Abstract
After-action review uses experiences gained from past events to adopt best practices, thereby improving future interventions. In December 2016 and late 2018, the government of Tanzania with support from partners responded to anthrax and rabies outbreaks in Arusha and Morogoro regions respectively. The One Health Coordination Desk (OHCD) of the Prime Minister’s Office (PMO) later coordinated after-action reviews to review the multi-sectoral preparedness and response to the outbreaks. To establish and describe actions undertaken by the multi-sectoral investigation and response teams during planning and deployment, execution of field activities, and outbreak investigation and response, system best practices and deficiencies. These were cross-sectional surveys. Semi-structured, open and closed-ended questionnaire and focus group discussions were administered to collect information from responders at the national and subnational levels. It was found that the surveillance and response systems were weak at community level, lack of enforcement of public health laws including vaccination of livestock and domestic animals and joint preparedness efforts were generally undermined by differential disease surveillance capacities among sectors. Lack of resources in particular funds for supplies, transport and deployment of response teams contributed to many shortfalls. The findings underpin the importance of after-action reviews in identifying critical areas for improvement in multi-sectoral prevention and control of disease outbreaks. Main sectors under the coordination of the OHCD should include after action reviews in their plans and budget it as a tool to continuously assess and improve multi-sectoral preparedness and response to public health emergencies.
Key words: Outbreaks, response, after-action review
Introduction
The Republic of Tanzania has made huge steps in strengthening the International Health Regulation 2005 (IHR- 2005) core capacities and fulfilling the requirements of the Global Health Security Agenda (GHSA). The National One Health Strategic Plan (NOHSP) 2015-2020 was prepared in 2015 and its implementation started in 2016.1 The National One Health Platform for Tanzania, called the One Health Coordination Desk (OHCD) and positioned in the Prime Minister’s Office (PMO), was created in 2016 to coordinate all One Health-related activities in Tanzania. The national One Health platform’s core structure encompasses appointed staff from human, animal and environment sectors. Other public sectors such as agriculture, finance a diversity of regulatory authorities, research and academic institutions, UN agencies and NGOs are also part of the platform.1
The Joint External Evaluation (JEE) was conducted in Tanzania in 2016, which resulted in the development and launch of the National Action Plan for Health Security (NAPHS) in 2018. IHR-2005 core capacities in the areas identified by the JEE have been developed, gaps are being addressed at different levels and progress made are shared during the scheduled IHR technical working group quarterly meetings so as to assess and monitor progress made.2 A number of desk-top simulation exercises have been conducted to test and improve the existing diseases specific and multi-hazard preparedness and response frameworks. These include but are not limited to the one regional Rift Valley Fever field simulation exercise in 2018 and Ebola Viral Disease field simulation exercise in Tanzania in 2018. The United States Agency for International Development (USAID)-supported the anthrax and rabies after-action reviews to test the multi-sectoral preparedness and response to public health events in Tanzania in identifying their strengths and gaps for better responses in future, in case such outbreaks recur.2
Literature review
Zoonotic diseases account for 70% of emerging infectious diseases in humans. More than three-quarters of the emerging zoonoses are the result of wildlife-origin pathogens.3,4 The rising number of emerging zoonoses are driven by modernization of farming practices, particularly in the developing world, habitat destruction, climate change, expanded encroachment of wildlife and forestry resource ecosystems, food consumption habits, environmental pollution and enhanced global movements of people, goods and services.5,6 While emerging zoonoses are often a greater concern to donors and decision-makers, endemic zoonoses have a greater societal impact on neglected populations than emerging diseases. Many of the endemic zoonoses are part of the group of diseases called the neglected tropical diseases (NTDs) that “affect mainly poor and marginalized populations in low-resource settings”.7,8
Control of zoonoses in most sub-Sahara African countries is poor in both human and animal populations. Rabies for instance, causes an estimated 59,000 human deaths worldwide each year, primarily as a result of bites from rabid dogs. Of this number, 96.0% occur in Africa and Asia.8,9 Rabies causes significant public health and economic problem in developing countries where canine rabies is endemic. Bites from suspect rabid animals impose a substantial financial burden on affected households, especially for poor rural bite victims who suffer excessively high costs in obtaining post exposure prophylaxis compared to those from urban areas, and are less likely to receive vaccine.8,10,11 In Tanzania, an estimated 1,500 people die due to rabies every year. Rabies outbreaks have been reported in different regions including Mara, Kilimanjaro, Morogoro, Dodoma, Tanga, Arusha and Manyara regions.7,9,12
