Abstract
Whipple's disease is a rare disease caused by the actinomycete bacteria Tropheryma whipplei, which cause intestinal infection. The most common symptoms are chronic diarrhoea, weight loss, abdominal pain, arthritis and neurological abnormalities, which can be fatal. This paper reports a case of a 57-year-old Brazilian woman with diarrhoea, vomiting, abdominal pain, appetite loss, intermittent fever, malaise, weight loss and malnutrition. Migratory polyarthralgia and recurrent visual scotomas preceded the symptoms. The retroperitoneal pseudotumour formation finding was associated with prolonged wasting syndrome, which did not respond to usual therapies, thus leading to the investigation of carcinomatosis disease. After laparotomy, biopsy and histochemical study of the lesions with negative results for malignancy, we proceeded to the investigation of Whipple's disease, which was then confirmed. The patient improved clinically and started gaining weight after using ceftriaxone (IV).
Keywords: Whipple's disease, Tropheryma whipplei, Carcinomatosis
Introduction
Whipple's disease, caused by Tropheryma whipplei bacteria, is a rare disease, with an annual worldwide incidence of about 12 new cases. It presents gastrointestinal symptoms, mainly related to malabsorption, which is associated with systemic symptoms such as fever, joint pain, and neurological manifestations.1
Despite affecting any age group, it mainly affects white men between the fourth and sixth decades of life.1, 2 The disease pathogenesis is uncertain, but it appears to involve faecal–oral transmission of the bacillus that belongs to the Actinomycetes group. Host's susceptibility, combined with a probable cellular immunity deficit, also seems to contribute to the disease onset. Inter-human transmission cases have not been documented. The diagnosis is established by histological examination of the tissues involved, generally obtained through an endoscopic duodenal biopsy, which shows macrophages containing microorganisms positive for periodic acid-Schiff (PAS) reaction.3, 4 If the pathologic diagnosis is not possible or if there are any questions regarding the histological findings, polymerase chain reaction (PCR) is useful in the diagnostic investigation.5 There might be, among non-specific laboratory findings, increased levels of acute phase reactants, anaemia, leucocytosis, and thrombocytosis.6 Treatment consists of prolonged broad-spectrum antibiotics, preferably with agents that cross the blood brain barrier, due to the possible involvement of the central nervous system (CNS), where the local recurrence is more frequent.7
This paper aimed to report an atypical clinical manifestation of Whipple's disease with the formation of a lipophilic retroperitoneal tumour of reactive nature, simulating carcinomatosis.
Case presentation
A 57-year-old Brazilian woman, of Caucasian ethnicity, residing in the city of Ipatinga, Minas Gerais, who was previously healthy, started having diarrhoea, postprandial vomiting, abdominal pains, appetite loss, intermittent fever and asthenia. Despite the symptomatic treatments, symptoms persisted for nine months. It contributed then to a weight loss of approximately 25 kg and severe malnutrition. Intermittent headache and visual scotomas had been present for one year, and for four years, the patient complained of having arthralgia and/or migratory arthritis, especially in the ankles, knees, elbows and proximal phalanges. She did not have relevant family history or personal history of previous surgeries or hospitalizations. In spite of her countryside origin, she had resided in an urban environment for 40 years. On examination, she weighed 29 kg, was eupneic, eucardiac, febrile, pale, malnourished, with anasarca, asthenic, and unable to walk without bilateral support. She had abdomen ascites, which was generally painful on palpation. Laboratory tests showed hypochromic microcytic anaemia (Hb = 8.7 g/dL, ferritin = 332.5 ng/mL, serum iron = 15 mcg/dL) without leucocytosis, hypoalbuminemia (1.84 g/dL), hypokalemia (2.7 mEq/L) and hyponatremia (131 mEq/L). Serologies for HIV, hepatitis B, hepatitis C, celiac disease, brucellosis, antinuclear antibodies, rheumatoid factor, tumour markers, and TSH were investigated and showed negative or within normal limit results. The electrocardiogram was normal. Colonoscopy showed colonic tubular adenoma, and the anatomopathological examination showed changes that were consistent with mild dysplasia.
