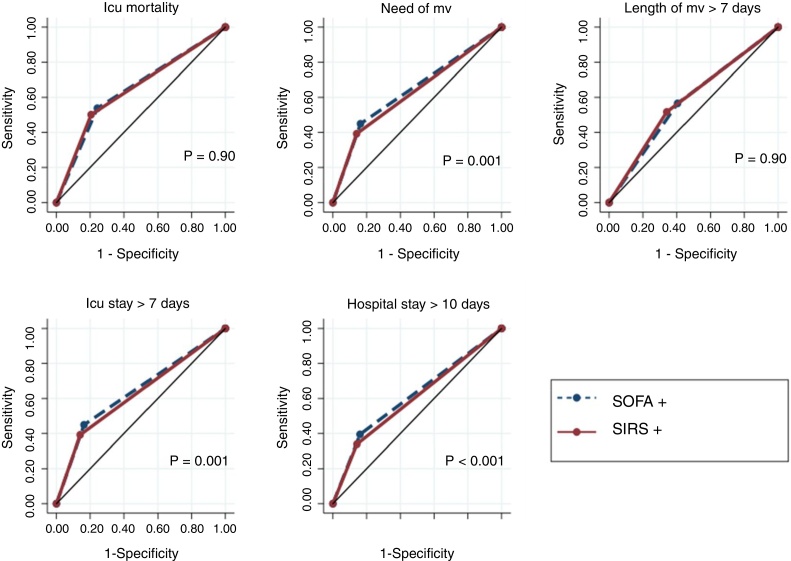
Fig. 1.
Comparison of predictive accuracy for outcomes among SOFA and SIRS criteria defining sepsis in 1487 critical care patients with infection at ICU admission. Abbreviations: AUROC, area under receiver operating characteristic curve; CI, confidence interval; ICU, intensive care unit; MV, mechanical ventilation.
Note: SOFA+, patients with SOFA variation ≥2 over their baseline clinical scores. SIRS+, patients with at least 2 of the following signs of SIRS: temperature > 38 °C or <36 °C, heart rate > 90 beats per minute, respiratory rate > 20 breaths per minute or PaCO2 < 32 mmHg, abnormal white blood cell count (>12,000/μL or <4000/μL or >10% immature forms).
ICU mortality: SOFA + AUROC 0.64 (95% CI, 0.62–0.67); SIRS + AUROC 0.64 (95% CI, 0.62–0.67). Need for MV: SOFA + AUROC 0.64 (95% CI, 0.62–0.65); SIRS + AUROC 0.62 (95% CI, 0.61–0.63). Length of MV >7 days: SOFA + AUROC 0.57 (95% CI, 0.55–0.60); SIRS + AUROC 0.58 (95% CI, 0.56–0.61). ICU stay >7 days: SOFA + AUROC 0.64 (95% CI, 0.62–0.65); SIRS + AUROC 0.62 [95% CI, 0.61–0.63). Hospital stay >10 days: SOFA + AUROC 0.61 (95% CI, 0.60–0.63); SIRS + AUROC 0.59 (95% CI, 0.58–0.61).