Abstract
Background
Telemonitoring and telerehabilitation can support home-based pulmonary rehabilitation (PR) and benefit patients with lung diseases or COVID-19. This study aimed to (1) identify which telemonitoring and telerehabilitation interventions (e.g. videoconferencing) are used to provide telehealth care for people with chronic respiratory conditions or COVID-19, and (2) provide an overview of the effects of telemonitoring and telerehabilitation on exercise capacity, physical activity, health-related QoL (HRQoL), and healthcare use in patients with lung diseases or COVID-19.
Methods
A search was performed in the electronic databases of Ovid MEDLINE, EMBASE, and Cinahl through 15 June 2021. Subject heading and keywords were used to reflect the concepts of telemonitoring, telerehabilitation, chronic lung diseases, and COVID-19. Studies that explored the effect of a telerehabilitation and/or telemonitoring intervention, in patients with a chronic lung disease such as asthma, chronic obstructive pulmonary diseases (COPD), or COVID-19, and reported the effect of the intervention in one or more of our outcomes of interest were included. Excluding criteria included evaluation of new technological components, teleconsultation or one-time patient assessment.
Results
This scoping review included 44 publications reporting the effect of telemonitoring (25 studies), telerehabilitation (8 studies) or both (11 studies) on patients with COPD (35 studies), asthma (5 studies), COPD and asthma (1 study), and COVID-19 (2 studies). Patients who received telemonitoring and/or telerehabilitation had improvements in exercise capacity in 9 out of 11 (82%) articles, better HRQoL in 21 out of 25 (84%), and fewer health care use in 3 out of 3 (100%) articles compared to pre-intervention. Compared to controls, no statistically significant differences were found in the intervention groups’ exercise capacity in 5 out 6 (83%) articles, physical activity in 3 out of 3 (100%) articles, HRQoL in 21 out of 25 (84%) articles, and healthcare use in 15 out of 20 (75%) articles. The main limitation of the study was the high variability between the characteristics of the studies, such as the number and age of the patients, the outcome measures, the duration of the intervention, the technological components involved, and the additional elements included in the interventions that may influence the generalization of the results.
Conclusion
Telemonitoring and telerehabilitation interventions had a positive effect on patient outcomes and appeared to be as effective as standard care. Therefore, they are promising alternatives to support remote home-based rehabilitation in patients with chronic lung diseases or COVID-19.
Keywords: Telerehabilitation; home telecare; telecare; ehealth, telehealth, telemonitoring, COVID-19, COPD
Introduction
Chronic lung diseases and COVID-19 are leading causes of disease, death and disability globally1–4 which entail a substantial burden on the individual5–7 and healthcare systems.8,9 Pulmonary rehabilitation (PR) is defined by the “National Heart, Lung, And Blood Institute” as a “supervised program that includes exercise training, health education, and breathing techniques for people who have certain lung conditions or lung problems due to other conditions” 10 is widely recognized as an important treatment for patients suffering from chronic respiratory diseases,11,12 and has been recommended as a potential beneficial intervention for post-COVID-19 patients. 13 PR has been shown to provide statistically and clinically significant improvements in physical activity, exercise capacity, self-efficacy, and health-related quality of life (HRQoL), and a decrease in healthcare use in patients with lung diseases.11,14 Despite the multiple benefits identified, it has been estimated that less than 3% of people with chronic lung diseases accessed PR programs 15 which are also hampered by low participation, insufficient attendance, and high dropout rates.16–19 Home-based PR programs seem to offer a promising alternative20,21 to overcome well-known PR barriers including, but not limited to, symptom severity, acute exacerbations, transportation, financial difficulties, disruption of daily routines and access to care in remote locations.17,18,22–25 In addition, the COVID-19 pandemic has highlighted the need for delivering PR programs remotely, safely, and efficiently. 15
Advances in technology have boosted at-home health service delivery26,27 and popularized telehealth for those with chronic diseases.27–30 Telehealth can be described as the use of electronic information and communication technology by professional health care providers to provide and support at-home health care to patients in case of long distances. 31 Evidence indicates that telehealth can enhance healthcare use,32,33 especially among the populations who cannot otherwise access care. 34 There are several terms used to describe telehealth systems based on their applications. Telerehabilitation is defined as the delivery of rehabilitation services (e.g. assessment, prevention, treatment, education, and counseling) via information and communication technologies. 35 It has been associated with lower healthcare costs compared with traditional inpatient or person-to-person rehabilitation.36,37 Recent advances in sensor technology have also enabled remote patient telemonitoring, which is the transmission of physiological and other noninvasive data (e.g. heart rate, blood pressure, oxygen saturation, weight, symptoms, etc.) directly to care providers via Bluetooth or digital/broadband/wireless.36,38 Telemonitoring can be used to recognize and treat changes in the patient's health status as a stand-alone approach (e.g. early detection) or as part of a telerehabilitation intervention. This paper focuses on telemonitoring and telerehabilitation as types of telehealth that can support home-based PR and benefit patients with lung diseases or COVID-19. The purpose of this paper is to depict the use of telemonitoring and telerehabilitation interventions in patients with chronic lung diseases, such as asthma, chronic obstructive pulmonary diseases (COPD), or COVID-19 patients and their association with patient health outcomes. The objectives of this paper were to (1) identify which telemonitoring and telerehabilitation interventions (e.g. videoconferencing) are used to provide telehealth care for people with chronic respiratory conditions or COVID-19, and (2) provide an overview of the effects of telemonitoring and telerehabilitation on exercise capacity, physical activity, HRQoL, and healthcare use in patients with lung diseases or COVID-19.
Methods
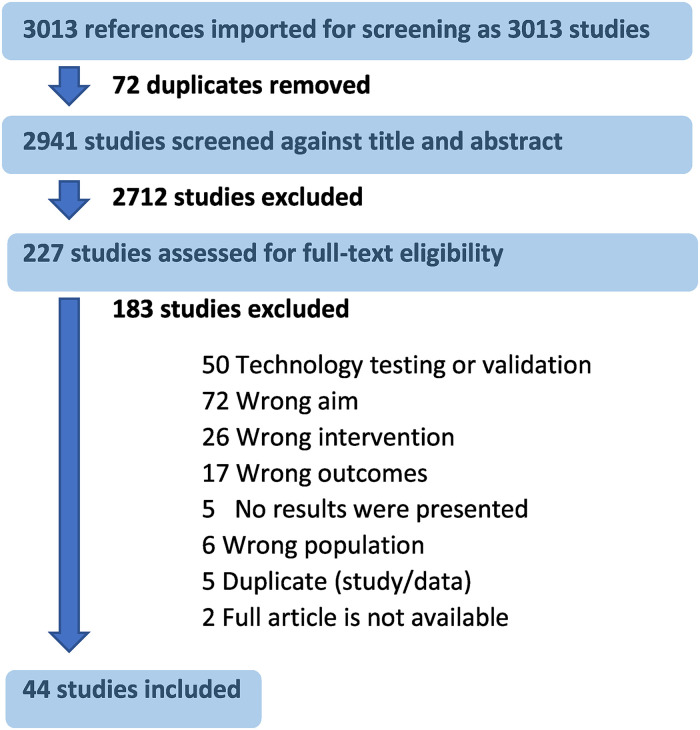
A health sciences librarian (HL), in consultation with the research team, developed and performed a search in the electronic databases of Ovid MEDLINE, EMBASE, and Cinahl through 15 June 2021. Subject heading and keywords were used to reflect the concepts of telemonitoring, telerehabilitation, chronic lung diseases, and COVID-19 (see supplement 1 for the OVID Medline search). The search was limited to full-text articles published in the English language with full text available. This scoping review of the literature, which has not been registered, was conducted using Preferred Items for Systematic Reviews and Meta-Analysis (PRISMA) (Figure 1). The search retrieved 3013 references. After removing the duplicates, two researchers screened 2941 titles and abstracts and read in full the text of 227 articles. Both researchers reviewed independently the articles and selected 44 publications that met the inclusion criteria of (1) the study explored the effect of a telerehabilitation and/or telemonitoring intervention, (2) in patients with a chronic lung diseases, such as asthma, COPD, or COVID-19 patients, (3) and reported the effect of the intervention in one or more of the following outcomes: exercise capacity, physical activity, HRQoL, or healthcare use. The main reasons for exclusion of the studies included: (1) the study aimed to validate a new technological component instead of evaluating an intervention, (2) the intervention was only teleconsultation or one-time assessment, or the effect of the intervention in one of the (3) populations or (4) outcomes of interest were not reported.
Fig. 1.
PRISMA—Literature selection process.