Anthrax on the other hand, has been associated with animal keeping, consumption of undercooked or raw infected meat or other animal products or working in establishments where wool, goat skins, and pelts are stored and processed.13 Anthrax is enzootic in many countries with sporadic outbreaks. Experience shows that countries with inadequate veterinary and public health facilities, and areas where it is difficult to implement control programmes are the most affected.14 West Africa is the most affected area of the world followed by Central America, Spain, Greece, Turkey, Albania, Romania, central Asia, and the Middle East.15 In Tanzania, an epidemic of 239 human cases of anthrax was reported in Rukwa region in 1985 mainly due to consumption of meat from infected animals dying of the disease.16 Outbreaks have also been reported in different parts of the country, the last one being in Arusha and Kilimanjaro regions where significant wildlife and domestic animal deaths and human morbidity were reported.17
After-action review
After-action review is an evaluation approach that uses lessons or experiences gained from past events in order to adopt best practices, thereby paving way for achievement of intended targets in future interventions.18,19 The World Health Organization (WHO) defines after-action review as a qualitative review of actions taken to respond to a public health event or following a project or a public health intervention as a means of identifying and documenting best practices demonstrated and challenges encountered during the response to the event or the implementation of the project.20 The WHO stresses on after-action review to demonstrate the functionality of national capacities in preparing for, detecting and responding to a public health event and to identify the corrective actions needed to institutionalize any lessons emerging from the management of public health events.20
Anthrax outbreak in Selela village, Monduli district, Arusha region
Monduli district is in Arusha region, in Northern Tanzania. The district forms part of the northern tourist circuit, surrounded by some of the world’s most famous natural attractions. It is these resources that attract visitors from around the world, who come to spend their holidays and so are the hunting sites and historical Olduvai Gorge. The large part of Monduli district is game-controlled (about 95%), where wildlife migrate in the wet season from surrounding national parks. It is estimated that 95% of the community inhabiting Selela ward are livestock keepers and 5% are involved in crop production and business. Although there are other ethnic groups in the district, Maasai are the major ethnic group constituting about 40% of the entire population. The main activity of the Maasai is nomadic livestock keeping.
In December 2016, the OHCD of the PMO received reports of confirmed anthrax from wildlife carcasses, deaths of domestic animals and occurrence of anthrax suspected cases in humans in Selela ward in Monduli district. It was reported that 19 of the suspected human cases from livestock keeping communities in 16 households reported to Selela, Mungere, Mswakini, Oltukai, Simangori and Mto wa Mbu health facilities where they were treated for anthrax and were progressing well after receiving. The number of livestock that were reported to have died because of the outbreak included 11 cattle, 17 goats and three sheep, with no human deaths. In wildlife, 89 wildebeests, 13 Grant’s gazelles and one hare were confirmed to have died of anthrax.
Human cases were treated with benzylpenicillin sodium injection and amoxicillin oral dose for 5-7 days. Anthrax from wild animal carcasses was confirmed by methylene blue stained blood smears and Polymerase Chain Reaction (PCR) at Tanzania Veterinary Laboratory Agency (TVLA), Arusha centre. Carcasses of domestic livestock were not available for sampling; they were either consumed or hidden. Carcasses of wild animals were mainly burnt (incinerated) into ashes at the death sites with the surrounding area decontaminated using formaldehyde. The cost of vaccinating an animal was estimated at Tanzanian Shiling 500 ($0.25), though with the privatization of the vaccination, it was much higher in some locations.
Rabies outbreak in Ulanga and Malinyi districts, Morogoro region
Ulanga and Malinyi districts are located in the Southern part of Morogoro region. The districts are bordered by a number of national parks and game reserve areas that include the Udzungwa National Park, Nyerere National Park, Saleou Game Reserve, Kilombero Basin Reserve, Ndororo Forest Reserve, Mbangayao Forest Reserve, Ligamba Forest Reserve and Nambinga Forest. Common wild animals in the forests and reserved areas include foxes, hyenas, wild dogs, leopards, monkeys, elephants etc. The tribes that live in the districts include the Pogoro, Ngindo, Ndwewe, Ndamba, Ngoni, Sukuma, Maasai, Barabaig, Kuria, Hehe, Kinga and Bena. Most of these tribes are primarily migrant from other regions. The main economic activities are food and cash crops farming and animal husbandry. Dogs and cats keeping is a common practice in the districts with some households keeping more than 10-15 dogs and 5-7 cats.
The rise in number of cases of animal bites from Ulanga and Malinyi districts was reported to local and higher authorities in late 2018. By January 2019, cumulatively, 153 human bite cases and 2 deaths were reported. Review of records indicated that from 2007 to April 2019, 119 cases of rabies were confirmed in dogs and human dog bite cases were 1455. Human dog-bite cases were referred to respective district hospitals for management where rabies post-exposure prophylaxis was also provided. Vaccination of dogs and cats in the district started on 24thApril 2019 with support from Food and Agriculture Organization of the United Nations (FAO) and USAID. By April 2019, a total of 608 domestic animals including dogs (508) and cats (105) were vaccinated.
