Abstract
Studies have indicated that anticancer drugs targeting cholesterol metabolism have clinical significance. From the perspective of the mechanism of cholesterol excretion from cells, ATP-binding cassette (ABC)A1 has an essential role that cannot be ignored. ABCA1 is located on the cell membrane and able to mediate the efflux of lipids, such as intracellular cholesterol, thereby initiating reverse cholesterol transport to reduce the intracellular cholesterol level. Therefore, inducing the expression of ABCA1 may become a new breakthrough point in cancer therapy.
Keywords: ABCA1, drug resistance, cell proliferation, invasion and metastasis
1. Introduction
Certain studies have indicated that cancer cells have an enhanced ability to proliferate and invade caused by changes in their metabolism, among which abnormal cholesterol metabolism has a key role. It is mainly manifested as abnormally increased or abnormally accumulated cholesterol in cancer cells, and inhibiting the increase of cholesterol levels may slow down the proliferation of cancer cells. An important factor affecting intracellular cholesterol levels is protein transport (1). ATP-binding cassette (ABC) transporters are localized to the plasma membrane and function as a class of lipid transporters. Energy is obtained by hydrolyzing ATP, thereby mediating the efflux of intracellular phospholipids and free cholesterol, which combine with non-fat or low-fat apolipoprotein A-I (apo A-I) on the cell surface to form high-density lipoprotein (HDL) to then initiate the reverse cholesterol transport process (2,3). When exploring the association between cholesterol and malignant cancers, it was observed that the accumulation of excessive intracellular cholesterol may promote the development of cancer cells to a certain extent (4). Phillips (5) indicated that high cholesterol levels were positively associated with the aggressiveness of prostate cancer. Abnormally active cholesterol metabolism in cancer cells leads to proliferation, survival, invasion, metastasis and enhanced adaptation to the cancer microenvironment (6). ABCA1 is also closely related to cancer resistance mechanisms (7); thus, inducing the expression of ABCA1 may provide novel therapeutic strategies for cancer prevention, inhibition and even treatment, bringing new hope for the treatment of cancer patients (8).
2. Influence of intracellular lipid microenvironment on cancers
As mentioned earlier in the introduction, cholesterol has an important role in the development of cancers, such as participation in the proliferation, migration and invasion of cancer cells. Luo et al (9) indicated that the abnormal cholesterol metabolism of cancer cells leads to proliferation, survival, invasion, metastasis and enhanced adaptability to the cancer microenvironment, thereby promoting the occurrence and development of cancers. Changes in membrane cholesterol and cholesterol-rich membranes have been observed to affect the progression and invasion of cancers (9). Cholesterol homeostasis is critical for cellular function and survival, and dysregulated cholesterol homeostasis is known to be associated with a variety of cancers, including prostate cancer (10), and alterations in lipid metabolism are increasingly recognized as a hallmark of prostate cancer cells (11). A large number of studies suggested that a variety of genes related to cholesterol synthesis exhibit increased activity in cancer cells, thereby promoting the growth, migration and metastasis of various cancer cell types, including gastric cancer, glioma and prostate cancer (12–14). In addition, it was reported that the expression of low-density lipoprotein receptors (LDLR) is upregulated in various cancer cells, which was significantly associated with poor clinical prognosis in patients with small cell lung cancer (15–18). Elevated expression of LDLR in patients with pancreatic cancer was associated with an increased recurrence rate. However, silencing of HDLR by short hairpin RNA in pancreatic cancer cells significantly reduced the cholesterol uptake, thereby inhibiting the proliferation of pancreatic cancer cells. Treatments related to the synthesis, uptake and esterification of cholesterol may alleviate cancer progression (19–21). It was reported that altering the intracellular lipid microenvironment by affecting various metabolic pathways of cholesterol has an important role in the proliferation and invasion of certain types of cancer cell (22,23). Table I summarizes the specific effects of intracellular cholesterol levels on cancer; as one of the major efflux pathways of cellular cholesterol, ABCA1 may be an important determinant of prostate cancer aggressiveness and a potential therapeutic target (24,25).
Table I.
Effect of cholesterol levels on cancers.
| Cancer type | Cholesterol intake | Cholesterol synthesis | ABCA1 expression | Function | (Refs.) |
|---|---|---|---|---|---|
| Prostate cancer | HDLR high expression | High expression of squalene monooxygenase | Low expression (methylation) | High cholesterol promotes tumor development | (44,46) |
| Glioblastoma | - | High expression of HMGCR | Low expression | High cholesterol promotes tumor development | (25) |
| Pancreatic cancer | LDLR high expression | - | Low expression | High cholesterol promotes tumor development | (31,32) |
| Breast cancer | LDLR high expression | - | Low expression | 27-HC promotes cell proliferation and metastasis | (43) |
| Lung cancer | - | - | Low expression | HDL-C is negatively correlated with the occurrence and development of lung cancer | (48,67) |
| Ovarian cancer | - | High expression of cholesterol synthase | Low expression (methylation) | High cholesterol promotes tumor development | (56,57) |
ABC, ATP-binding cassette; LDLR, low-density lipoprotein receptor; HDL-C, high-density lipoprotein cholesterol.