Data extraction and synthesis
Information from the 44 articles was summarized in Table 1, which presented: (1) author(s)’ name, (2) country of the study, (3) type of study, (4) intervention group and control group, (5) technology used in the study, (6) duration of the intervention, (7) participants’ condition, and (8) description of the study population. The effect of telemonitoring and telerehabilitation on physical activity, exercise capacity, health-related quality of life and healthcare use in patients with chronic lung diseases or COVID-19 was extracted and compiled in Tables 2–4.
Table 1.
Main characteristics of the studies included.
| Author Year Country |
Type of study | Intervention Group (IG) Control Group (CG) |
Technology | >1 Monitoring devices involved (Yes/no) | Duration of the intervention | Disease | Intervention group | Control group | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of participants | Age mean years (SD) | Males N (%) | Number of participants | Age Mean years (SD) | Males N (%) | |||||||
| Telemonitoring | ||||||||||||
| Antoniades, Nick 2012 39 | RCT | IG: Remote In-home monitoring (TeleMedCare) + standard best practice. CG: Standard best practice |
Laptop (software), daily monitoring spirometry, vital functions, oximetry, etc. | Yes | 12 Months | COPD | 22 | 70 (10) | 10 (83) | 22 | 68 (9) | 10 (83) |
| Australia | ||||||||||||
| Au, David 2015 40 | Matched group design (1:1) | IG: Telehealth system combined with care management program (Health Buddy Program) CG: Matched to similar baseline characteristics |
Four button Health Buddy device; asks for vital signs, disease symptoms, provides feedback, and categorizes patient's medical risk. | No | 3 Years | COPD | 619 | 75 (8) | 338 (55) | 619 | 74 (10) | 338 (55) |
| USA | ||||||||||||
| Boer, Lonneke 2019 41 | RCT | IG: Smart mobile health tool for self-management (mHealth tool). CG: Paper action plan |
Mobile phone (app), collected information on symptom changes and physiological measurements using a pulse oximeter, spirometer, and forehead thermometer. | Yes | 12 Months | COPD | 43 | 69 (8) | 25 (58) | 44 | 65 (8) | 29 (66) |
| Netherlands | ||||||||||||
| Chan, Debora 2007 42 | RCT | IG: Internet-based home monitoring and education. CG: Office-based care |
Home computer (website), camera and internet access. Digital video camera to capture patient's performance. | No | 52 Weeks | Asthma | 60 | 10 (3) | 38 (63) | 60 | 9 (3) | 37 (62) |
| USA | ||||||||||||
| Chau, Janita 2012 43 |
RCT | IG: Telecare service (ASTRI) + nurse home visit (education) CG: Only nurse home visit (education) |
Mobile phone, respiratory rate sensor, pulse oximeter. Internet and wireless systems, databases and software for critical decision analysis, and support. | Yes | 2 Months | COPD | 22 | 73 (6) | 21 (95) | 22 | 72 (6) | 18 (82) |
| Hong Kong | ||||||||||||
| Cushen, Brenda 2021 44 |
Pre-post | GI: Community virtual ward model (patient information transferred to hospital portal) | Bluetooth-enabled smartphone and hospital portal. Remote monitoring of daily oxygen saturations, heart rate, and spirometry measurements. | Yes | Mean 10 (4) days admission to discharge | COPD and/or asthma | 20 | 64 (13) | 7 (35) | N/A | N/A | N/A |
| Ireland | ||||||||||||
| de Jongste, Johan 2009 45 |
RCT | GI: Daily telemonitoring of exhaled nitric oxide + monitoring symptoms CG: Symptoms monitoring only |
PalmOne, airway inflammation monitor (NIOX MINO; Aerocrine, Solna, Sweden) that measures FENO0.05 | No | 30 Weeks | Asthma | 77 | 11 (2) | 46 (60) | 74 | 11 (4) | 54 (73) |
| Netherlands | ||||||||||||
| Deng, Ning 2020 46 |
Pre-post | GI: Mobile health technology to deliver a community-based closed-loop management system (app) | MHealth system: smartphone (patient app), workstation (doctor), a cloud server, and a simple peak flow meter. | No | 6 Months | COPD | 39 | 61 (6) | 36 (92) | N/A | N/A | N/A |
| China | ||||||||||||
| Ding, Hang 2014 47 |
Pre-post | GI: A mobile-phone-based home monitoring system (app) | Mobile phone to record COPD symptoms and vital signs on portal. Thermometer, pulse oximeter. | Yes | 6 Months | COPD | 10 | 65 (9) | 5 (50) | N/A | N/A | N/A |
| Australia | ||||||||||||
| Farias, Raquel 2019 48 |
Pre-post | GI: Phone interactive telesystem (computer-linked interactive phone telesystem) | Card (PIN) and the Telesystem contact information with automated phone call questions and a callback notification. | No | 12 Months | COPD | 256 | 70 (9) | 117 (46) | N/A | N/A | N/A |
| Canada | ||||||||||||
| Farmer, Andrew 2017 49 | RCT | GI: Digital health system (EDGE, Self-management, anD support prorGrammE). CG: Standard care |
EDGE platform, tablet, and Bluetooth-enabled oximeter. | No | 12 Months | COPD | 110 | 69 (9) | 68 (62) | 56 | 69 (10) | 34 (61) |
| UK | ||||||||||||
| Jódar-Sánchez, Francisco 2013 50 |
RCT | IG: Home telehealth program (Tele-Modem, Aerotel Medical Systems) CG: Usual care. |
Spirometer, a pulse oximeter, heart rate, blood pressure monitor (model UA-767 BT, A&D Company). Data sent via a hub (Tele-Modem, Aerotel Medical Systems) connected to the patient's home telephone line. | Yes | 4 Months | COPD | 24 | 74 (8) | 23 (96) | 21 | 71 (10) | 20 (95) |
| Spain | ||||||||||||
| Koff, Patricia 2021 51 |
Quasi-randomized clinical trial | IG: Proactive iCare (healthcare delivery model that couples integrated care with remote monitoring) CG: Usual care |
Health buddy, finger pulse oximeter, handheld spirometer and pedometer. | Yes | 9 Months | COPD | 352 | 68 (8) | 205 (58) | 159 | 68 (9) | 106 (67) |
| USA | ||||||||||||
| Lewis, Keir E 2010 52 | RCT | IG: Home telemonitoring (telemonitoring via the home telephone line) + standard care CG: Standard care |
Handheld telemonitor connected via telephone line, thermometer, and pulse oximeter probe connected to the monitor. | Yes | 6 Months | COPD | 20 | 70 (range 61–73) | 10 (50) | 20 | 73 (range 63–79) | 10 (50) |
| UK | ||||||||||||
| McDowell, Janet 2015 53 |
RCT | IG: Home-based healthcare with telemonitoring (telecommunications device connected directly to patient's phone line) CG: Usual care |
Home telehealth system (HomMed, Honeywell, USA) self-monitoring to record vital signs (finger probe and blood cuff) and answer questions. | Yes | 6 Months | COPD | 55 | 69 (7) | 32 (58) | 55 | 70 (7) | 30 (54) |
| Ireland | ||||||||||||
| Pare, Guy 2013 54 |
RCT | IG: Home telemonitoring (touchscreen, modem) CG: Regular home care visits. |
Touch screen with an integrated modem (TELUSTM) to send clinical data. | No | 21.5 Months | COPD | 60 | 67 (6) | 19 (32) | 60 | 68 (6) | 19 (32) |
| Canada | ||||||||||||
| Pedone, Claudio 2013 55 |
RCT | IG: Multiparametric telemonitoring of vital signs CG: Standard care |
Cellular telephone coupled with wristband containing Bluetooth sensors (heart rate, physical activity, body temperature, and a pulse-oximeter). | No | 9 Months | COPD | 50 | 74 (6) | 36 (72) | 49 | 75 (6) | 31 (63) |
| Italy | ||||||||||||
| Persson, Hans 2020 56 |
Cohort study | IG: Health Diary Telemonitoring and Hospital-Based Home Care (HBCH). | Digital pen and a Health Diary paper form to report daily health status. | No | 12 Months | COPD | 36 | 75 (6) | 14 (39) | NA | NA | NA |
| Sweden | ||||||||||||
| Pinnock, Hilary 2013 57 | RCT | IG: Touch screen telemonitoring equipment + clinical care. CG: Clinical care. |
Touchscreen Telemonitoring equipment to record and transmit daily questionnaires and monitor oxygen. Algorithms alerts. | No | 12 Months | COPD | 128 | 69 (8) | 53 (41) | 128 | 68 (8) | 63 (49) |
| UK | ||||||||||||
| Rasmussen, Linda 2005 58 |
RCT (3 groups) |
IG: Internet-based monitoring asthma tool. CG1: Asthma specialist treatment CG2: General practitioner treatment |
Internet diary or push-button phone. Peak flowmeter (Vitalograph, Ltd, Maid Moriton, Buckingham, United Kingdom). | No | 6 Months | Asthma | 85 | 28 (range 14–44) | 27 (32) | CG1: 88 CG2:80 |
CG1: 30 (range 19–45) CG2:30 (range 20–45) |
CG1: 30 (34) CG2: 30 (38) |
| Denmark | ||||||||||||
| Schou, Lone 2013 59 | RCT | GI: telemedicine-based treatment (videoconferencing system-daily ward rounds) CG: conventional hospital admission |
Touch screen PC and additional devices (pulse oximeter, spirometer, and thermometer) for monitoring the vital signs. | No | 3 Months | COPD | 22 | 68 (12) | 10 (45) | 22 | 73 (10) | 8 (36) |