Objectives of rabies and anthrax after-action reviews
The objectives of rabies and anthrax responses’ after-action reviews were to establish and describe actions undertaken by the multi-sectoral investigation and response teams during planning and deployment, execution of field activities, and outbreak investigation and response, to determine system strengths, deficiencies or gaps that may have contributed to delays in preventing the outbreaks and to assess preparedness measures put in place at the national and sub-national levels across the human and animal health sectors for outbreak prevention, detection and response.
Materials and methods
Design
The after-action reviews were designed as cross-sectional surveys with participatory approach. Investigators were members of the One Health platform under the coordination of the OHCD. They were engaged in developing the concept notes and proposal for the after action-review, as well as in the data collection, data analysis, report writing, dissemination and planned follow-up actions.
Ethical considerations
Responders during data collection were government employees who were acting in their official capacities as key players during outbreak response. No ethical approval was required for their participation in the interviews nor focus group discussions and no human nor animal sample was taken through any invasive procedure.
Sampling and data collection methods
In each after-action review, the investigation team randomly selected one member from the Epidemiology Unit and one member from the Emergency Preparedness and Response Unit of the Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC), one veterinary epidemiologist from the Ministry of Livestock and Fisheries (MoLF), and the other from the Tanzania Veterinary Laboratory Agency (TVLA), and lastly a wildlife/veterinary epidemiologist from the Ministry of Tourism and Natural Resources for face to face/one-on-one interview at the national level. All the interviewed persons played a role in the response to these outbreaks. At the sub-national level i.e. at the regions, districts and village levels (community), the team conducted focus group discussions with key responders (Figure 1) and randomly selected cases from members of the community who consented. The plan was to have around 10 participants at each level to participate in focus group discussions. Prior visits, information was sent to the regional, district and village authorities a week earlier. At the regional level, some staff were appointed to accompany the teams to affected districts and villages.
Data collection tools and analysis
Semi-structured, open and closed-ended questionnaire were administered to collect information in one-on-one in-depth interviews at the national level and cases while lead questions were used to engage responders in focus group discussions at the subnational levels.
Questions were mainly on inter-sectoral communication and collaboration, preparedness activities such as vaccination to prevent occurrence of diseases, data collection and sharing, awareness campaign, capacity building, enforcement of laws on prevention etc. and response activities such as vaccination during outbreaks, presence of response guidelines, coordination of response and multi-sectoral communication and collaboration.
Data collected was mainly qualitative. At the national level all responses from responders were collated into themes that were summarized into the three categories above i.e. intersectoral communication and collaboration as one category, multi-sectoral preparedness as the second category and multi-sectoral response as the last. In focus group discussions, responses based on consensuses were grouped the three categories above.
While the anthrax after-action review was conducted from 22nd to 29th of August 2017, eight months after emergency response activities were concluded, rabies outbreak after-action review took place from 28th May to 7th June 2019, a month after the outbreak was controlled. Funds for anthrax after-action review were obtained from the USAID-Preparedness and Response project and for rabies after-action review were obtained from USAID-funded Human Resource for Health (HRH2030) under Chemonics International.
Results
The cadres of staff who were ultimately involved in the interviews at the national level and those engaged in focus group discussions at subnational level are as indicated in Tables 1 and 2 below.
Village/community level
Dog bite cases in the community
Three humans with dog-bite cases were interviewed, one from Malinyi and two from Ulanga, two of them were male and one female. All three admitted having been aware of rabies, mode of transmission and how it is managed before they were bitten by dogs. Two of them were sent to nearby health facilities for bite wound care within 24 hours and one was sent to district hospital after 72 hours. All of them received Post- Exposure Prophylaxis (PEP) at district hospitals which were at a range of 5-40 kilometers from their homes. Two of the cases finished the recommended 4 doses, but one received only two doses as she did not have enough funds for the third and fourth doses. On average, dog-bite cases spent 2 weeks of inactivity attending to treatment. The cost for one dose of rabies PEP was Tanzanian Shilling 23,000 ($11) including transport cost, meals and other indirect costs. On average, a single case incurred an estimated 200,000 Tanzanian shilling to complete PEP doses. The amount included, the costs for PEP, hospital charges, transport and meals. This had significant negative economic impact on adults who are breadwinners in the households and consequent negative academic impact on pupils.
Figure 1.
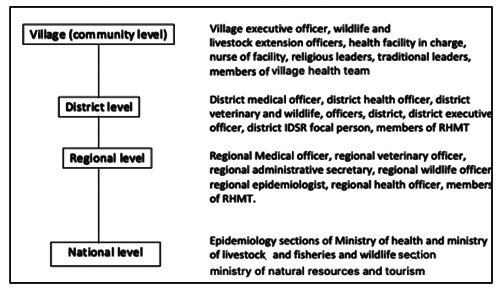
Administrative levels and available interviewees.