3. Effect of ABCA1 on the intracellular lipid microenvironment
ABCA1 and plasma membrane remodeling and lipid redistribution
ABCA1 is known as the main efflux channel of intracellular cholesterol. Although there is still no perfect model to explain the mechanism, the latest efflux mechanism is widely recognized (8). Multiple studies suggested that the binding of apo A-I to ABCA1 may lead to the redistribution of phospholipids and cholesterol on the outside of the plasma membrane, thereby changing the intracellular lipid microenvironment and remodeling the plasma membrane, which facilitated the binding of apo A-I to lipids and maintained intracellular cholesterol homeostasis (26–29). After the combination of the two, the plasma membrane is remodeled in two ways: Horizontal and vertical. The vertical remodeling promotes the net transport of phospholipids to the outer leaflets of the plasma membrane through ABCA1, resulting in an imbalance in the packing density of the two leaflets of the phospholipid bilayer, thereby regulating the lipid density of the plasma membrane (30). In horizontal remodeling, ABCA1 is enabled by hydrolysis of ATP, causing the phospholipid and cholesterol molecules that constitute the plasma membrane to translocate laterally on the cell membrane, resulting in the redistribution of lipids from non-lipid rafts to lipid rafts, which in turn changes the lipid distribution of the entire plasma membrane (31–33). Therefore, it may be speculated that ABCA1 changes the intracellular lipid microenvironment through plasma membrane remodeling and lipid redistribution.
ABCA1 and intracellular lipid efflux
All cells in the body are able to synthesize cholesterol, but most of them lack effective metabolic pathways and may only be excreted from cells through a series of transporters (34). Among them, ABCA1 is able to use the energy provided by ATP to promote the efflux of free cholesterol and phospholipids in cells, and combine with apo A-I on the cell surface to form new HDL, which in turn initiates the reverse cholesterol transport process to transport cholesterol from peripheral tissues back to the liver (35–37). At this stage, it has been indicated that numerous factors (such as IGF-1), are able to directly or indirectly regulate the expression level of ABCA1 to affect the intracellular cholesterol level (38). The importance of ABCA1 for cholesterol efflux is currently widely recognized, but the pathway to the plasma membrane remains to be fully elucidated (39). Yoshioka et al (40) provided three models of cholesterol efflux mechanisms. They are the channel transport model, the mushroom-like protrusion model and the endocytosis-exocytosis transport model. The channel transport model is widely accepted and is presented in Fig. 1 to indicate how ABCA1 is able to regulate the intracellular microenvironment by transporting intracellular lipids.
Figure 1.

Mechanism of lipid efflux mediated by ABCA1. ① Low-density lipoprotein binds to ABCA1 to form a complex. ② The complex is internalized, part of it is transferred to the lysosome for degradation and the rest is located to the endosome. ③ The complex on the endosome combines with lipid to form the apoA-l/lipid complex. ④ The lipid complexes are resecreted through exocytosis, and after dissociation, they are conducive to the formation of high-density lipoprotein complexes. Apo, apolipoprotein; ABC, ATP-binding cassette.
4. ABCA1 and cancer cell proliferation, invasion and metastasis
The above studies proved that a series of life activities of cancer cells are closely related to the level of intracellular cholesterol and ABCA1 indirectly affects the proliferation, metastasis and invasion of cancer cells by regulating the level of intracellular cholesterol (41–44). ABCA1 mediates the transmembrane transport of free intracellular cholesterol and phospholipids to apo A-I, which has an important role in maintaining the normal metabolism of intracellular cholesterol. As indicated by Prochazka et al (45), in non-small cell lung carcinoma H1299 cells, overexpression of ABCA1 enhanced drug resistance. ABCA1 is strongly expressed in normal breast epithelium and the reduced expression of ABCA1 in breast cancer appears to be associated with poor prognosis (46). Activated liver X receptor and overexpression of ABCA1 have been reported to reduce cholesterol levels and cancer growth in mouse prostate cancer xenografts (47). Maslyanko et al (48) also indicated that high cholesterol levels may promote the proliferation of breast cancer cells in a mouse transgenic model, specifically by upregulating the protein expression of ABCA1 to maintain the cholesterol balance in the body and inhibit the proliferation of cancer cells. It was also indicated that cholesterol efflux has an important role in the treatment of lung cancer. Downregulation of ABCA1 was evident in all prostate cancers. It has been reported that when prostate cancer metastasizes, the cells contain high levels of cholesterol (49). Studies suggested that cancer-specific ABCA1 methylation and loss of protein expression directly led to elevated intracellular cholesterol levels in cancer cells, thus forming a microenvironment favorable for cancer progression (50). Liu et al (51) indicated that microRNA-200b-3p acts as an oncogene in lung adenocarcinoma samples and in the human lung adenocarcinoma cell lines A549 and H1299 by targeting ABCA1, and overexpression of ABCA1 significantly inhibited the proliferation, migration and invasion of lung adenocarcinoma cells. Huang et al (52) demonstrated that ABCA1 may protect the normal function of cells by maintaining low levels of cholesterol in mitochondria and have a certain inhibitory effect on the proliferation of cancer cells. Prostate cancer bone metastases exhibit clear metabolic differences from bone metastases of other cancer types, including increased levels of cholesterol. Regulation of cholesterol in the plasma membrane has been indicated to modulate the ability of cells to migrate (53). Furthermore, cholesterol-rich lipid rafts were reported to have an important role in the adhesion and migration of cancer cells (54,55). The activity of phosphoinositide 3-kinase is able to regulate the surface protein expression of ABCA1, which significantly increases the risk of cancer cells entering the blood to form metastases (56). In Tables I and II, the specific effects of ABCA1 in cancer cells are summarized, linking abnormal cholesterol levels to aberrant ABCA1 expression, regulation of ABCA1 expression levels, which may be utilized for inhibiting cancer cells to proliferate, metastasize and invade.