| Denmark | ||||||||||||
| Stamenova, Vess 2020 60 |
RCT (3 arms) | IG: Technology -Enabled remote monitoring program. CG1: Technology-Enabled Self-Management (web-based) CG2: Standard care |
Web-based portal and Bluetooth devices: custom tablet computer pulse wave wrist cuff monitor, oximeter, weighing scale, and thermometer. | Yes | 6 Months | COPD | 41 | 71 (9) | 23 (56) | CG1: 41 CG: 40 |
CG1: 71 (7) CG2: 72 (9) |
CG1: 23 (56) CG2: 21 (52) |
| Canada | ||||||||||||
| van Gaalen, Johanna 2013 61 |
RCT (multicenter nonblinded, pragmatic randomized controlled parallel trial) | IG: Internet-based self-management support. CG: Usual care. |
Website platform. Handheld spirometer and reporting symptom score. | No | 30 Months | Asthma | 47 | 36 (8) | 12 (26) | 60 | 37 (8) | 19 (32) |
| Netherlands | ||||||||||||
| Vianello, Andrea 2016 62 | RCT | IG: Home telemonitoring (Gateway device for data transmission over telephone) CG: Usual care |
TM system: finger pulse-oximeter and a gateway device for data transmission over a telephone line to a central data management unit located at the Veneto Regional e-Health Centre. | No | 12 Months | COPD | 230 | 75 (6) | 164 (71) | 104 | 76 (6) | 76 (73) |
| Italy | ||||||||||||
| Zairina, Elida 2015 63 | RCT | IG: Telehealth program CG: Usual care |
Mobile application Breathe-easy© supported by a Bluetooth-enabled handheld device (COPD-6 R), which was used for self-monitoring of lung function. | No | 6 Months | Asthma | 36 | 31 (4) | 0 | 36 | 31 (4) | 0 |
| Australia | ||||||||||||
| Telerehabilitation | ||||||||||||
| Bermejo-Gil, Beatriz 2021 64 | Pre-post | IG: Home-based telerehabilitation system (RespiraCon Nosotros) | Web application for respiratory exercises and chat function for interaction compatible with computer, tablet, television, and mobile. | No | 1 Month | COVID-19 | 15 | range 28–38 | 8 (53) | NA | NA | NA |
| Spain | ||||||||||||
| Burkow, Tatjana 2015 65 | Pre-post | IG: PR in home-based online groups (videoconference) | Internet-based comprehensive, multidisciplinary pulmonary rehabilitation program + step counter. | No | 9 Weeks | COPD | 10 | 61 (range 46–72) | 5 (50) | N/A | N/A | N/A |
| Norway | ||||||||||||
| Hansen, Henrik 2020 66 |
RCT | IG: Pulmonary Telerehabilitation program (videoconference). CG: Conventional PR program |
Videoconference software system installed on a single touch screen. | No | 10 Weeks | COPD | 67 | 68 (8) | 32 (48) | 67 | 68 (9) | 28 (42) |
| Denmark | ||||||||||||
| Yuyu 2020 67 | RCT | IG: Pulmonary internet explorer Rehabilitation (PeR) program based on social media (WeChat) CG: Face-to-face PR rehabilitation |
PeR includes two ports: the computer end and the WeChat end. | No | 3 Months | COPD | 53 | 70 (6) | 44 (83) | 53 | 71 (7) | 43 (81) |
| China | ||||||||||||
| Jiménez-Reguera, Begoña 2020 68 |
RCT | IG: mHealth Web-Based platform (HappyAir) CG: Hospital scheduled evaluations. |
HappyAir app: educational program and data collection related to physical activity and disease, recording medication intake, daily exercise time (minutes), level of tiredness and daily mood. | No | 12 Months | COPD | 20 | 68 (6) | 9 (41) | 24 | 68 (7) | 13 (59) |
| Spain | ||||||||||||
| Lewis, Adam 2021 69 | pre-post | IG: Online platform delivery of PR | E-learn Moodle platform (videoconference, messaging) | No | 6 Weeks | COPD | 17 | 69 (10) | 8 (47) | NA | NA | NA |
| UK | ||||||||||||
| Stickland, Michael 2011 70 | RCT | IG: PR delivered via Telehealth CG: PR delivered in person (standard outpatient hospital-based program) |
Videoconference | No | 8 Weeks | COPD | 147 | 69 (8) | 78 (53) | 262 | 69 (9) | 125 (44) |
| Canada | ||||||||||||
| Telemonitoring and telerehabilitation | ||||||||||||
| Benzo, Roberto 2021 71 | RCT | IG: Home-based program with video-guided exercises (website) + phone call health coaching* CG: Waiting list 8 weeks and the intervention was offered afterwards |
Computer tablet: video-guided exercises using an oximeter, an activity monitor and daily self-report of symptoms. | Yes | 8 Weeks | COPD | 72 | 69 (8) | 34 (47) | 74 | 68 (9) | 37 (50) |
| USA | ||||||||||||
| Bhatt, Surya 2019 72 | Matched group design (1:2) | IG: Telehealth PR (video conference) * CG: Contemporaneous subjects who had been hospitalized for a COPD exacerbation but did not receive the intervention |
Smartphone with video capabilities to facilitate two-way live videoconferencing. Automatic sphygmomanometers (blood pressure), and a pulse oximeter (heart rate and oxygen saturation). | Yes | 12 Weeks | COPD | 80 | 64 (10) | 49 (61) | 160 | 63 (11) | 92 (57) |
| USA | ||||||||||||
| Broadbent, Elizabeth 2018 73 |
RCT | IG: iRobi robot (monitor health and prompt medical contact) CG: Standard care |
Robot with Wi-Fi linked smart inhalers: (1) Measure pulse oximetry, forced expiration volume, heart rate, and symptoms, mental state, and functional status using the Clinical COPD Questionnaire (2) reminding medication and inhalers and record their adherence several times a day; (3) remind rehabilitation exercises (4) provide education about COPD; (5) I am feeling unwell function (6) trends over time health status and adherence. | No | 4 Months | COPD | 30 | 70 (10) | 11 (37) | 30 | 69 (9) | 12 (40) |
| New Zealand | ||||||||||||
| Galdiz, Juan 2021 74 |
RCT | IG: Pulmonary Telerehabilitation program (web-based platform) CG: Standard care |
Web-based platform, and a telerehabilitation kit (mobile phone, pulse oximeter, dumbbells and exercise bicycle). | No | 12 Months | COPD | 46 | 62 (8) | 30 (65) | 48 | 63 (6) | 33 (68) |
| Spain | ||||||||||||
| Gilmutdinova, Ilmira R 2021 75 |
pre-post | IG: Telemedicine platform (COVIDREHAB) | A mobile phone, tablet or computer, an Internet connection and an e-mail address on this device. Platform: information and analytical system for remote monitoring of medical rehabilitation. | No | 2 Weeks | COVID-19 | 178 | 50 (range 32–82) | 70 (39) | NA | NA | NA |
| Russia | ||||||||||||
| Holland, Anne 2013 76 | Pre-post | IG: Telerehabilitation (video collaborative software) | A tablet computer was used for videoconferencing. A pulse oximeter (oxyhemoglobin saturation and heart rate). | No | 8 Weeks | COPD | 8 | 66 (range 56–83) | 3 (38%) | NA | NA | NA |
| Australia | ||||||||||||
| Marquis, Nicole 2015 77 | Pre-post | IG: In-home PR (video conferencing system) | Videoconferencing system, internet connection with encrypted transmission. Wireless oximeter (oxygen saturation and heart rate). | Yes | 6 Months | COPD | 23 | 65 (7.1) | 8 (35) | NA | NA | NA |
| Canada | ||||||||||||
| Paneroni, Mara 2015 78 |
controlled, non-randomized pilot study | IG: Telerehabilitation (satellite platform) CG: Standard outpatient rehabilitation program |
Home telemonitoring platform, medical devices (oximeter, steps counter) | Yes | 40 Days | COPD | 18 | 6 5(10) | 16 (89) | 18 | 66 (6) | 15 (83) |
| Italy | ||||||||||||
| Rassouli, Frank 2018 79 |
Observational (pre-post) | IG: Digital multidisciplinary PR (App) | Multiplatform smartphone application with exercise videos. Pedometer. | No | 20 Days | COPD | 34 | 59 (8) | 8 (24) | NA | NA | NA |
| Switzerland, Austria, and Germany | ||||||||||||
| Ringbaek, Thomas 2015 80 |
RCT | IG: Telehealth care (telemonitoring equipment) with the option of video consultation CG: Usual care |
Tablet computer with a web camera, a microphone, and measurement equipment (spirometer, pulse oximeter, and bathroom scale). | Yes | 6 Months | COPD | 141 | 69 (9) | 55 (39) | 140 | 69 (10) | 76 (54) |
| Denmark | ||||||||||||
| Tsai, Ling 2017 81 |
RCT | IG: Home-based telerehabilitation (videoconferencing) CG: Usual care without exercise training |
Computer with an in-built camera, and a finger-tip pulse oximeter. | Yes | 8 Weeks | COPD | 19 | 73 (8) | 12 (63) | 17 | 75 (9) | 6 (86) |
| Australia | ||||||||||||
| Vitacca, Michele 2009 82 |
RCT | IG: Tele-assistance program (modem system through telephone line) CG: Standard care |
Pulse oximetry device with solid memory card + modem telephone. | No | 12 Months | COPD | 57 | 61 (7) | NR | 44 | 61 (17) | NR |
| Italy | ||||||||||||
SD: standard deviation; PR: pulmonary rehabilitation; SBP: standard best practice; N/A: not applicable; NR: not reported.