Inter-sectoral communication and collaboration
The results of the study demonstrated that adoption of OH approaches underpinned by multisectoral communication and collaboration was low at the village or community level for both rabies and anthrax as human cases which were captured through the electronic Integrated Disease Surveillance and Response System (eIDSR) were reported directly to MoHCDGEC. Information was rarely communicated to local animal health counterparts at grass root level. Initiation of responses by grass root animal health experts was mainly a result of instructions from the national level i.e. MoLF rather than communication between local human and animal health experts at community level after MoLF having been informed by MoHCDGEC.
Multi-sectoral preparedness
It was apparent that vaccination of dogs and cats against rabies was not routinely conducted in Malinyi and Ulanga districts, as often there was a lapse of two years between vaccination cycles. The coverage was also low. Vaccination was done mainly through donor support rather than being a mainstream activity of the animal health sector. On the other hand, enforcement of by-laws that govern animal vaccinations was weak and there was apparently low compliance in adopting best practices involving keeping of few secured dogs as often large numbers of dogs were routinely seen accompanying men when going to work on their farmland and/or hunting. On the other hand, local health facilities lacked PEP supplies largely as a result of high costs of maintaining the cold chains. Often PEP supplies had to be brought by MoHCDGEC upon receiving reports of disease outbreaks thereby taking more than two weeks to reach affected areas and hence delay treatment of victims. In Monduli district, vaccination coverage for anthrax was also apparently low. This was attributed to high costs involved and most Maasai associating the disease with weed poisoning while others linking it with altered taste and reduced milk production.
Table 1.
Interviewees and composition of focus group discussions in anthrax outbreak after-action review.
| Sector/admin level | Interviewees | Number |
|---|---|---|
| MoLF | Veterinary Epidemiologist, Tanzania Veterinary Laboratory Agency | 2 |
| MoHCDGEC | Epidemiology Section, Emergency Preparedness and Response Unit | 2 |
| MNRT | Wildlife Epidemiologist | 1 |
| Arusha region Response Team | Regional Medical Officer (RMO), Regional Health Officer (RHO), Regional Veterinary Officer (RVO) representative, Regional Nurse Officer (RNO), 2 clinicians from regional hospital, regional IDSR focal person, 2 nurses from regional hospital, 2 clinicians from regional hospital and Regional Wildlife Officer (RWO) | 11 |
| Monduli district Response Team | District Medical Officer, 2 clinicians from district hospital, 1 nurse from district hospital, District Health Officer, District Veterinary Officer, District Veterinary Epidemiologist, IDSR focal person, District Game Officer | 9 |
| Key stakeholders in Selela village | Village animal health officer, local health facility in-charge, clinician from local facility, ward game officer, health facility nurse, Selela village executive officer, 4 traditional leaders (Laigwanans) | 10 |
| Total | 35 |
Table 2.
Interviewees and composition of focus group discussions in rabies outbreak after-action review.
| Sector/admin level | Interviewees | Number |
|---|---|---|
| MoLF | Veterinary Epidemiologist, Tanzania Veterinary Laboratory Agency | 2 |
| MoHCDGEC | Epidemiology Section, Emergency Preparedness and Response Unit | 2 |
| MNRT | Wildlife Epidemiologist | 1 |
| Morogoro region Response Team | Regional Medical Officer, Regional Health Officer, Regional Nurse Officer, 2 nurses from regional hospital, 2 clinicians from regional hospital, Regional Surveillance Officer, Regional Veterinary Officer, Veterinary Epidemiologist from Ministry of Natural Resources and Tourism | 10 |
| Ulanga district Response Team | District Medical Officer, District Health Officer, District Veterinary Officer, IDSR focal person, District Game Officer, clinician from district hospital, staff from District Medical Office, 3 members from District Health Management Team in Ulanga | 10 |
| Malinyi district Response Team | District Executive Secretary, representative of District Medical Office, District Health Officer, 2 nurses from district hospital, District Veterinary Officer, Surveillance Officer (member of IDSR team), District Wildlife Officer, doctor in-charge district hospital in Malinyi | 10 |
| Village response team in Ulanga | Local health facility in-charge, a nurse of a local facility, 2 ward wildlife extension officers, 2 ward livestock extension officers and 4 village executive officers in Ulanga | 10 |
| Village response team in Malinyi | Local health facility in-charge, 2 nurses of a local facility, 1 ward livestock extension officer and 2 village executive officers in Malinyi, 4 village executive officers | 10 |
| Ulanga and Malinyi dog bite cases | 3 | |
| Total | 58 |
The review also revealed that the eIDSR system in the two study sites was well established; with cases being reported to the higher levels in real time. Conversely, the surveillance system in the animal health sector in the two regions was mainly paperbased and often takes time to reach MoLF. It was also apparent that community health workers in the human health system were responsible for providing information about disease outbreaks to the community members. They were, for instance, instrumental in dealing with anthrax outbreak in Monduli district. The situation was however rather different in the animal health sector where there was apparent shortage of extension agents at community level to capture disease events. For instance, in Malinyi and Ulanga districts there were only 18 livestock field officers who served 29 wards with 59 villages. In both districts, one wildlife game officer or veterinary extension officer was found to be serving an average of ten villages. There were no veterinary officers in the two districts.