Table II.
ABCA1 and cancer cell proliferation, invasion and metastasis.
| Cancer type | Cancer cell proliferation, invasion and metastasis | (Refs.) |
|---|---|---|
| Prostate cancer | High levels of cholesterol can modulate the ability of cells to migrate | (49) |
| Breast cancer | Reduced expression of ABCA1 in breast cancer appears to be associated with poor prognosis | (46) |
| Non-small cell lung carcinoma | Upregulation of the expression level of ABCA1 enhances drug resistance | (45) |
| Lung adenocarcinoma | Overexpression of ABCA1 significantly inhibits the proliferation, migration and invasion of lung adenocarcinoma cells | (53) |
ABC, ATP-binding cassette.
5. ABCA1 and cancer therapy
It is promising to treat cancer by regulating the expression level of ABCA1, thereby regulating the level of intracellular cholesterol. Of note, cancer cells require excess cholesterol to maintain high levels of proliferation, which has been widely accepted (57). Available epidemiological data indicated that low serum cholesterol as well as statins reduce the risk of prostate cancer, demonstrating that cholesterol metabolism has a role in the development of aggressive prostate cancer (58). Therefore, it may be speculated that high expression of ABCA1 is able to mediate cholesterol efflux, resulting in the reduction of intracellular cholesterol in prostate cancer cells to achieve the purpose of inhibiting cancer growth. Ovarian cancer is a common gynecological malignancy. Although chemotherapy is able to delay the disease, the post-operative survival rate is not high. Studies have indicated that ABCA1 has a key role in drug resistance and prognosis (59). According to the latest research, patients with ovarian cancer with high methylation of RASSF1C (functions as an oncogene in cancer cells) and low ABCA1 expression have shorter survival (60). In conclusion, existing studies suggest that moderately high expression of ABCA1 has a positive effect on the treatment of prostate cancer and breast cancer.
6. ABCA1 and drug resistance of cancer
ABCA1, as a research hotspot in recent years, has received extensive attention due to its function, and as a major transporter regulating intracellular cholesterol, its role in cancer resistance has attracted much attention (8). Chemotherapy, as one of the most important cancer treatment methods, is still not able to completely remove cancer cells. Chemotherapy tolerance is one of the most common problems in chemotherapy failure. Therefore, overcoming the resistance of cancer cells to chemotherapeutic drugs is an important issue in cancer treatment (61). Multidrug resistance generally refers to the adaptability of cancer cells to increase drug output and decrease drug uptake, and drug transporters have a key role in pre-targeted drug resistance (62). Existing studies suggested found that chemotherapy failure is directly related to ABC transporters and preventing the induction of ABC transporters in cancer cells may help avoid drug resistance (63). The high expression of transporters in cancer cells results in a variety of anticancer drugs being transported out of cells and unable to exert their anticancer effects (64,65), which has been observed in the drug resistance to curcumin, doxorubicin and nitidine in the treatment of breast and lung cancer (66–68). Chen et al (69) indicated that ABC transporters have a certain role in cancer stem cells through the reversal of inhibition of ABC transporter expression. There are numerous ways to overcome the drug resistance that depends on high expression of ABCA1, such as valproic acid downregulating the expression level of ABCA1 through histone deacetylase 2, thereby enhancing the sensitivity of non-small cell lung cancer cells to cisplatin (70). ABCA1-dependent resistance to α-tocopheryl succinate in mitochondria-targeted therapy of lung cancer was also reported (71). However, certain studies also indicated that when the expression level of ABCA1 in cancer cells was generally decreased, cholesterol accumulated and increased the order of bilayer phospholipids, thereby reducing the permeability of the membrane and finally promoting the resistance of cancers to membrane-active anticancer drugs (72). As indicated in Fig. 2, the role of ABCA1 in multidrug resistance has been widely recognized and measuring the expression of ABCA1 may be used to predict the response to anticancer drugs.
Figure 2.