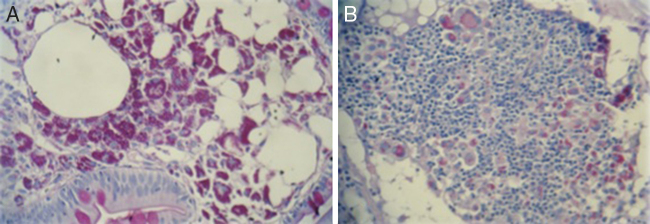
A CT scan of the abdomen revealed a heterogeneous formation consisting predominantly of fat content, with its epicentre in the retroperitoneal region, associated with diffuse densification of the abdominal mesenteric fat and the thickening of the small-bowel intestinal loop wall, whose differential diagnosis included a tumour of lipomatous lineage (Fig. 1).
Fig. 1.
CT scan showing retroperitoneal tumour to the left, with irregular, infiltrative aspect, predominantly of fat content, highlighted by the contrast, as shown by the arrow.
The prolonged wasting syndrome associated with the radiological condition, compatible with retroperitoneal pseudotumour formation, led to exploratory laparotomy for the investigation of the carcinomatous disease. The tumour removed had a brown-yellowish gelatinous microcystic appearance, measuring 9.0 cm × 6.0 cm × 4.0 cm. The retroperitoneal lymph nodes consisted of three irregular fragments of greyish tissue, measuring together 7.0 cm × 4.0 cm × 1.0 cm, containing five nodes. The anatomopathological examination revealed lymphoid/lipomatous proliferation associated with histiocytosis in adipose tissue and lymph nodes. The immunohistochemical technique excluded malignancy from the sample, featuring a nonspecific lipophilic reaction with foci of steatonecrosis and inflammatory reaction.
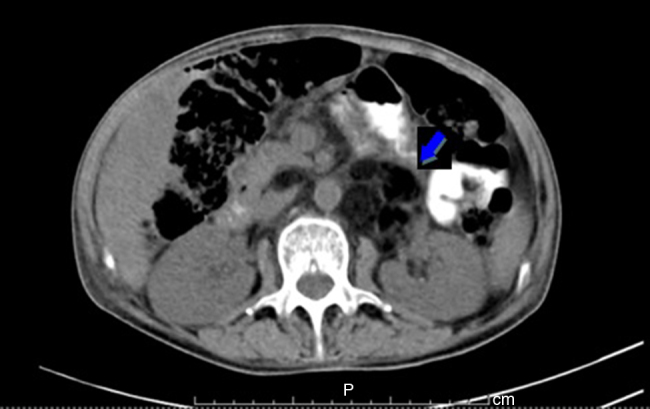
As there were chances of the disease being Whipple's disease, a high digestive endoscopy was carried out and revealed a normal macroscopic appearance. Fragments from the second portion of the duodenum were collected for histopathology, which demonstrated an increased lamina propria cellularity at the expense of histiocytes, the cytoplasm of which stained positively with PAS (Fig. 2A). The tissue removed from the abdomen was also subjected to the same procedure with similar results (Fig. 2B). Acid-fast bacilli (AFB) staining was negative.
Fig. 2.
(A) Biopsy of the second portion of the duodenum, stained with periodic acid-Schiff (PAS), 40× magnification and (B) peritoneum with PAS positive histiocytes and with numerous lymphocytes and adipocytes.
Since the clinical and histopathological findings were consistent with Whipple's disease, treatment was initiated with diuretics, vitamin and mineral replacement, and symptomatics. However, only after the introduction of antibiotic therapy with ceftriaxone (1 g, every 12 h, IV) was there a significant clinical improvement with the return of appetite and physiological bowel habit in five days. The disappearance of visual scotoma and arthralgia came next, which led to hospital discharge as soon as the 15-day antimicrobial treatment was concluded. The patient was kept on doxycycline 100 mg every 12 h, due to having developed leukopenia after the administration of trimethoprim–sulfamethoxazole for seven days. In 30 days, laboratory parameters returned to normal, she became afebrile, and gained 15 kg. After 40 days, we reintroduced trimethoprim–sulfamethoxazole successfully, as there was no episode of leukopenia again, which had been probably related to malnutrition or infectious cause.