In Monduli, where there are also national parks and game-controlled areas, the first observed case of anthrax was from wildebeest. The presence of wildlife in close proximity or at times sharing grazing sites with livestock, makes transmission of anthrax from wildlife to livestock almost inevitable, the converse is also true. It was found out that vaccination of livestock against anthrax was not well covered. The Maasai who keep large number of cows, goats and sheep, did not vaccinate their animals due to a number of reasons. Some thought it was expensive and not worth it, some thought the death of animals was attributed to a particular weed and not anthrax, and other had an unfounded myth that vaccination affecting taste and production of milk.
Local facilities could not afford to maintain cold chain and hence they lacked PEP. Rabies vaccines had to be brought from higher levels (either district, regional or national levels) some with support from development partners i.e., not readily available locally. eIDSR was found to be well established in human side i.e. cases are reported to the higher levels in real time while surveillance system in animal side was found to be mainly paper-based hence it took time for information to reach higher levels.
Community Health Workers (CHW) were also used to communicate the outbreak information among the community members in both regions. These were used effectively following anthrax outbreak in Monduli district that occurred in February. With respect to animal sector, there was a shortage of staff at the community level in both regions. It was established that one wildlife and one veterinary extension officers served ten villages.
Multi-sectoral response
There was only one dispensary in Selela ward that served several other wards and was manned by one clinical assistant who also oversaw the eIDSR. The facility laboratory was not capable to diagnose anthrax due to lack of reagents. Diagnosis of anthrax hence based on presenting symptoms. Samples collected were therefore sent to the Arusha-based zonal veterinary laboratory, a distance of two hours from Selela village.
During anthrax outbreak, the Tanzania Wildlife Research Institute (TAWIRI) proactively led the response system by providing wildlife veterinary staff to conduct disease investigation and follow-up carcasses disposal and disinfection. Other wildlife authorities such as Tanzania National Parks Authority (TANAPA) and Ngorogoro Conservation Area Authority (NCAA) provided material and logistical supports and staff time. The responses by TAWIRI, TANAPA and NCAA were driven by the fear related to the negative impact of the disease on the communities but more importantly on the tourism industry, a substantial revenue earner for the Tanzania economy. Despite this prompt response of the wildlife health sector, the mainstream animal health sector’s response was poor and slow partly because of shortage of extension staff at community level as one agent often served a number of villages. This was further compounded by lack of transport to facilitate disease investigation and response. Furthermore, it was evident that animal health staff in the two study sites often take a long time to respond to disease events. At times, it took months thereby leading to most community members being helpless for appreciable durations and forced to endure various forms of disease scourges attributable to continued presence of, for instance, rabid dogs in the villages.
It was also apparent that when the afteraction review team arrived at the village level, no proper vaccination records were available and as such it was difficult to establish when and how many dogs had been vaccinated. It was however clear that when dogs were vaccinated, cats were often not included because of inadequate numbers of animal health extension staff, the difficulty of restraining cats, coupled with their more intense roaming and scavenging behaviours. Neither preparedness and response guidelines nor standard operating procedures (SOPs) were available at the community level.
On the other hand, the health service seeking behavior of some community members was a notable setback to enhanced access to quality services as some patients often sought medical help from local healers first and resorted to seeking conventional healthcare services only when disease had progressed enormously, and prognosis was already not favourable. This often caused most health facilities to handle severe or terminal cases. Poor transport network in rural areas and high cost of PEP regimen were also cited as drivers for some community members seeking health services from traditional healers as the first option. Lack of funds for emergencies was often a limiting factor, and anthrax vaccination was done periodically through the support of NCAA, FAO and the Serengeti Health Initiative. In the case of rabies, vaccination was also delayed because of the observed weaknesses of the national capacity to mobilise resources.
Scope and nature of multisectoral collaboration and communication at the district level
Inter-sectoral communication and collaboration
Although, human and animal health experts in Malinyi and Ulanga districts were aware of the value of OH approaches, their mainstreaming in disease surveillance systems was lacking and this was despite the knowledge having been imparted through previous retooling courses offered by Southern Africa Center for Infectious Diseases Surveillance (SACIDS). However, there existed some forms of inconsistent communication between the human and animal sectors when disease events occurred. A good example is the information about a human rabies case in a village in Ulanga district that was communicated to the District Medical Officer (DMO), who in turn informed the District Veterinary Officer (DVO), thereby leading to rabid dogs being traced and other veterinary interventions initiated. The same applied with anthrax outbreak in Selela, in Monduli district that led to formation of the multi-sectoral response team, an activity that was coordinated by the Monduli District Executive Director’s (DED) office.