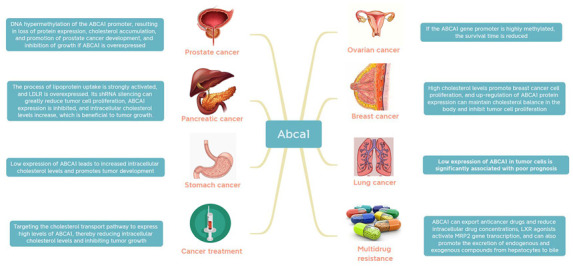
Roles of ABCA1 in various cancer types and cancer treatment (64,65,69,71,72). ABC, ATP-binding cassette; shRNA, short hairpin RNA; LDLR, low-density lipoprotein receptor; MRP2, multidrug resistance-associated protein 2.
7. Conclusion and perspective
Cholesterol efflux minimizes the potential harm to cells by excess cholesterol, but cancer cells have evolved to exploit this link to promote malignancy. As one of the main transporters of intracellular cholesterol efflux, ABCA1 has been widely recognized and used in anti-atherosclerosis treatment (73); its ability to transport cholesterol also has great potential in cancer treatment (74). Further research on ABCA1 will help elucidate its transport function and mechanisms to inhibit the transport of chemotherapeutic drugs, as well as the related effects of its reduced expression level on cancer cells, so as to achieve the purpose of cancer treatment. By modifying and inhibiting this gene, mechanisms of cancer cell growth and efflux of chemotherapeutic drugs may be interfered with. This provides novel directions for research on lipid metabolism and offers new effective targets for cancer prevention, inhibition and treatment. ABCA1 in cancer and provides a new avenue for drug discovery and therapy.
Acknowledgements
Not applicable.
Funding Statement
This work was funded by the Hengyang City Science and Technology Planning Project (grant no. 202150063473), the Scientific Research Project of Hunan Provincial Health Commission (grant no. 202202044140), the Scientific Research Project of Hunan Provincial Education Department (grant no. 21B0438) and the Undergraduate Research-based Learning and Innovative Experimental Program of the University of South China (grant no. X202110555457).
Availability of data and materials
Not applicable.
Authors' contributions
XY was responsible for the design of the review. XL, XY and LZ were responsible for revising the draft. KW drafted the manuscript, all authors approved the final draft. All authors read and approved the final manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Bian X, Liu R, Meng Y, Xing D, Xu D, Lu Z. Lipid metabolism and cancer. J Exp Med. 2021;218:e20201606. doi: 10.1084/jem.20201606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang YC, Lee TS, Chiang AN. Quercetin enhances ABCA1 expression and cholesterol efflux through a p38-dependent pathway in macrophages. J Lipid Res. 2012;53:1840–1850. doi: 10.1194/jlr.M024471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang J, Wang WJ, Zhai L, Zhang DF. Association of cholesterol with risk of pancreatic cancer: A meta-analysis. World J Gastroenterol. 2015;21:3711–3719. doi: 10.3748/wjg.v21.i12.3711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee BH, Taylor MG, Robinet P, Smith JD, Schweitzer J, Sehayek E, Falzarano SM, Magi-Galluzzi C, Klein EA, Ting AH. Dysregulation of cholesterol homeostasis in human prostate cancer through loss of ABCA1. Cancer Res. 2013;73:1211–1218. doi: 10.1158/0008-5472.CAN-12-3128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phillips MC. Molecular mechanisms of cellular cholesterol efflux. J Biol Chem. 2014;289:24020–24029. doi: 10.1074/jbc.R114.583658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chushi L, Wei W, Kangkang X, Yongzeng F, Ning X, Xiaolei C. HMGCR is up-regulated in gastric cancer and promotes the growth and migration of the cancer cells. Gene. 2016;587:42–47. doi: 10.1016/j.gene.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 7.Wang W, Lokman NA, Noye TM, Macpherson AM, Oehler MK, Ricciardelli C. ABCA1 is associated with the development of acquired chemotherapy resistance and predicts poor ovarian cancer outcome. Cancer Drug Resist. 2021;4:485–502. doi: 10.20517/cdr.2020.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobo-Albavera L, Domínguez-Pérez M, Medina-Leyte DJ, González-Garrido A, Villarreal-Molina T. The role of the ATP-binding cassette A1 (ABCA1) in human disease. Int J Mol Sci. 2021;22:1593. doi: 10.3390/ijms22041593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo X, Cheng C, Tan Z, Li N, Tang M, Yang L, Cao Y. Emerging roles of lipid metabolism in cancer metastasis. Mol Cancer. 