Table 2.
Effect of telemonitoring and/or telerehabilitation on physical activity and exercise capacity in patients with lung diseases or COVID-19.
| Disease | Study | Exercise capacity | Physical activity | |||||
|---|---|---|---|---|---|---|---|---|
| IG change from pre-intervention | IG effect in comparison with CG | Instrument/tool used to assess the outcome | IG change from baseline | IG effect in comparison with CG | Instrument/tool used to assess the outcome | |||
| Telemonitoring | COPD | Koff, P. 2021 51 | ↑ | ↑ | 6MWT | |||
| Telerehabilitation | COVID-19 | Bermejo-Gil, B. 2021 64 | ↑ | NA | Borg scale | |||
| COPD | Hansen, Henrik 2020 66 | ↑ | = | 6MWT, 30 s sit-to stand test | no | = | Triaxial accelerometer | |
| Stickland, M. 2011 70 | ↑ | = | 12 min walk test | |||||
| Lewis, A. 2021 69 | ↑ | NA | 1 min sit-to stand test | |||||
| Jiménez-Reguera, B. 2020 68 | no | = | 6MWT | |||||
| Telerehabilitation and telemonitoring | COPD | Benzo, R. 2021 71 | NR | = | ActiGraph | |||
| Tsai, L. 2017 81 | ↑ | ↑ | Endurance shuttle walk test | no | = | Triaxial accelerometer | ||
| ↑ | = | 6MWT | ||||||
| Paneroni, M. 2015 78 | ↑ | = | 6MWT | |||||
| Holland, A. 2013 76 | ↑ | NA | 6MWT | |||||
| Marquis, N. 2015 77 | ↑ | NA | 6MWT | |||||
| Galdiz, J. 2020 74 | no | = | 6MWT | |||||
IG: Intervention group; CG: control group; 6MWT: 6-min walking test NA: not applicable. ↑: significantly better outcome; =: no significant difference in outcome change between groups. not reported. NR: data and/or significance level not reported.
Table 3.
Effect of telemonitoring and/or telerehabilitation on health-related quality of life and/or health status in patients with lung diseases or COVID-19.
| Disease | Study | Health-related quality of life (HRQoL) and/or health status | |||
|---|---|---|---|---|---|
| IG change from pre-intervention | IG effect in comparison with CG | Instrument/tool used to assess the outcome | |||
| Telemonitoring | Asthma | Rasmussen, L. 2005 58 | ↑ | ↑ (than the 2 CGs) | Asthma-related quality of life (AQLQ) |
| van Gaalen, J. 2013 61 | ↑ | ↑ | AQLQ | ||
| Zairina, E. 2015 63 | ↑ | ↑ | mAQLQ (mini asthma quality of life questionnaire) | ||
| de Jongste, J. 2009 45 | ↑ | = | Pediatric asthma caregiver quality of life questionnaire (PACQLQ) | ||
| Chan, D. 2007 42 | ↑ | NR | Pediatric asthma quality of life questionnaires (PAQLQ) applied to caregiver | ||
| COPD and/or asthma | Cushen, B. 2021 44 | no | NA | EQ-VAS questionnaire | |
| COPD | Koff, P. 2021 51 | ↑ | ↑ | SGRQ | |
| Farmer, A. 2017 49 | ↑ | ↑ | EQ-5D-5L questionnaire | ||
| ↑ | = | SGRQ | |||
| Stamenova, V. 2020 60 | ↑ | = (in the 3 groups) | SGRQ | ||
| Deng, N. 2020 46 | ↑ | NA | COPD assessment test (CAT) | ||
| Antoniades, N. 2012 39 | no | = | Chronic respiratory disease questionnaire (CRDQ), 36-Item short from survey (SF-36) | ||
| Persson, H. 2020 56 | no | NA | SGRQ | ||
| McDowell, J. 2015 53 | NR | ↑ | SGRQ | ||
| = | EQ-5D questionnaire | ||||
| Boer, L. 2019 41 | NR | = | EQ-5D questionnaire, Nijmegen clinical screening instrument (NSCI), Clinical COPD Questionnaire (CCQ) | ||
| Chau, J. 2012 43 | NR | = | Chronic respiratory questionnaire (CRQ) | ||
| Jódar-Sánchez, F. 2013 50 | NR | = | SGRQ, EuroQoL-5D questionnaire | ||
| Lewis, K. 2010 69 | NR | = | SGRQ, and EuroQoL EQ-5D questionnaire | ||
| Pinnock, H. 2013 57 | NR | = | SGRQ | ||
| Schou, L. 2013 59 | NR | = | SGRQ | ||
| Vianello, A. 2016 62 | NR | = | SF-36 | ||
| Telerehabilitation | COPD | Stickland, M. 2011 70 | ↑ | = | SGRQ |
| Burkow, T. 2015 65 | ↑ | NA | SGRQ | ||
| Lewis, A. 2021 69 | ↑ | NA | CRQ | ||
| Rassouli, F. 2018 79 | ↑ | NA | CAT, CRQ | ||
| Jiang, Y. 2020 67 | ↑ | = | CAT, SGRQ | ||
| Jiménez-Reguera, B. 2020 68 | ↑ | = | SGRQ | ||
| no | = | CAT, EuroQOL-5D questionnaire | |||
| Hansen, H. 2020 66 | ↑ | = | Clinical COPD Questionnaire (CCQ) | ||
| no | = | EQ-5D-VAS | |||
| Telerehabilitation and telemonitoring | COVID-19 | Gilmutdinova, I. 2021 75 | ↑ | NA | Survey (Overall well-being improved in 83% of the participants) |
| COPD | Holland, A. 2013 76 | ↑ | NA | CRQ | |
| Marquis, N. 2015 77 | ↑ | NA | CRQ | ||
| Paneroni, M. 2015 78 | ↑ | = | SGRQ | ||
| Tsai, L. 2017 81 | ↑ | = | CAT | ||
| no | = | CRDQ (Chronic respiratory disease Questionnaire) | |||
| Benzo, R. 2021 71 | NR | = | CRQ | ||
| Broadbent, E. 2018 73 | NR | = | CCQ | ||
| Galdiz, J. 2020 74 | no | = | SF-36, Chronic respiratory disease Questionnaire (CRQ) | ||
IG: Intervention group; CG: control group. NA: not applicable. EQ-VAS: EuroQol-visual analogue scales; CAT: COPD assessment test; SGRQ: St George's Respiratory Questionnaire; CRQ: chronic respiratory disease questionnaire; ↑: significantly better outcome; =: no significant difference in outcome change between groups. NR: data and/or significance level not reported.
Table 4.