Multi-sectoral preparedness
The robust eIDSR system was able to generate weekly disease reports that were received from the community level and thereafter transmitted to MoHCDHEC. Except for some areas that had rolled out Afya data and Event-based Mobile Application system (EMA-i), paper-based surveillance system in the animal health sector was a major source of surveillance data at the district level. There was a general outcry of lack of funds to respond to disease events in the two sectors. It was also reported that human resource availability in the human health sector was close to being adequate in the three districts, however for the case of the animal sector, staff numbers were often inadequate. For instance, there were no veterinary doctors in Malinyi and Ulanga districts despite the requirements of the Animal Disease Act No 16 of 2003. It was evident that experts in both sectors had no up to-date information on preparedness and response protocols and availability of emergency resources such as PPE vaccines, syringes etc. was often poor.
Advocacy on rabies in primary schools and the communities using animal extension officers had been done previously through mass media channels for which important information on rabies and other health education information was shared. Despite this, there was weak enforcement of the requirement of rabies vaccination as demanded for by the by-laws, which also spelt out the penalty to the tune of Tanzanian Shilling 50,000 ($25) for each non-vaccinated dog. The by-laws also required dog owners to shoulder costs of treatment of dog bite victims. In addition, there was no national guidelines on preparedness and response that were present in the study districts; rather only those provided by international organizations such as WHO/OIE/FAO were available in the office of the DVO.
Multi-sectoral response
Although, district emergency response teams existed in the three study districts, was no evidence of formal multi-sectoral collaboration and communication and this was in spite of previous OH retooling courses offered by SACIDS and “Afyadata” project. Rabies disease response activities and resource mobilization were coordinated by DED through participation of staff of Ifakara Health Institute, Sokoine University of Agriculture, sector ministries and one non-governmental organization. The multisectoral team that responded to anthrax outbreak in Monduli district was composed of staff from offices of DVO, DMO as well as other cadres of human and animal health experts.
Scope of multisectoral collaboration at regional level
Intersectoral communication and collaboration
High level of awareness of One Health approach was evident at the regional level and hence formal and informal communication between sectors was well established. For instance, the Regional Veterinary Officer received outbreak information from the Regional Medical Officer due to the established communication between them. Staff at the regional level attended meetings that advocated One Health approach. At this level, joint meetings among staff of sectors were also common. Apart from human, animal, and environment sectors, other institutions involved included Tanzania Wildlife Management Authority (TAWA), TAWIRI, TVLA, ZVC, Red-Cross and NCAA.
Multi-sectoral preparedness
While the Morogoro Regional Medical Officer (RMO) office relied on eIDSR for surveillance data, the regional veterinary office (RVO) had only a few areas with Afya data for electronic surveillance data sharing. Most of the districts had paperbased animal disease surveillance system. Human resource was adequate in human health sector as compared to animal health sector but there was general lack of supplies like anti-rabies vaccine and rabies toxoid. Although from time to time the government and partners supported rabies vaccination, dog owners depended mainly on private sector to have their animals vaccinated.
Preparedness and response guidelines such as the IDSR guidelines, Public Health Act 2009, guidelines for treatment of common diseases of year 2013 were available and there was an adequate stockpile of drugs at the regional hospital. On the animal side no specific guidelines for anthrax diagnosis and management were present at the RVO, there were only SOPs for roles of DVOs. Anthrax vaccine was inadequate and there was evidence of low vaccine coverage done by NCAA and TANAPA. There was low compliance to vaccination attributed mainly to the cost of vaccination. It was clear that enforcement of the existing bylaws that require animals to be vaccinated were not done.
Multi-sectoral response
Outbreak response roles and responsibilities were shared between actors. Coordination of emergency response was done by RMO instead of the regional administrative secretary in both Arusha and Morogoro regions. Key actors were from sectors and institutions including human health, animal health, wildlife, the Sokoine University of Agriculture, Ifakara Health Institute, Muhimbili University of Health and Allied Sciences among others. During rabies outbreak response, dog vaccination was done using veterinary staff and trained volunteers as there wasn’t adequate veterinary staff to conduct the vaccination. Funds for response were secured from partners and antirabies vaccines were procured from Medical Stores Department.
Rabies outbreak daily reports and information sharing were effected through the formation of a rabies response WhatsApp group. In the veterinary sector, field officers shared outbreak report with the DVO, and the RVO only played response roles on request. Surveillance form in each district was sent to the regions every month for monthly reports. Weakness in the enforcement of bylaws was observed during response as there were no mandatory routine animal vaccination against zoonotic diseases including rabies and penalties were not imposed on defaulters.