2017;16:76. doi: 10.1186/s12943-017-0646-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adlakha YK, Khanna S, Singh R, Singh VP, Agrawal A, Saini N. Pro-apoptotic miRNA-128-2 modulates ABCA1, ABCG1 and RXRα expression and cholesterol homeostasis. Cell Death Dis. 2013;4:e780. doi: 10.1038/cddis.2013.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yue S, Li J, Lee SY, Lee HJ, Shao T, Song B, Cheng L, Masterson TA, Liu X, Ratliff TL, Cheng JX. Cholesteryl ester accumulation induced by PTEN loss and PI3K/AKT activation underlies human prostate cancer aggressiveness. Cell Metab. 2014;19:393–406. doi: 10.1016/j.cmet.2014.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiu Z, Yuan W, Chen T, Zhou C, Liu C, Huang Y, Han D, Huang Q. HMGCR positively regulated the growth and migration of glioblastoma cells. Gene. 2016;576:22–27. doi: 10.1016/j.gene.2015.09.067. [DOI] [PubMed] [Google Scholar]
- 13.Ashida S, Kawada C, Inoue K. Stromal regulation of prostate cancer cell growth by mevalonate pathway enzymes HMGCS1 and HMGCR. Oncol Lett. 2017;14:6533–6542. doi: 10.3892/ol.2017.7025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xiong T, Xu G, Huang XL, Lu KQ, Xie WQ, Yin K, Tu J. ATP-binding cassette transporter A1: A promising therapy target for prostate cancer. Mol Clin Oncol. 2018;8:9–14. doi: 10.3892/mco.2017.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo D, Reinitz F, Youssef M, Hong C, Nathanson D, Akhavan D, Kuga D, Amzajerdi AN, Soto H, Zhu S, et al. An LXR agonist promotes glioblastoma cell death through inhibition of an EGFR/AKT/SREBP-1/LDLR-dependent pathway. Cancer Discov. 2011;1:442–456. doi: 10.1158/2159-8290.CD-11-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Touvier M, Fassier P, His M, Norat T, Chan DS, Blacher J, Hercberg S, Galan P, Druesne-Pecollo N, Latino-Martel P. Cholesterol and breast cancer risk: A systematic review and meta-analysis of prospective studies. Br J Nutr. 2015;114:347–357. doi: 10.1017/S000711451500183X. [DOI] [PubMed] [Google Scholar]
- 17.Zhou P, Li B, Liu B, Chen T, Xiao J. Prognostic role of serum total cholesterol and high-density lipoprotein cholesterol in cancer survivors: A systematic review and meta-analysis. Clin Chim Acta. 2018;477:94–104. doi: 10.1016/j.cca.2017.11.039. [DOI] [PubMed] [Google Scholar]
- 18.Guillaumond F, Bidaut G, Ouaissi M, Servais S, Gouirand V, Olivares O, Lac S, Borge L, Roques J, Gayet O, et al. Cholesterol uptake disruption, in association with chemotherapy, is a promising combined metabolic therapy for pancreatic adenocarcinoma. Proc Natl Acad Sci USA. 2015;112:2473–2478. doi: 10.1073/pnas.1421601112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Menter DG, Ramsauer VP, Harirforoosh S, Chakraborty K, Yang P, His L, Newman RA, Krishnan K. Differential effects of pravastatin and simvastatin on the growth of tumor cells from different organ sites. PLoS One. 2011;6:e28813. doi: 10.1371/journal.pone.0028813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J, Gu D, Lee SS, Song B, Bandyopadhyay S, Chen S, Konieczny SF, Ratliff TL, Liu X, Xie J, Cheng JX. Abrogating cholesterol esterification suppresses growth and metastasis of pancreatic cancer. Oncogene. 2016;35:6378–6388. doi: 10.1038/onc.2016.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou T, Zhan J, Fang W, Zhao Y, Yang Y, Hou X, Zhang Z, He X, Zhang Y, Huang Y, Zhang L. Serum low-density lipoprotein and low-density lipoprotein expression level at diagnosis are favorable prognostic factors in patients with small-cell lung cancer (SCLC) BMC Cancer. 2017;17:269. doi: 10.1186/s12885-017-3239-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cruz PM, Mo H, McConathy WJ, Sabnis N, Lacko AG. The role of cholesterol metabolism and cholesterol transport in carcinogenesis: A review of scientific findings, relevant to future cancer therapeutics. Front Pharmacol. 2013;4:119. doi: 10.3389/fphar.2013.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Folkerd EJ, Dowsett M. Influence of sex hormones on cancer progression. J Clin Oncol. 2010;28:4038–4044. doi: 10.1200/JCO.2009.27.4290. [DOI] [PubMed] [Google Scholar]
- 24.Phillips MC. Is ABCA1 a lipid transfer protein? J Lipid Res. 2018;59:749–763. doi: 10.1194/jlr.R082313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saxena K, Shipley GG. Structural studies of detergent-solubilized and vesicle-reconstituted low-density lipoprotein (LDL) receptor. Biochemistry. 1997;36:15940–15948. doi: 10.1021/bi971579p. [DOI] [PubMed] [Google Scholar]
