory cytokines IL-6, IL-1 and TNF-α, which are characteristic of a low-grade systemic inflammatory state. There is an increase in intestinal permeability due to the direct effects of glucotoxicity and gut dysbiosis. Created with BioRender.com.