Scope of multisectoral collaboration at national level
Intersectoral communication and collaboration
The existence of the national One Health platform coordinated by the OHCD ensured coordination of multi-sectoral emergency response. Virtual and physical meetings (teleconference) were conducted under the auspices of the Public Health Emergency Operating Centre (PHEOC) of the MoHCDGEC. Key players included staff of MoHCDGEC, MoLF, research and academic institutions, regional and district authorities. The meetings also mobilized resources for joint response activities including planning for awareness campaigns, investigation and vaccination.
Multi-sectoral prepared
Surveillance data captured through eIDSR system allowed for information flow to MoHCDGEC whereas MoLF relied on the paper-based submission system. Information captured through eIDSR was key to initiation of national level responses coordinated by OHCD. National level authorities also organized joint desktop and field simulation exercises to test the capacity for preparedness and response frameworks and also to address gaps identified during JEE.
Multi-sectoral response
Multi-sectoral Rapid Response Teams were found to exist at the regional level in Arusha and Morogoro regions. The MoHCDGEC, through the PHEOC coordinated response to anthrax and rabies, however there was a delayed in vaccination of dogs due to unavailability of vaccines and staff to vaccinate. During anthrax outbreak, email and WhatsApp groups were created, which included sectors and other key players who shared information about the outbreaks. Key players included the MoLF, MoHCDGEC, FAO, Ifakara Health Institute (IHI), RMOs, RVOs, DEDs, DMOs, DVOs eIDSR and HMIS focal points.
Where there was Afya data or EMA-I, the MoLF obtained outbreak data through electronic information system from the outbreak areas. In other areas, outbreak data was obtained through Zonal Veterinary Centres (ZVCs) and districts. Districts filled surveillance forms, scanned and sent them via email to the MoLF and copied to the ZVCs. Funds for emergency were not readily available. This necessitated partners to avail support in different forms including funds, transport and supplies. The MoLF requested rabies vaccine from development partners such as FAO and other partners such as the Serengeti Health Initiative.
Discussion
Tanzania has made notable steps in the utilisation of OH approaches in dealing with zoonoses and other risks of public health concern. During the zoonotic diseases’ prioritization (ZDP) exercise, anthrax and rabies were selected among the leading zoonoses of public health importance, for purposes of inclusion in major disease prevention and control strategies. The exercise was in line with the requirements of the National One Health Strategic Plan (NOHSP) of 2015-2020 and the JEE recommendations. The ZDP, plus other major activities that have been carried out during data collection, underscored the country’s commitment to and compliance with the GHSA, the International Health Regulations (IHR), 2005 and OIE Performance of Veterinary Services (OIE PVS).
Despite the above efforts, a number of challenges and operational gaps were identified in the areas of information sharing, preparedness and response capacities that required prompt corrective actions. Mainstreaming of OH approaches in disease surveillance and response at community level where first responders and frontline workers are supposed to act was lacking. This certainly undermines real time disease reporting and rapid response capacity at disease sources. Lack of funds to carry out active disease investigation and paperbased disease surveillance system in animal sector were also a major challenge coupled with uncoordinated lack of PEP vaccines in district and regional hospitals as a result of high costs of maintaining the cold chain. In addition, there are lack of routine vaccination programmes for rabies and anthrax because of fragmented veterinary service supply chain and the resources to enable disease investigation and responses are lacking because of heavy reliance on donor support.
Building the capacity of first responders including recruitment, training, conducting OH awareness at community level and engagement DVOs, DMOs, RVOs, RMOs and regional and district policy makers and planners should be planned for better preparedness and response to anthrax and rabies outbreaks in future. The OHCD needs to strengthen its coordination role and ensure that multisectoral teams are formed at all levels; their functionality improved and OH principles are adequately mainstreamed in human and animal health system. In the final analysis, these findings therefore call for immediate, mid-term and long-term plans to alleviate the negative impacts of public health emergencies in rural livelihood and social wellbeing and the national economy.
Conclusions
Whereas a number of desktop and field simulation exercises have been conducted in Tanzania to assess and strengthen multisectoral preparedness and response to public health threats, very few after-action reviews have been conducted for the same. According to the WHO, a well-planned after-action review can assess the functionality of public health preparedness and response capacities during a “real” event, offering unparalleled opportunities to reflect on gaps, lessons learned, and best practices following responses to public health events.
The current study has demonstrated the value of after-action reviews in identifying technical gaps that need to be addressed by the One Health stakeholders under the coordination of the OHCD, in particular the IHR-2005 core capacities, in order to strengthen multisectoral partnership in handling public health events or major concern. It emphasizes the importance of after-action review as a tool to complement other existing efforts such as the mandatory States Parties Annual Reporting (SPAR) and Simulation Exercises (SimEx) if it is based on embracement of collective learning and OH approaches. It is however, important that after-action reviews are done soon after the event in order to gather relevant information that depends on recall ability of respondents. Key sectors therefore, under the coordination of the OHCD, should include after-action reviews in their annual plans, work out ways to mobilize resources locally so as build a robust foundation for assessing the capacity of multi-sectoral preparedness and response in dealing with public health emergencies in due times.