- 26.Vedhachalam C, Duong PT, Nickel M, Nguyen D, Dhanasekaran P, Saito H, Rothblat GH, Lund-Katz S, Phillips MC. Mechanism of ATP-binding cassette transporter A1-mediated cellular lipid efflux to apolipoprotein A-I and formation of high density lipoprotein particles. J Biol Chem. 2007;282:25123–25130. doi: 10.1074/jbc.M704590200. [DOI] [PubMed] [Google Scholar]
- 27.Nagao K, Tomioka M, Ueda K. Function and regulation of ABCA1-membrane meso-domain organization and reorganization. FEBS J. 2011;278:3190–3203. doi: 10.1111/j.1742-4658.2011.08170.x. [DOI] [PubMed] [Google Scholar]
- 28.Takahashi Y, Smith JD. Cholesterol efflux to apolipoprotein AI involves endocytosis and resecretion in a calcium-dependent pathway. Proc Natl Acad Sci USA. 1999;96:11358–11363. doi: 10.1073/pnas.96.20.11358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu R, Arakawa R, Ito-Osumi C, Iwamoto N, Yokoyama S. ApoA-I facilitates ABCA1 recycle/accumulation to cell surface by inhibiting its intracellular degradation and increases HDL generation. Arterioscler Thromb Vasc Biol. 2008;28:1820–1824. doi: 10.1161/ATVBAHA.108.169482. [DOI] [PubMed] [Google Scholar]
- 30.Hamon Y, Broccardo C, Chambenoit O, Luciani MF, Toti F, Chaslin S, Freyssinet JM, Devaux PF, McNeish J, Marguet D, Chimini G. ABC1 promotes engulfment of apoptotic cells and transbilayer redistribution of phosphatidylserine. Nat Cell Biol. 2000;2:399–406. doi: 10.1038/35017029. [DOI] [PubMed] [Google Scholar]
- 31.Landry YD, Denis M, Nandi S, Bell S, Vaughan AM, Zha X. ATP-binding cassette transporter A1 expression disrupts raft membrane microdomains through its ATPase-related functions. J Biol Chem. 2006;281:36091–36101. doi: 10.1074/jbc.M602247200. [DOI] [PubMed] [Google Scholar]
- 32.Santamarina-Fojo S, Remaley AT, Neufeld EB, Brewer HB., Jr Regulation and intracellular trafficking of the ABCA1 transporter. J Lipid Res. 2001;42:1339–1345. doi: 10.1016/S0022-2275(20)30266-2. [DOI] [PubMed] [Google Scholar]
- 33.Koseki M, Hirano K, Masuda D, Ikegami C, Tanaka M, Ota A, Sandoval JC, Nakagawa-Toyama Y, Sato SB, Kobayashi T, et al. Increased lipid rafts and accelerated lipopolysaccharide-induced tumor necrosis factor-alpha secretion in Abca1-deficient macrophages. J Lipid Res. 2007;48:299–306. doi: 10.1194/jlr.M600428-JLR200. [DOI] [PubMed] [Google Scholar]
- 34.Tang SL, Chen WJ, Yin K, Zhao GJ, Mo ZC, Lv YC, Ouyang XP, Yu XH, Kuang HJ, Jiang ZS, et al. PAPP-A negatively regulates ABCA1, ABCG1 and SR-B1 expression by inhibiting LXRα through the IGF-I-mediated signaling pathway. Atherosclerosis. 2012;222:344–354. doi: 10.1016/j.atherosclerosis.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 35.Wang N, Silver DL, Thiele C, Tall AR. ATP-binding cassette transporter A1 (ABCA1) functions as a cholesterol efflux regulatory protein. J Biol Chem. 2001;276:23742–23747. doi: 10.1074/jbc.M102348200. [DOI] [PubMed] [Google Scholar]
- 36.Smith JD, Le Goff W, Settle M, Brubaker G, Waelde C, Horwitz A, Oda MN. ABCA1 mediates concurrent cholesterol and phospholipid efflux to apolipoprotein A-I. J Lipid Res. 2004;45:635–644. doi: 10.1194/jlr.M300336-JLR200. [DOI] [PubMed] [Google Scholar]
- 37.Tall AR. An overview of reverse cholesterol transport. Eur Heart J. 1998;19((Suppl A)):A31–A35. [PubMed] [Google Scholar]
- 38.Qian H, Zhao X, Cao P, Lei J, Yan N, Gong X. Structure of the human lipid exporter ABCA1. Cell. 2017;169:1228–1239.e10. doi: 10.1016/j.cell.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 39.Kang MH, Singaraja R, Hayden MR. Adenosine-triphosphate-binding cassette transporter-1 trafficking and function. Trends Cardiovasc Med. 2010;20:41–49. doi: 10.1016/j.tcm.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 40.Yoshioka Y, Sasaki J, Yamamoto M, Saitoh K, Nakaya S, Kubokawa M. Quantitation by (1)H-NMR of dolichol, cholesterol and choline-containing lipids in extracts of normal and phathological thyroid tissue. NMR Biomed. 2000;13:377–383. doi: 10.1002/1099-1492(200011)13:7<377::AID-NBM658>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 41.Ding X, Zhang W, Li S, Yang H. The role of cholesterol metabolism in cancer. Am J Cancer Res. 2019;9:219–227. [PMC free article] [PubMed] [Google Scholar]