Effect of telemonitoring and/or telerehabilitation on healthcare use in patients with lung diseases.
| Disease | Study | Healthcare use | |||
|---|---|---|---|---|---|
| IG change from pre-intervention | IG effect in comparison with CG | Instrument/tool used to assess the outcome | |||
| Telemonitoring | Asthma | Chan, D. 2007 42 | NR | = | Number of ED visits, hospitalizations, unscheduled asthma-related visits. |
| Zairina, E. 2015 63 | NR | = | Number of unscheduled health-care visits. | ||
| COPD | Koff, P. 2021 51 | ↓ | ↓ | COPD-related urgent office GP visits (decreased only on IG). | |
| ↓ | = | COPD-related hospitalizations, hospital LOS, ED visits, ICU hospitalization. | |||
| no | = | Non-COPD urgent office GP visits, hospitalizations, hospital LOS, ED visits, ICU hospitalizations. | |||
| Ding, H. 2014 47 | ↓ | NA | Hospital admissions, ED presentations, and GP visits. | ||
| Farias, R. 2019 48 | ↓ | NA | Respiratory-related ER visits, and COPD-related hospitalizations. | ||
| Au, D. 2015 40 | NR | ↓ | Quarterly all-cause hospital admissions, respiratory-related hospital admissions. | ||
| Pare, G. 2013 54 | NR | ↓ | Number of hospitalization days and visits to ER. | ||
| Pedone, C. 2013 55 | NR | ↓ | COPD-related hospitalizations. | ||
| Farmer, A. 2017 49 | NR | ↓ | Visits to the GP practice nurses. | ||
| NR | = | Relative risk of hospital admission. | |||
| Vianello, A. 2016 62 | NR | ↓ | Readmission rate AECOPD and/or for any cause, appointment with a pulmonary specialist. | ||
| NR | = | Hospitalization rate for AECOPD (acute exacerbations of COPD) and/or for any cause. | |||
| Antoniades, N. 2012 39 | NR | = | Number of COPD-admission/year, COPD-related length of stay (LOS) days/year, total admission/year, total LOS days/year. | ||
| Boer, L. 2019 41 | NR | = | Exacerbation-related hospital admissions, unscheduled respiratory-related healthcare consultations. | ||
| Chau, J. 2012 43 | NR | = | Number of emergency department visits and hospital re-admissions. | ||
| Jódar- Sánchez, F. 2013 50 | NR | = | ED visits, specialized consultations, hospitalizations. | ||
| McDowell, J. 2015 53 | NR | = | Number of ED visits, hospitalizations, or contacts with GP. | ||
| Pinnock, H. 2013 57 | NR | = | Hospital admissions due to COPD or all cause, duration of hospital admission. | ||
| Stamenova, V. 2020 60 | NR | = | Hospitalizations, ED visits, or clinic visits. | ||
| Telerehabilitation | COPD | Hansen, H. 2020 66 | NR | = | Hospital admission related to COPD exacerbations; all causes of hospitalization. |
| Telerehabilitation and Telemonitoring | COPD | Bhatt, S. 2019 72 | NR | ↓ | 30-day all-cause readmission and AECOPD (acute exacerbation of COPD) readmission. |
| Vitacca, M. 2009 82 | NR | ↓ | Hospitalizations, ER admissions and urgent GP calls. | ||
| Ringbaek, T. 2015 80 | NR NR | ↓ | Visits to the respiratory outpatient clinic. | ||
| = | Number of hospital admissions (for COPD or all causes), time to first admission, length of stay, visit to ER. | ||||
| Broadbent, E. 2018 73 | NR | = | Hospitalizations for respiratory problems, total number of days in hospital for respiratory problems. | ||
IG: Intervention group; CG: control group. ED: emergency department; ER: emergency room; GP: general practitioner; ↓ significantly lower; = no significant difference between groups. NA: not applicable. NR: data and/or significance level not reported.
Results
All 44 manuscripts were original research published between 2005 and 2021. The studies were conducted in Australia (5), Canada (5), USA (5), Denmark (4), Italy (4), Spain (4), UK (4), China (3), the Netherlands (3), Ireland (2), New Zeeland (1), Norway (1), Russia (1), Sweden (1), and 1 study in Austria, Germany, and Switzerland. The main characteristics of the included studies are presented in Table 1. Twenty-eight manuscripts reported on randomized controlled studies, 11 pre-post intervention studies, 2 matched population studies, 1 controlled non-randomized study, 1 quasi-randomized clinical trial, and 1 cohort study. Follow-up periods reported range between 10 days and 36 months. The number of participants involved in intervention groups of the studies ranged between 8 and 619 (median: 45). Thirty-five of the studies were conducted in patients with COPD, 5 in patients with asthma, 1 included patients with COPD and/or asthma, and 2 in patients with COVID-19. Two studies were conducted on children and the rest on adult patients (Table 1).
Interventions and technology
Table 1 describes the details of the interventions and the technology used. The effect of telemonitoring (25 studies), telerehabilitation (8 studies) or both interventions combined (11 studies) were reported on the physical activity, exercise capacity, HRQoL and healthcare use of patients with respiratory diseases or COVID-19. These technology-enabled remote interventions were implemented as a stand-alone approach or in combination with other elements (e.g. standard care). Twenty-seven of the studies involved mobile apps, web pages, or virtual platforms accessed using a laptop, tablet or smartphone.39,41–44,46,47,49,55,59–61,63–69,71,72,74–76,79–81 In two studies the intervention was delivered using a teleconference platform,66,76 and one social platform. 67 Other transmitting devices/systems used in the studies included the health buddy device,40,51 the iRobi robot, 73 a PalmOne, 45 touch screen telemonitoring equipment, 57 a home health system connected to a phone line, 53 a computer-linked interactive phone tele-system, 48 a tele-modem,50,54,62,82 a satellite platform, 83 computer or push-bottom telephone, 58 handheld monitor connected to a phone line, 52 a digital pen and health dairy paper together with SMS. 56 Portable devices used to monitor patients’ remotely included pulse oximeters (oxygen saturation and heart rate), spirometers (lung function), and accelerometers (physical activity) among others. Sixteen studies used more than one device to collect patient data. Information from the monitoring devices was collected using Bluetooth technology, manually entered, or verbally reported by participants to the research team or healthcare providers.
Exercise capacity and physical activity
A significant improvement in exercise capacity was reported in COVID-19 patients who received home-based telerehabilitation 64 (Table 2). Increased baseline exercise capacity was also found in COPD patients who received telemonitoring, 51 telerehabilitation (3 of 4 studies),66,69,70 or a combination of both.76–78,81 However, only one study that explored the effect of telemonitoring 51 and another that combined telemonitoring and telerehabilitation 81 found greater improvement in exercise capacity in intervention groups compared to controls. Telerehabilitation76–78,81 alone or in combination with telemonitoring was not associated with changes in physical activity compared to control groups among COPD patients.66,71,81
HRQoL and/or health status
Overall well-being improved in 83% of COVID-19 patients who participated in an intervention involving telerehabilitation and telemonitoring 75 (Table 3). Telemonitoring interventions were associated with an improvement in HRQoL in patients with asthma42,45,58,61,63 and COPD (4 of 6 studies),46,49,51,60 and no changes in HRQoL were identified in one study that included both asthma and COPD patients combined. 44 Nevertheless, when compared to control groups, telemonitoring was associated with a greater improvement in HRQoL only in 75% (3 of 4) of studies in asthma patients46,49,51,58,60,61,63 and in 23% (3 of 13) of studies in COPD patients.49,51,53 Telerehabilitation65–70,79 alone and the combination of telerehabilitation with telemonitoring76–78,81 were associated with improvement in HRQoL in COPD patients. However, no significant difference in HRQoL change was found between the intervention groups and controls.66–68,70,71,73,74,78,81
Healthcare use
A decrease in pre-intervention hospital admissions, length of hospitalization, and visits to the emergency department and GP's office were reported in COPD patients who participated in telemonitoring interventions.47,48,51 Furthermore, 6 out of 13 studies reported fewer urgent visits to GP's office, 51 fewer visits to the pulmonary specialist 62 and nurse practitioner, 49 fewer hospital admissions,40,55 and readmissions, 62 fewer days of hospitalization, and fewer ER visits 54 in patients with COPD who received telemonitoring compared to control groups. However, 7 of 13 studies found no significant difference in health care use between controls and patients with COPD,39,41,43,50,53,57,60 who participate in telemonitoring interventions, and the same was reported in two studies among patients with asthma.42,63 No significant differences were found in COPD exacerbation-related hospital admission or in all causes of hospitalization between COPD participants of a telerehabilitation program compared with a conventional pulmonary rehabilitation (PR) program. 66 Three of 4 studies reported lower use of healthcare in COPD patients who participated in interventions combining telerehabilitation and telemonitoring compared with control groups.72,80,82
Discussion
This paper aimed at portraying the use of telemonitoring and telerehabilitation in patients with chronic lung diseases such as asthma, COPD or COVID-19 patients and the effects of these modalities of intervention on physical activity, exercise capacity, health-related quality of life and healthcare use. A scoping review methodology was followed to explore the literature in the field. 27.3% of the studies retrieved were published after 2020 demonstrating the expanding need for technology in PR, especially after the rise of COVID-19. The first objective was to identify the telemonitoring and telerehabilitation interventions that are used to provide telehealth care for people with chronic respiratory conditions or COVID-19. The literature review identified various technologies and technology-based approaches used to provide telemonitoring and/or telerehabilitation interventions for patients with asthma, COPD, or COVID-19. The technologies used were classified into two types. The first type included portable and mobile technologies to capture physiological and other-non-invasive variables measured by patients themselves at home (e.g. heart rate, oxygen saturation) and the second type included information and communication technologies that allow seamless transfer of health data from the remote location to the healthcare provider. Overall, technologies were diverse, involved various levels of complexity, and were deployed in specific ways depending on the cases used. As such, we have classified the interventions into telemonitoring where only the surveillance of physiological and other non-invasive variables was needed, telerehabilitation where a PR or exercise intervention was administered remotely, or a combination of both.
