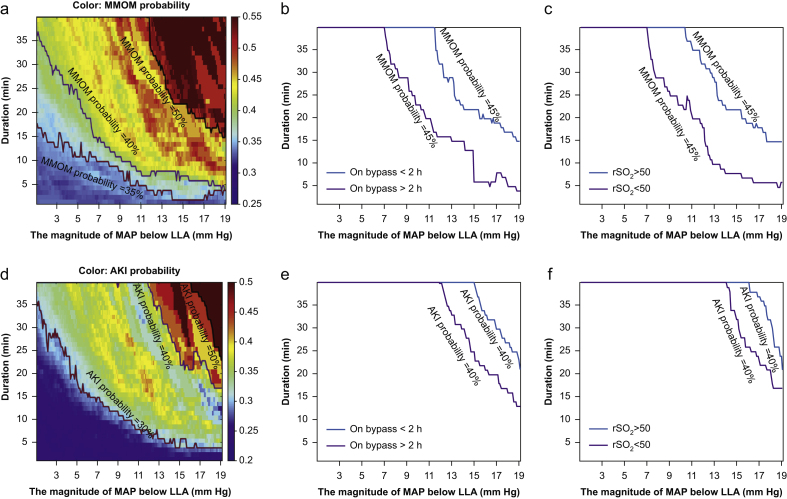
Fig 3.
Visualising the relationship between the magnitude of MAP below LLA (mm Hg), time duration (min) and occurrence of major morbidity and mortality or AKI. As an overview, each coordinate in the figures refers to a hypoperfusion episode of MAP below LLA at a certain magnitude (mm Hg) for at least a certain duration (min). For each pair of magnitude and duration thresholds, the probability of AKI or MMOM is calculated and then represented by colour codes (blue colour indicates low probability and red colour indicates high probability). The solid lines demarcate distinct transitions in probabilities for each outcome. For example, the colour coding and black line in panel (a) demonstrate that if the MAP was below LLA cerebral oximetry index by 13 mm Hg, and lasted for longer than 30 min, the probability of developing MMOM increased to 50%. Panels (a) and (d) demonstrate that the probability of both MMOM and AKI increase as both the magnitude and duration of MAP < LLA increase, with highest occurrence in the top-right corner of each panel. Panels (b) and (e) demonstrate the modifying effects of bypass duration on the probability of AKI (b) and MMOM (e). Panels (c) and (f) demonstrate the modifying effects of reduced cerebral oximetry values (regional cortical oxygen saturation [rSO2]) on probability of AKI (c) and MMOM (f). These latter panels demonstrate that patients with longer duration of cardiopulmonary bypass and lower cerebral oximetry values (rSO2) have an increased risk of AKI and MMOM even at similar intensities and duration of MAP below the LLA, as compared with patients who had shorter duration of bypass or higher cerebral oximetry values. MAP, mean arterial blood pressure; LLA, lower limit of autoregulation; AKI, acute kidney injury; MMOM, major morbidity and operative mortality.