- 42.Kitahara CM, Berrington de González A, Freedman ND, Huxley R, Mok Y, Jee SH, Samet JM. Total cholesterol and cancer risk in a large prospective study in Korea. J Clin Oncol. 2011;29:1592–1598. doi: 10.1200/JCO.2010.31.5200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang B, Song BL, Xu C. Cholesterol metabolism in cancer: Mechanisms and therapeutic opportunities. Nat Metab. 2020;2:132–141. doi: 10.1038/s42255-020-0174-0. [DOI] [PubMed] [Google Scholar]
- 44.Tabas I. Consequences of cellular cholesterol accumulation: Basic concepts and physiological implications. J Clin Invest. 2002;110:905–911. doi: 10.1172/JCI0216452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Prochazka L, Koudelka S, Dong LF, Stursa J, Goodwin J, Neca J, Slavik J, Ciganek M, Masek J, Kluckova K, et al. Mitochondrial targeting overcomes ABCA1-dependent resistance of lung carcinoma to α-tocopheryl succinate. Apoptosis. 2013;18:286–299. doi: 10.1007/s10495-012-0795-1. [DOI] [PubMed] [Google Scholar]
- 46.Schimanski S, Wild PJ, Treeck O, Horn F, Sigruener A, Rudolph C, Blaszyk H, Klinkhammer-Schalke M, Ortmann O, Hartmann A, Schmitz G. Expression of the lipid transporters ABCA3 and ABCA1 is diminished in human breast cancer tissue. Horm Metab Res. 2010;42:102–109. doi: 10.1055/s-0029-1241859. [DOI] [PubMed] [Google Scholar]
- 47.Dufour J, Viennois E, De Boussac H, Baron S, Lobaccaro JM. Oxysterol receptors, AKT and prostate cancer. Curr Opin Pharmacol. 2012;12:724–728. doi: 10.1016/j.coph.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 48.Maslyanko M, Harris RD, Mu D. Connecting cholesterol efflux factors to lung cancer biology and therapeutics. Int J Mol Sci. 2021;22:7209. doi: 10.3390/ijms22137209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Silvente-Poirot S, Poirot M. Cancer. Cholesterol and cancer, in the balance. Science. 2014;343:1445–1446. doi: 10.1126/science.1252787. [DOI] [PubMed] [Google Scholar]
- 50.Smith B, Land H. Anticancer activity of the cholesterol exporter ABCA1 gene. Cell Rep. 2012;2:580–590. doi: 10.1016/j.celrep.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu K, Zhang W, Tan J, Ma J, Zhao J. MiR-200b-3p functions as an oncogene by targeting ABCA1 in lung adenocarcinoma. Technol Cancer Res Treat. 2019;18:1533033819892590. doi: 10.1177/1533033819892590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huang CX, Zhang YL, Wang JF, Jiang JY, Bao JL. MCP-1 impacts RCT by repressing ABCA1, ABCG1, and SR-BI through PI3K/Akt posttranslational regulation in HepG2 cells. J Lipid Res. 2013;54:1231–1240. doi: 10.1194/jlr.M032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thysell E, Surowiec I, Hörnberg E, Crnalic S, Widmark A, Johansson AI, Stattin P, Bergh A, Moritz T, Antti H, Wikström P. Metabolomic characterization of human prostate cancer bone metastases reveals increased levels of cholesterol. PLoS One. 2010;5:e14175. doi: 10.1371/journal.pone.0014175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Murai T, Maruyama Y, Mio K, Nishiyama H, Suga M, Sato C. Low cholesterol triggers membrane microdomain-dependent CD44 shedding and suppresses tumor cell migration. J Biol Chem. 2011;286:1999–2007. doi: 10.1074/jbc.M110.184010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ramprasad OG, Srinivas G, Rao KS, Joshi P, Thiery JP, Dufour S, Pande G. Changes in cholesterol levels in the plasma membrane modulate cell signaling and regulate cell adhesion and migration on fibronectin. Cell Motil Cytoskeleton. 2007;64:199–216. doi: 10.1002/cm.20176. [DOI] [PubMed] [Google Scholar]
- 56.Plösch T, Gellhaus A, van Straten EM, Wolf N, Huijkman NC, Schmidt M, Dunk CE, Kuipers F, Winterhager E. The liver X receptor (LXR) and its target gene ABCA1 are regulated upon low oxygen in human trophoblast cells: A reason for alterations in preeclampsia? Placenta. 2010;31:910–918. doi: 10.1016/j.placenta.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 57.Ohno Y, Ohori M, Nakashima J, Okubo H, Satake N, Hashimoto T, Tachibana M. Association between preoperative serum total cholesterol level and biochemical recurrence in prostate cancer patients who underwent radical prostatectomy. Mol Clin Oncol. 2016;4:1073–1077. doi: 10.3892/mco.2016.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buchwald H. Cholesterol inhibition, cancer, and chemotherapy. Lancet. 1992;339:1154–1156. doi: 10.1016/0140-6736(92)90744-N. [DOI] [PubMed] [Google Scholar]