The second objective of this paper was to provide an overview of the effects of telemonitoring and telerehabilitation on exercise capacity, physical activity, HRQoL, and healthcare use in patients with lung diseases or COVID-19. Results indicated that telemonitoring and telerehabilitation were associated with an improvement in exercise capacity, higher HRQoL, and lower healthcare use in these patients. Furthermore, these interventions produced outcomes comparable to standard care, which aligns with previous evidence that reported similar benefits of telerehabilitation to traditional in-person outpatient PR programs.84,85 Previous evidence has also suggested that telemonitoring interventions can contribute to better disease management, higher patient empowerment, higher patient engagement and satisfaction, facilitate communication between the patient and healthcare team, and facilitate data collection and data access in patients with COPD. 86 Some potential barriers associated with these interventions included heterogeneity of care, lack of patient comfort with technology, patient resistance, time-consuming, increased workload for healthcare providers and staff shortages. 86 From the cost-effective perspective, evidence suggested that although technology-based interventions require an initial financial investment, they will substantially reduce costs in the long-term, potentially due to a reduction in healthcare use and travel costs. 87
Overall, evidence suggested that telemonitoring and telerehabilitation are potentially valuable mechanisms to improve patient care and access, especially in rural areas, 88 and do not increase mortality rates. 89 Therefore, policy and decision-makers should consider supporting the implementation of telemonitoring and telerehabilitation interventions by providing an initial investment associated with the cost of the equipment, regulating the practice of telerehabilitation including protected time for healthcare providers, and involving in-institution information and technology services to support data transmission and enable secure remote sessions.90,91 Future studies should explore mechanisms to reduce potential barriers associated with the use of technology-based interventions, such as lack of standardization and cost-effectiveness analyses.
Strengths and limitations
The results of this study contribute to filling a significant knowledge gap about the value of telemonitoring and telerehabilitation in the management of patients with chronic lung diseases or COVID-19. This knowledge is needed among the first priorities identified by the patients and clinicians after COVID-19 widely affected the delivery of rehabilitation services.92,93 63.6% of the retrieved manuscript reported on randomized controlled trials demonstrating the current need for evidence about the effectiveness of telemonitoring and telerehabilitation in patients with chronic lung diseases or COVID-19. This paper presented the evidence available as of June 2021. The generalizability of the results of this study may be influenced by the higher variability between the characteristics of the studies included such as the number and age of the patients, outcome measurements, length of the intervention, technological components involved, and additional elements included (e.g. education components, type and numbers of healthcare providers involved, etc.). Due to this heterogeneity, authors suggested a cautious interpretation of the results and compiled the studies characteristics in Table 1 to facilitate the readers’ interpretation.
Conclusion
Telemonitoring and telerehabilitation interventions had a positive effect on patient exercise capacity and HRQoL and are associated with fewer healthcare use in patients with chronic lung diseases such as asthma, COPD, or post COVID-19. Furthermore, the results indicated that the outcomes of these interventions are comparable to standard care. Therefore, they are promising alternatives to support remote home-based rehabilitation in this group of patients that should be supported by policy and decision-making.
Supplemental Material
Supplemental material, sj-docx-1-jtt-10.1177_1357633X221122124 for Effect of telemonitoring and telerehabilitation on physical activity, exercise capacity, health-related quality of life and healthcare use in patients with chronic lung diseases or COVID-19: A scoping review by Diana C Sanchez-Ramirez, Margriet Pol, Hal Loewen, and Mohamed-Amine Choukou in Journal of Telemedicine and Telecare
Acknowledgements
The authors would like to thank Yang Zhaoyun, Rachel Adodo, and Amarzish Qadeer for their contribution to article screening and data extraction.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This work was supported by the start-up funds provided to Dr Sanchez-Ramirez by the University of Manitoba.
ORCID iDs: Diana C Sanchez-Ramirez https://orcid.org/0000-0003-1637-4309
Hal Loewen https://orcid.org/0000-0003-3621-1304
Mohamed-Amine Choukou https://orcid.org/0000-0001-9477-2412
References
- 1.Forum of International Respiratory Societies. The Global Impact of Respiratory Disease-Second Edition Sheffield: European Respiratory Society; 2017 [Available from: Available from: https://www.who.int/gard/publications/The_Global_Impact_of_Respiratory_Disease.pdf.
- 2.Johns Hopkins University of Medicine. COVID-19 Case Tracker. 2022 [Available from: Available from: https://coronavirus.jhu.edu/.
- 3.Hodgson CL, Higgins AM, Bailey MJ, et al. The impact of COVID-19 critical illness on new disability, functional outcomes and return to work at 6 months: A prospective cohort study. Crit Care 2021; 25: 382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanchez-Ramirez DC, Normand K, Zhaoyun Yet al. et al. Long-term impact of COVID-19: A systematic review of the literature and meta-analysis. Biomedicines 2021; 9: 900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiBonaventura M, Paulose-Ram R, Su J, et al. The burden of chronic obstructive pulmonary disease among employed adults. Int J Chron Obstruct Pulmon Dis 2012; 7: 211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alghamdi F, Ashour A, Adeyemi L, et al. The psychological impacts of COVID-19 pandemic among emerging adults: An observational cross-sectional study. Int J Environ Res Public Health 2022; 19: 1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corlade-Andrei M, Măirean C, Nedelea Pet al. et al. Burnout syndrome among staff at an emergency department during the COVID-19 pandemic. Healthcare 2022; 10: 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mapel DW, Dutro MP, Marton JPet al. et al. Identifying and characterizing COPD patients in US managed care. A retrospective, cross-sectional analysis of administrative claims data. BMC Health Serv Res 2011; 11: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mulpuru S, McKay J, Ronksley PEet al. et al. Factors contributing to high-cost hospital care for patients with COPD. Int J Chron Obstruct Pulmon Dis 2017; 12: 989–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NHLBI. National Heart, Lung, and Blood Institute/Pulmonary Rehabilitation [Available from: https://www.nhlbi.nih.gov/health-topics/pulmonary-rehabilitation.