Limitations
Delayed anthrax outbreak response after-action review was attributed to the processes in securing funds to execute it. As a result, due to a long period lapse, recall bias contributed to lack of some of the details relevant for the after-action review report.
Acknowledgements
The authors are very grateful to USAID-Preparedness and Response project and USAID-funded Human Resource for Health under Chemonics International for provision of financial support and all respondents who took part in this study. The authors are also thankful to all those who enabled the study to be conducted in the Monduli, Malinyi and Ulanga districts.
Funding Statement
Funding: The study was part of the generous support from the USAID to multi-sectoral preparedness and response to public health threats in Tanzania 2015-2020. No funding was solicited for manuscript preparation.
References
- 1.Government of Tanzania (GOT). The National One Health Strategic Plan 2015-2020. 2015. [Google Scholar]
- 2.United Republic of Tanzania (GOT). Tanzania National Action Plan for Health Security. 2018. [Google Scholar]
- 3.World Health Organization. (2004). Food and Agriculture Organization of the United Nations (FAO) & World Organisation for Animal Health (OIE). – Report of the WHO/FAO/OIE joint consultation on emerging zoonotic diseases, 3 to 5 May, Geneva. WHO, Geneva. [Google Scholar]
- 4.Jones KE, Patel NG, Levy MA, et al. Global trends in emerging infectious diseases. Nature 2008; 451: 990–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grace D, Mutua F, Ochungo P, et al. Mapping of poverty and likely zoonoses hotspots. Zoonoses Project 4. Report to the Department for International Development, UK; 2012; 1–119. [Google Scholar]
- 6.Wang LF, Crameri G. Emerging zoonotic viral diseases. (Revue scientifique et technique (International Office of Epizootics) 2014; 33(2):569–81. [DOI] [PubMed] [Google Scholar]
- 7.Kipanyula MJ. Why has canine rabies remained endemic in the Kilosa district of Tanzania? Lessons learnt and the way forward. Infect Dis Poverty 2015; 4:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Rabies vaccine. WHO position paper – Weekly Epidemiological Record; Switzerland;. 2018;18 also available at: http://www.who.int/rabies/resources/who_wer9316/en/ [Google Scholar]
- 9.Changalucha J, Steenson R, Grieve E, et al. The need to improve access to rabies post-exposure vaccines: Lessons from Tanzania. Vaccine 2019;37:A45-A53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knobel DL, Cleaveland S, Coleman PG, et al. Re-evaluating the burden of rabies in Africa and Asia. Bulletin of the World Health Organization 2005;360-368. [PMC free article] [PubMed] [Google Scholar]
- 11.Sambo M, Cleaveland S, Ferguson H, et al. The burden of rabies in Tanzania and its impact on local communities. PLoS Negl Trop Dis 2013;7:e2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.FAO report. Government, FAO and USAID join hands to fight against rabies in Moshi. 2018. Also available at: http://www.fao.org/tanzania/news/detail-events/en/c/1133102/ [Google Scholar]
- 13.Montecucco C, Mock M. (eds). Anthrax. Molecular Aspects of Medicine 2009;30;345-510. [DOI] [PubMed] [Google Scholar]
- 14.Shadomy S, Ahmed El Idrissi, Eran Raizman, et al. Anthrax outbreaks: a warning for improved prevention, control and heightened awareness. empresanimalhealth@fao.org/www.fao.org/ag/empres.html. [Google Scholar]
- 15.Turnbull PC, Hugh-Jones ME and Cosivi O. World Health Organization activities on anthrax surveillance and control. Applied Microbiol 1999;87:318-20 [DOI] [PubMed] [Google Scholar]
- 16.Webber RH. Anthrax in Lake Rukwa Valley, Tanzania: a persistent problem. J Tropical Med Hygiene 1985;88:327-331. [PubMed] [Google Scholar]
- 17.Mwakapeje ER, Høgset S, Fyumagwa R. Anthrax outbreaks in the humans - livestock and wildlife interface areas of Northern Tanzania: a retrospective record review 2006–2016. BMC Public Health 2018;18:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeGrosky MT. Eighth International Wildland Fire Safety Summit 2005; 26-28. [Google Scholar]
- 19.Gurteen D. Introduction to after-action reviews. Global Knowledge Review; 2000. Retrieved on October 25, 2004 from, http://www.gurteen.com/gurteen/gurteen.nsf. [Google Scholar]
- 20.World Health Organization. Guidance for after-action review (after-action review). Geneva, Switzerland: (WHO/WHE/CPI/.4) 2019. [Google Scholar]