- 59.Cerovska E, Elsnerova K, Vaclavikova R, Soucek P. The role of membrane transporters in ovarian cancer chemoresistance and prognosis. Expert Opin Drug Metab Toxicol. 2017;13:741–753. doi: 10.1080/17425255.2017.1332179. [DOI] [PubMed] [Google Scholar]
- 60.Amaar YG, Reeves ME. RASSF1C regulates miR-33a and EMT marker gene expression in lung cancer cells. Oncotarget. 2019;10:123–132. doi: 10.18632/oncotarget.26498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Di Nicolantonio F, Mercer SJ, Knight LA, Gabriel FG, Whitehouse PA, Sharma S, Fernando A, Glaysher S, Di Palma S, Johnson P, et al. Cancer cell adaptation to chemotherapy. BMC Cancer. 2005;5:78. doi: 10.1186/1471-2407-5-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shang Y, Zhang Z, Liu Z, Feng B, Ren G, Li K, Zhou L, Sun Y, Li M, Zhou J, et al. miR-508-5p regulates multidrug resistance of gastric cancer by targeting ABCB1 and ZNRD1. Oncogene. 2014;33:3267–3276. doi: 10.1038/onc.2013.297. [DOI] [PubMed] [Google Scholar]
- 63.Gottesman MM, Fojo T, Bates SE. Multidrug resistance in cancer: Role of ATP-dependent transporters. Nat Rev Cancer. 2002;2:48–58. doi: 10.1038/nrc706. [DOI] [PubMed] [Google Scholar]
- 64.Moitra K. Overcoming multidrug resistance in cancer stem cells. Biomed Res Int. 2015;2015:635745. doi: 10.1155/2015/635745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bachmeier BE, Iancu CM, Killian PH, Kronski E, Mirisola V, Angelini G, Jochum M, Nerlich AG, Pfeffer U. Overexpression of the ATP binding cassette gene ABCA1 determines resistance to Curcumin in M14 melanoma cells. Mol Cancer. 2009;8:129. doi: 10.1186/1476-4598-8-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hou H, Kang Y, Li Y, Zeng Y, Ding G, Shang J. miR-33a expression sensitizes Lgr5+ HCC-CSCs to doxorubicin via ABCA1. Neoplasma. 2017;64:81–91. doi: 10.4149/neo_2017_110. [DOI] [PubMed] [Google Scholar]
- 67.Iwasaki H, Okabe T, Takara K, Yoshida Y, Hanashiro K, Oku H. Down-regulation of lipids transporter ABCA1 increases the cytotoxicity of nitidine. Cancer Chemother Pharmacol. 2010;66:953–959. doi: 10.1007/s00280-010-1247-7. [DOI] [PubMed] [Google Scholar]
- 68.Sun M, Yang C, Zheng J, Wang M, Chen M, Le DQS, Kjems J, Bünger CE. Enhanced efficacy of chemotherapy for breast cancer stem cells by simultaneous suppression of multidrug resistance and antiapoptotic cellular defense. Acta Biomater. 2015;28:171–182. doi: 10.1016/j.actbio.2015.09.029. [DOI] [PubMed] [Google Scholar]
- 69.Chen JH, Zheng YL, Xu CQ, Gu LZ, Ding ZL, Qin L, Wang Y, Fu R, Wan YF, Hu CP. Valproic acid (VPA) enhances cisplatin sensitivity of non-small cell lung cancer cells via HDAC2 mediated down regulation of ABCA1. Biol Chem. 2017;398:785–792. doi: 10.1515/hsz-2016-0307. [DOI] [PubMed] [Google Scholar]
- 70.Ma Y, Li X, Cheng S, Wei W, Li Y. MicroRNA-106a confers cisplatin resistance in non-small cell lung cancer A549 cells by targeting adenosine triphosphatase-binding cassette A1. Mol Med Rep. 2015;11:625–632. doi: 10.3892/mmr.2014.2688. [DOI] [PubMed] [Google Scholar]
- 71.Heilos D, Röhrl C, Pirker C, Englinger B, Baier D, Mohr T, Schwaiger M, Iqbal SM, van Schoonhoven S, Klavins K, et al. Altered membrane rigidity via enhanced endogenous cholesterol synthesis drives cancer cell resistance to destruxins. Oncotarget. 2018;9:25661–25680. doi: 10.18632/oncotarget.25432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wali VB, Bachawal SV, Sylvester PW. Suppression in mevalonate synthesis mediates antitumor effects of combined statin and gamma-tocotrienol treatment. Lipids. 2009;44:925–934. doi: 10.1007/s11745-009-3344-0. [DOI] [PubMed] [Google Scholar]
- 73.Chen W, Li L, Wang J, Zhang R, Zhang T, Wu Y, Wang S, Xing D. The ABCA1-efferocytosis axis: A new strategy to protect against atherosclerosis. Clin Chim Acta. 2021;518:1–8. doi: 10.1016/j.cca.2021.02.025. [DOI] [PubMed] [Google Scholar]
- 74.Srivastava N. ATP binding cassette transporter A1-key roles in cellular lipid transport and atherosclerosis. Mol Cell Biochem. 2002;237:155–164. doi: 10.1023/A:1016506221047. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