- 11.Sanchez-Ramirez DC. Impact of pulmonary rehabilitation services in patients with different lung diseases. J Clin Med 2022; 11: 407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang H, Hu D, Xu Yet al. et al. Effect of pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis of randomized controlled trials. Ann Med 2022; 54: 262–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siddiq MAB, Rathore FA, Clegg Det al. et al. Pulmonary rehabilitation in COVID-19 patients: A scoping review of current practice and its application during the pandemic. Turk J Phys Med Rehabil 2020; 66: 480–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corhay JL, Dang DN, Van Cauwenberge Het al. et al. Pulmonary rehabilitation and COPD: providing patients a good environment for optimizing therapy. Int J Chron Obstruct Pulmon Dis 2014; 9: 27–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lahham A, Holland AE. The need for expanding pulmonary rehabilitation services. Life (Basel) 2021; 11: 1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Milner SC, Boruff JT, Beaurepaire Cet al. et al. Rate of, and barriers and enablers to, pulmonary rehabilitation referral in COPD: A systematic scoping review. Respir Med 2018; 137: 103–114. [DOI] [PubMed] [Google Scholar]
- 17.Fischer MJ, Scharloo M, Abbink JJ, et al. Drop-out and attendance in pulmonary rehabilitation: The role of clinical and psychosocial variables. Respir Med 2009; 103: 1564–1571. [DOI] [PubMed] [Google Scholar]
- 18.Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis 2011; 8: 89–99. [DOI] [PubMed] [Google Scholar]
- 19.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013; 188: e13–e64. [DOI] [PubMed] [Google Scholar]
- 20.Holland AE, Mahal A, Hill CJ, et al. Home-based rehabilitation for COPD using minimal resources: A randomised, controlled equivalence trial. Thorax 2017; 72: 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu XL, Tan JY, Wang T, et al. Effectiveness of home-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: A meta-analysis of randomized controlled trials. Rehabil Nurs 2014; 39: 36–59. [DOI] [PubMed] [Google Scholar]
- 22.Rochester CL, Vogiatzis I, Holland AE, et al. An official American Thoracic Society/European Respiratory Society policy statement: Enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med 2015; 192: 1373–1386. [DOI] [PubMed] [Google Scholar]
- 23.Vitacca M, Montini A, Comini L. How will telemedicine change clinical practice in chronic obstructive pulmonary disease? Ther Adv Respir Dis 2018; 12: 1753465818754778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bjoernshave B, Korsgaard J, Nielsen CV. Does pulmonary rehabilitation work in clinical practice? A review on selection and dropout in randomized controlled trials on pulmonary rehabilitation. Clin Epidemiol 2010; 2: 73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bjoernshave B, Korsgaard J, Jensen Cet al. et al. Participation in pulmonary rehabilitation in routine clinical practice. Clin Respir J 2011; 5: 235–244. [DOI] [PubMed] [Google Scholar]
- 26.Maeder A. Telehealth and remote access. Stud Health Technol Inform 2010; 151: 239–254. [PubMed] [Google Scholar]
- 27.Murray E. Internet-delivered treatments for long-term conditions: Strategies, efficiency and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res 2008; 8: 261–272. [DOI] [PubMed] [Google Scholar]
- 28.Polisena J, Tran K, Cimon K, et al. Home telehealth for chronic obstructive pulmonary disease: A systematic review and meta-analysis. J Telemed Telecare 2010; 16: 120–127. [DOI] [PubMed] [Google Scholar]
- 29.Darkins A, Ryan P, Kobb R, et al. Care coordination/home telehealth: The systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health 2008; 14: 1118–1126. [DOI] [PubMed] [Google Scholar]
- 30.Kobb R, Chumbler NR, Brennan DMet al. et al. Home telehealth: Mainstreaming what we do well. Telemed J E Health 2008; 14: 977–981. [DOI] [PubMed] [Google Scholar]
- 31.Field MJ. Telemedicine: A guide to assessing telecommunications in healthcare. J Digit Imaging 1997; 10: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schneider NM. Managing congestive heart failure using home telehealth. Home Healthc Nurse 2004; 22: 719–722. [DOI] [PubMed] [Google Scholar]
- 33.Waqas A, Teoh SH, Lapão LVet al. et al. Harnessing telemedicine for the provision of health care: Bibliometric and scientometric analysis. J Med Internet Res 2020; 22: e18835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jong M, Mendez I, Jong R. Enhancing access to care in northern rural communities via telehealth. Int J Circumpolar Health 2019; 78: 1554174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brennan D, Tindall L, Theodoros D, et al. A blueprint for telerehabilitation guidelines. Int J Telerehabil 2010; 2: 31–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ambrosino N, Vagheggini G, Mazzoleni Set al. et al. Telemedicine in chronic obstructive pulmonary disease. Breathe (Sheff) 2016; 12: 350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peretti A, Amenta F, Tayebati SKet al. et al. Telerehabilitation: Review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol 2017; 4: e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andreu-Perez J, Leff DR, Ip HMet al. et al. From wearable sensors to smart implants–toward pervasive and personalized healthcare. IEEE Trans Biomed Eng 2015; 62: 2750–2762. [DOI] [PubMed] [Google Scholar]
- 39.Antoniades NC, Rochford PD, Pretto JJ, et al. Pilot study of remote telemonitoring in COPD. Telemed J E Health 2012; 18: 634–640. [DOI] [PubMed] [Google Scholar]
- 40.Au DH, Macaulay DS, Jarvis JLet al. et al. Impact of a telehealth and care management program for patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc 2015; 12: 323–331. [DOI] [PubMed] [Google Scholar]
- 41.Boer L, Bischoff E, van der Heijden M, et al. A smart Mobile health tool versus a paper action plan to support self-management of chronic obstructive pulmonary disease exacerbations: Randomized controlled trial. JMIR Mhealth Uhealth 2019; 7: e14408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chan DS, Callahan CW, Hatch-Pigott VB, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: Results of a 1-year asthma in-home monitoring trial. Pediatrics 2007; 119: 569–578. [DOI] [PubMed] [Google Scholar]
- 43.Chau JP-C, Lee DT-F, Yu DS-F, et al. A feasibility study to investigate the acceptability and potential effectiveness of a telecare service for older people with chronic obstructive pulmonary disease. Int J Med Inf 2012; 81: 674–682. [DOI] [PubMed] [Google Scholar]
- 44.Cushen B, Madden A, Long D, et al. Integrating hospital and community care: using a community virtual ward model to deliver combined specialist and generalist care to patients with severe chronic respiratory disease in their homes. Ir J Med Sci 2022; 191: 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Jongste JC, Carraro S, Hop WCet al. et al. Daily telemonitoring of exhaled nitric oxide and symptoms in the treatment of childhood asthma. American Journal of Respiratory & Critical Care Medicine 2009; 179: 93–97. [DOI] [PubMed] [Google Scholar]
- 46.Deng N, Chen J, Liu Y, et al. Using Mobile health technology to deliver a community-based closed-loop management system for chronic obstructive pulmonary disease patients in remote areas of China: Development and prospective observational study. JMIR Mhealth Uhealth 2020; 8: e15978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ding H, Karunanithi M, Kanagasingam Yet al. et al. A pilot study of a mobile-phone-based home monitoring system to assist in remote interventions in cases of acute exacerbation of COPD. J Telemed Telecare 2014; 20: 128–134. [DOI] [PubMed] [Google Scholar]
- 48.Farias R, Sedeno M, Beaucage D, et al. Innovating the treatment of COPD exacerbations: A phone interactive telesystem to increase COPD action plan adherence. BMJ Open Respir Res 2019; 6: e000379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Farmer A, Williams V, Velardo C, et al. Self-Management support using a digital health system compared with usual care for chronic obstructive pulmonary disease: Randomized controlled trial. J Med Internet Res 2017; 19: e144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jódar-Sánchez F, Ortega F, Parra C, et al. Implementation of a telehealth programme for patients with severe chronic obstructive pulmonary disease treated with long-term oxygen therapy. Journal of Telemedicine & Telecare 2013; 19: 11–17. [DOI] [PubMed] [Google Scholar]
- 51.Koff PB, Min S-J, Freitag TJ, et al. Impact of proactive integrated care on chronic obstructive pulmonary disease. Chronic Obstructive Pulmonary Diseases (Miami, Fla) 2021; 8: 100–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lewis KE, Annandale JA, Warm DLet al. et al. Home telemonitoring and quality of life in stable, optimised chronic obstructive pulmonary disease. J Telemed Telecare 2010; 16: 253–259. [DOI] [PubMed] [Google Scholar]
- 53.McDowell JE, McClean S, FitzGibbon Fet al. et al. A randomised clinical trial of the effectiveness of home-based health care with telemonitoring in patients with COPD. J Telemed Telecare 2015; 21: 80–87. [DOI] [PubMed] [Google Scholar]
- 54.Pare G, Poba-Nzaou P, Sicotte C, et al. Comparing the costs of home telemonitoring and usual care of chronic obstructive pulmonary disease patients: A randomized controlled trial. European Research in Telemedicine 2013; 2: 35–47. [Google Scholar]
