Figure 3.
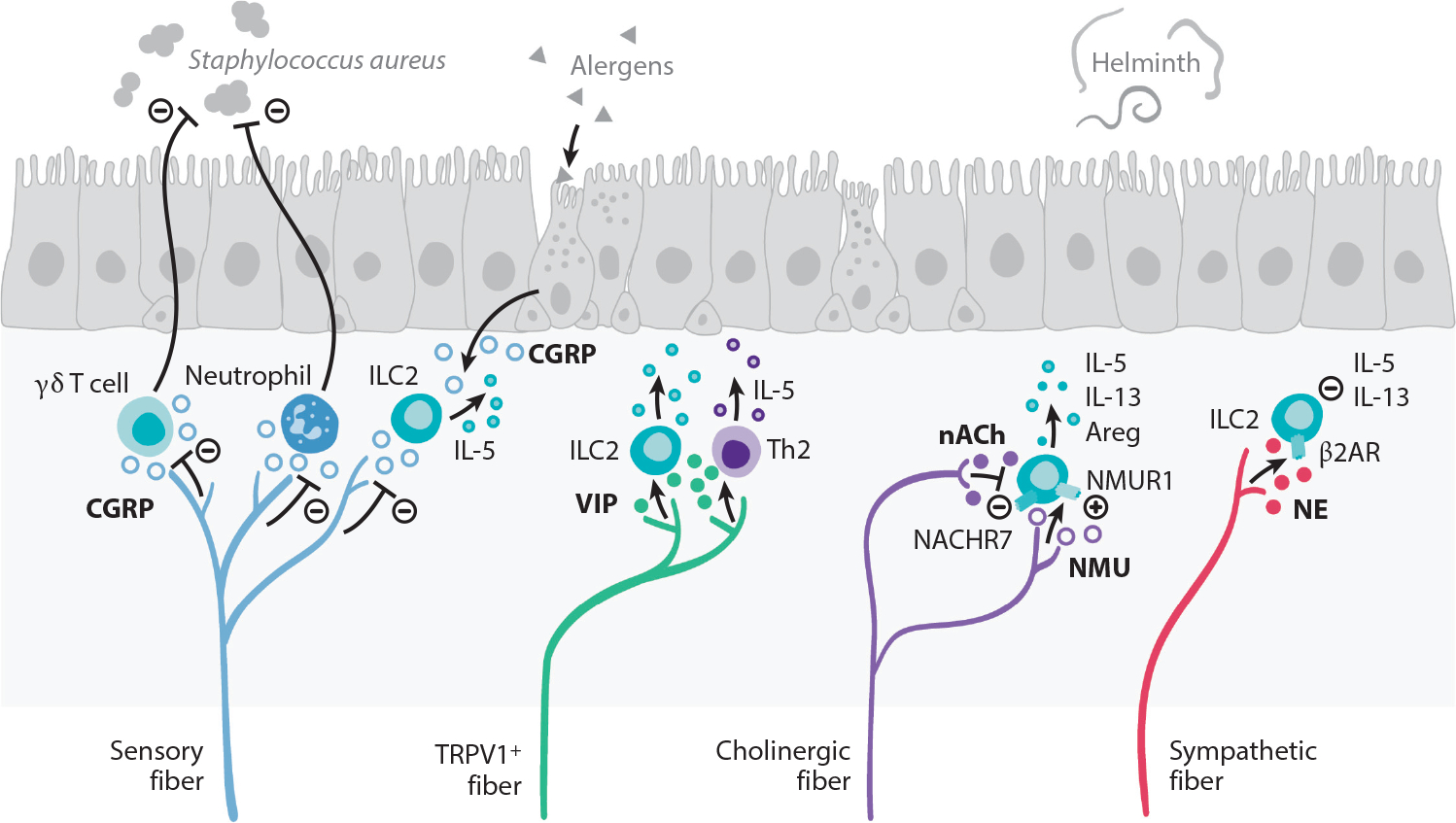
Peripheral neuroimmune interactions in the lungs. The vagus nerve supplies most of the sensory and cholinergic innervation of the airways. Allergic inflammation in the lungs stimulates the production of the type 2 cytokine IL-5 that directly stimulates sensory neurons to release VIP. VIP recruits and activates ILC2s and CD4+ T cells, which further potentiate airway inflammation. TRPV1+ pulmonary fibers restrict antibacterial immunity through secretion of CGRP, which restricts recruitment of neutrophils and γδ T cells. CGRP, released by sensory fibers and neuroendocrine cells that are found interspersed in the lung epithelium, also regulates IL-5 production by ILC2s. Cholinergic fibers release the neuropeptide NMU, which is a potent activator of ILC2s via NMUR1 that responds by producing the type 2 effector cytokines IL-5, IL-13, and Areg that are important for helminth immunity. In turn, acetylcholine inhibits ILC2 function via NACHR7. Sympathetic fibers release NE that acts on β2AR expressed by ILC2s, downmodulating the production of IL-5 and IL-13. Abbreviations: β2AR, β2 adrenergic receptor; Areg, amphiregulin; CGRP, calcitonin gene–related peptide; ILC2, group 2 innate lymphoid cell; NACHR7, nicotinic acetylcholine receptor 7; NE, norepinephrine; NMU, neuromedin U; NMUR1, neuromedin U receptor 1; TRPV1, transient receptor potential cation channel V member 1; VIP, vasoactive intestinal peptide.