After improvement of her intestinal condition, the patient returned to seek medical attention due to intense arthralgia in the right coxofemoral joint, as well as low back pain with significant functional limitation. She was diagnosed and then treated for sacroiliitis.
Discussion
As the annual incidence is estimated at less than 1/1,000,000 people, Whipple's disease is probably underdiagnosed. Although men are more often affected, the disease can in fact affect people of any gender or any age group, having an increased frequency in farmers or rural residents.4, 6, 8 In this report, the patient presented the first manifestations of the disease by the fifth decade of life, and according to what is described in the literature, she had worked in rice and coffee plantations from childhood to the age of seventeen years, during which she probably acquired the bacteria.
After four decades of alleged contact with the agent, the patient developed migratory symmetric polyarthralgia, which preceded the diagnosis in four years. The joint condition was intermittent, especially affecting the ankles, knees and proximal phalanges, at a moderate intensity. This is the typical frame in which osteoarticular symptoms (arthralgia and/or peripheral arthritis) – present in up to 90% of patients – often preceding in years the classic triad of the disease, diarrhoea, malabsorption and weight loss, which can cause cachexia and death if not treated.6, 9, 10 Sacroiliitis can also be found, as shown in the case above, as well as the spine condition, though both are rare.10, 11, 12
The daily visual scotoma reported by the patient disappeared after specific antibiotic therapy, and that was probably due to a neurological change. The central nervous system involvement is clinically recognized in 45% of patients and observed in 90% of them in post-mortem examination, including the asymptomatic.13 Although visual problems were excluded as the cause for such a change, the disease's ocular manifestations are described as uveitis, vitritis, retinitis, retinal haemorrhage, choroiditis, papilledema, optic atrophy, and keratitis.14
The intestinal lipodystrophy condition and retroperitoneal pseudotumour formation, associated with the prolonged wasting syndrome, led to the investigation of carcinomatous disease, which ultimately led to exploratory laparotomy, biopsy and histochemical study of the lesions. From the negative results for malignancy, we proceeded to the investigation of Whipple's disease, as the patient's condition was progressively worsening. The mesenteric panniculitis found in this case is rare and of unknown aetiology. However, among the suggested factors that trigger the process, we can mention the existence of infection and of autoimmune diseases.15, 16
Whipple's disease should be considered in the differential diagnosis of malignant tumours and lymphoproliferative diseases, as it manifests in the formation of multiple lymphadenopathy. Although it is associated with the onset of lymphomas, the peripheral and abdominal lymphadenopathy found are mostly present.17, 18 The finding of a retroperitoneal mass of fat content simulating a tumour, which was probably a reaction to the presence of the bacteria, has been poorly described in the literature, demonstrating once again the disease's manifold presentation.
Current recommendations for the treatment of Whipple's disease are based on case reports and case series retrospectively and consider the activity and pharmacokinetic properties of antimicrobials. In the absence of effective therapy, the disease is potentially fatal. The use of antibiotics that surpass the blood–brain barrier is recommended, since the CNS is often affected and very often involved in relapses. Currently, the most widely used regimen calls for the oral administration of 160 mg of trimethoprim and 800 mg of sulfamethoxazole, twice daily, for one or two years, usually preceded by parenteral administration of ceftriaxone (2 g/day) for fifteen days.7, 8, 19 In our case, we opted for doxycycline as maintenance of the antibiotic therapy due to the occurrence of leucopenia after a short course of trimethoprim–sulfamethoxazole. Reintroduction of trimethoprim–sulfamethoxazole after 40 days was followed with no changes in the leucocyte count.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgement
We are very grateful to Aloísio Bemvindo de Paula, Internal Medicine Residency Coordinator of the Márcio Cunha Hospital in Ipatinga - MG - Brazil, for the technical assistance provided.