- 55.Pedone C, Chiurco D, Scarlata Set al. et al. Efficacy of multiparametric telemonitoring on respiratory outcomes in elderly people with COPD: A randomized controlled trial. BMC Health Serv Res 2013; 13: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Persson HL, Lyth J, Lind L. The health diary telemonitoring and hospital-based home care improve quality of life among elderly multimorbid COPD and chronic heart failure subjects. Int J Chron Obstruct Pulmon Dis 2020; 15: 527–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pinnock H, Hanley J, McCloughan L, et al. Effectiveness of telemonitoring integrated into existing clinical services on hospital admission for exacerbation of chronic obstructive pulmonary disease: researcher blind, multicentre, randomised controlled trial. BMJ (Clinical Research ed) 2013; 347: f6070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rasmussen LM, Phanareth K, Nolte Het al. et al. Internet-based monitoring of asthma: A long-term, randomized clinical study of 300 asthmatic subjects. J Allergy Clin Immunol 2005; 115: 1137–1142. [DOI] [PubMed] [Google Scholar]
- 59.Schou L, Ostergaard B, Rydahl-Hansen S, et al. A randomised trial of telemedicine-based treatment versus conventional hospitalisation in patients with severe COPD and exacerbation - effect on self-reported outcome. J Telemed Telecare 2013; 19: 160–165. [DOI] [PubMed] [Google Scholar]
- 60.Stamenova V, Liang K, Yang R, et al. Technology-Enabled self-management of chronic obstructive pulmonary disease with or without asynchronous remote monitoring: Randomized controlled trial. J Med Internet Res 2020; 22: e18598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.van Gaalen JL, Beerthuizen T, van der Meer V, et al. Long-term outcomes of internet-based self-management support in adults with asthma: Randomized controlled trial. J Med Internet Res 2013; 15: e188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vianello A, Fusello M, Gubian L, et al. Home telemonitoring for patients with acute exacerbation of chronic obstructive pulmonary disease: A randomized controlled trial. BMC Pulm Med 2016; 16: 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zairina E, Abramson MJ, McDonald CF, et al. Telehealth to improve asthma control in pregnancy: A randomized controlled trial. Respirology (Carlton, Vic) 2016; 21: 867–874. [DOI] [PubMed] [Google Scholar]
- 64.Bermejo-Gil BM, Perez-Robledo F, Llamas-Ramos R, et al. Respiraconnosotros: A viable home-based telerehabilitation system for respiratory patients. Sensors (Basel, Switzerland) 2021; 21: 3318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Burkow TM, Vognild LK, Johnsen E, et al. Comprehensive pulmonary rehabilitation in home-based online groups: A mixed method pilot study in COPD. BMC Res Notes 2015; 8: 766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hansen H, Bieler T, Beyer N, et al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: A randomised multicentre trial. Thorax 2020; 75: 413–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jiang Y, Liu F, Guo J, et al. Evaluating an intervention program using WeChat for patients with chronic obstructive pulmonary disease: Randomized controlled trial. J Med Internet Res 2020; 22: e17089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jimenez-Reguera B, Maroto Lopez E, Fitch S, et al. Development and preliminary evaluation of the effects of an mHealth web-based platform (HappyAir) on adherence to a maintenance program after pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: Randomized controlled trial. JMIR Mhealth Uhealth 2020; 8: e18465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lewis A, Knight E, Bland M, et al. Feasibility of an online platform delivery of pulmonary rehabilitation for individuals with chronic respiratory disease. BMJ Open Respir Res 2021; 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stickland M, Jourdain T, Wong EYet al. et al. Using telehealth technology to deliver pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Can Respir J 2011; 18: 216–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Benzo RP, Ridgeway J, Hoult JP, et al. Feasibility of a health coaching and home-based rehabilitation intervention with remote monitoring for COPD. Respir Care 2021; 66: 960–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bhatt SP, Patel SB, Anderson EM, et al. Video telehealth pulmonary rehabilitation intervention in chronic obstructive pulmonary disease reduces 30-day readmissions. New York, New York: American Thoracic Society, 2019, pp.511–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Broadbent E, Garrett J, Jepsen N, et al. Using robots at home to support patients with chronic obstructive pulmonary disease: Pilot randomized controlled trial. J Med Internet Res 2018; 20: e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Galdiz JB, Gomez A, Rodriguez D, et al. Telerehabilitation programme as a maintenance strategy for COPD patients: A 12-month randomized clinical trial. Arch Bronconeumol 2021; 57: 195–204. [DOI] [PubMed] [Google Scholar]
- 75.Gilmutdinova IR, Kolyshenkov VA, Lapickaya KA, et al. Telemedicine platform COVIDREHAB for remote rehabilitation of patients after COVID-19. Eur J Transl Myol 2021; 31: 9783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Holland AE, Hill CJ, Rochford Pet al. et al. Telerehabilitation for people with chronic obstructive pulmonary disease: Feasibility of a simple, real time model of supervised exercise training. J Telemed Telecare 2013; 19: 222–226. [DOI] [PubMed] [Google Scholar]
- 77.Marquis N, Larivee P, Saey Det al. et al. In-Home pulmonary telerehabilitation for patients with chronic obstructive pulmonary disease: A Pre-experimental study on effectiveness, satisfaction, and adherence. Telemed J E Health 2015; 21: 870–879. [DOI] [PubMed] [Google Scholar]
- 78.Paneroni M, Saleri M, Vitacca M, et al. Is telerehabilitation a safe and viable option for patients with COPD? A feasibility study. COPD: Journal of Chronic Obstructive Pulmonary Disease 2015; 12: 217–225. [DOI] [PubMed] [Google Scholar]
- 79.Rassouli F, Boutellier D, Duss Jet al. et al. Digitalizing multidisciplinary pulmonary rehabilitation in COPD with a smartphone application: An international observational pilot study. Int J Chron Obstruct Pulmon Dis 2018; 13: 3831–3836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ringbaek T, Green A, Laursen LCet al. et al. Effect of tele health care on exacerbations and hospital admissions in patients with chronic obstructive pulmonary disease: A randomized clinical trial. Int J Chron Obstruct Pulmon Dis 2015; 10: 1801–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tsai LLY, McNamara RJ, Moddel Cet al. et al. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: The randomized controlled TeleR study. Respirology (Carlton, Vic) 2017; 22: 699–707. [DOI] [PubMed] [Google Scholar]
- 82.Vitacca M, Bianchi L, Guerra A, et al. Tele-assistance in chronic respiratory failure patients: A randomised clinical trial. Eur Respir J 2009; 33: 411–418. [DOI] [PubMed] [Google Scholar]
- 83.Paneroni M, Simonelli C, Vitacca Met al. et al. Aerobic exercise training in very severe chronic obstructive pulmonary disease: A systematic review and meta-analysis. Am J Phys Med Rehabil 2017; 96: 541–548. [DOI] [PubMed] [Google Scholar]
- 84.Cox NS, Dal Corso S, Hansen H, et al. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst Rev 2021; 1 : CD013040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Snoswell CL, Chelberg G, De Guzman KR, et al. The clinical effectiveness of telehealth: a systematic review of meta-analyses from 2010 to 2019. J Telemed Telecare 2021. DOI: 10.1177/1357633X211022907. [DOI] [PubMed] [Google Scholar]
- 86.Kruse C, Pesek B, Anderson Met al. et al. Telemonitoring to manage chronic obstructive pulmonary disease: systematic literature review. JMIR Med Inform 2019; 7: e11496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Seto E. Cost comparison between telemonitoring and usual care of heart failure: A systematic review. Telemed J E Health 2008; 14: 679–686. [DOI] [PubMed] [Google Scholar]
- 88.Venter A, Burns R, Hefford Met al. et al. Results of a telehealth-enabled chronic care management service to support people with long-term conditions at home. J Telemed Telecare 2012; 18: 172–175. [DOI] [PubMed] [Google Scholar]
- 89.Snoswell CL, Stringer H, Taylor MLet al. et al. An overview of the effect of telehealth on mortality: A systematic review of meta-analyses. J Telemed Telecare 2021. DOI. 10.1177/1357633X211023700. [DOI] [PubMed] [Google Scholar]
- 90.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26: 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Thomas EE, Haydon HM, Mehrotra A, et al. Building on the momentum: Sustaining telehealth beyond COVID-19. J Telemed Telecare 2022; 28: 301–308. [DOI] [PubMed] [Google Scholar]
- 92.Leochico CFD, Rey-Matias BMV, Rey-Matias RR. Telerehabilitation perceptions and experiences of physiatrists in a lower-middle-income country during the COVID-19 pandemic. Pm r 2022; 14: 210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Werneke MW, Deutscher D, Grigsby Det al. et al. Telerehabilitation during the COVID-19 pandemic in outpatient rehabilitation settings: A descriptive study. Phys Ther 2021; 101: pzab110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jtt-10.1177_1357633X221122124 for Effect of telemonitoring and telerehabilitation on physical activity, exercise capacity, health-related quality of life and healthcare use in patients with chronic lung diseases or COVID-19: A scoping review by Diana C Sanchez-Ramirez, Margriet Pol, Hal Loewen, and Mohamed-Amine Choukou in Journal of Telemedicine and Telecare