References
- 1.Dobbins W.O., 3rd. Whipple’ disease. Mayo Clin Proc. 1988;63:623–624. doi: 10.1016/s0025-6196(12)64892-7. [DOI] [PubMed] [Google Scholar]
- 2.Moos V., Schneider T. Changing paradigms in Whipple's disease and infection with Tropheryma whipplei. Eur J Clin Microbiol Infect Dis. 2011;30:1151–1158. doi: 10.1007/s10096-011-1209-y. [DOI] [PubMed] [Google Scholar]
- 3.Neufert C., Vieth M., Monkemüller K., Neurath M.F., Neumann H. In vivo diagnosis and characterisation of Whipple's disease. Lancet Infect Dis. 2011;11:970. doi: 10.1016/S1473-3099(11)70311-5. [DOI] [PubMed] [Google Scholar]
- 4.Oliveira L., Gorjao R., Deus J.R. Doença de Whipple. J Port Gastrenterol. 2010;17:69–77. [Google Scholar]
- 5.Fenollar F., Raoult D. Molecular techniques in Whipple's disease. Expert Ver Mol Diagn. 2001;1:299–309. doi: 10.1586/14737159.1.3.299. [DOI] [PubMed] [Google Scholar]
- 6.Durand D.V., Lecomte C., Cathebras P., Rousset H., Godeau P. Whipple disease: clinical review of 52 cases. Medicine (Baltimore) 1997;76:170–184. doi: 10.1097/00005792-199705000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Keinath R.D., Merrell D.E., Vlietstra R., Dobbins W.O., III Antibiotic treatment and relapse in Whipple's disease: long term follow-up of 88 patients. Gastroenterology. 1985;88:1867–1873. doi: 10.1016/0016-5085(85)90012-5. [DOI] [PubMed] [Google Scholar]
- 8.Dobbins W.O., 3rd. Thomas; Springfield, IL: 1987. Whipple's disease. [Google Scholar]
- 9.Fenollar F., Puéchal X., Raoult D. Whipple’ disease. N Engl J Med. 2007;356:55–66. doi: 10.1056/NEJMra062477. [DOI] [PubMed] [Google Scholar]
- 10.Puéchal X. Whipple disease and arthritis. Curr Opin Rheumatol. 2001;13:74–79. doi: 10.1097/00002281-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Canoso J.J., Saini M., Hermos J.A. Whipple's disease and ankylosing spondylitis. Simultaneous occurrence in HLA-B27 positive male. J Rheumatol. 1978;5:79–84. [PubMed] [Google Scholar]
- 12.Scheib J.S., Quinet R.J. Whipple's disease with axial and peripheral joint destruction. South Med J. 1990;83:684–687. doi: 10.1097/00007611-199006000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Anderson M. Neurology of Whipple's disease. J Neurol Neurosurg Psychiatry. 2000;68:1–5. doi: 10.1136/jnnp.68.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rickman L., Freeman W., Green W., et al. Brief report: uveitis caused by Tropheryma whippelii (Whipple’ bacillus) N Engl J Med. 1995;332:363–366. doi: 10.1056/NEJM199502093320604. [DOI] [PubMed] [Google Scholar]
- 15.Patel N., Saleeb S.F., Teplick S.K. General case of the day. Mesenteric panniculitis with extensive inflammatory involvement of the peritoneum and intraperitoneal structures. Radiographics. 1999;19:1083–1085. doi: 10.1148/radiographics.19.4.g99jl221083. [DOI] [PubMed] [Google Scholar]
- 16.Moreira L.B.M., Pinheiro R.A., Alves-de-Melo A.S., et al. Paniculite mesentérica: aspectos na tomografia computadorizada. Radiol Bras. 2001;34:135–140. [Google Scholar]
- 17.Gillen C.D., Coddington R., Monteith P.G., Taylor R.H. Extraintestinal lymphoma in association with Whipple's disease. Gut. 1993;34:1627–1629. doi: 10.1136/gut.34.11.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pimentel-Nunes P., Cardoso E., Brandão C., et al. Apresentação da Doença de Whipple como linfoma. Jornal Português de Gastrenterologia. 2011;18:135–138. [Google Scholar]
- 19.Knaapen H.K.A., Barrera P. Therapy for Whipple's disease. J Antimicrob Chemother. 2007;60:457–458. doi: 10.1093/jac/dkm259. [DOI] [PubMed] [Google Scholar]