Abstract
Background and aim:
Recently a modification of the DAA in lateral decubitus, called ALDI, has been proposed to obtain a better surgical exposure than DAA in supine decubitus and it easier for surgeons accustomed to the posterolateral (PLA) or direct lateral approach. The aim of this paper was to report our early experience with the ALDI approach for THA and to compare outcomes between ALDI and PLA in a retrospective investigation.
Methods:
From September 2017 to January 2020 we have identified all patients who received THA through the ALDI approach and through the PLA. We collected patients demographic, clinical (HHS and HOOS) and radiographic data by our electronic hospital database. The ALDI group included 60 hips and the PLA group included 219 hips. These patients underwent to strict follow-up in the first 3 post-operative months.
Results:
Compared to the PLA, the ALDI approach showed clinical outcomes significantly higher in the first month of follow-up. The PLA group has a lower operative time and a greater mean hospital length of stay. No blood transfusions were administered in the ALDI group while the 1.4% of patients in the PLA group needed blood transfusion. Cup anteversion and inclination angles were significantly wider in the PLA group. THA dislocation occurred in seven patients of the PLA group. No femoral cutaneus nerve palsy was recorded in the ALDI group.
Conclusions:
The ALDI approach can represent a quickly and safe solution for surgeons who are accustomed to the PLA who want to perform THA in DAA. Our preliminary experience has shown encouraging outcomes in terms of clinical and radiographic parameters although the operative time needs to be improved. (www.actabiomedica.it)
Keywords: Total hip arthroplasty, Direct Anterior Approach, Lateral decubitus, ALDI
Introduction
Direct anterior approach (DAA) for primary total hip arthroplasty (THA) had significantly better outcomes in the early postoperative recovery (1) than the other hip approaches. The DAA for THA is traditionally performed with the patient in the supine position. Surgeons can use a special traction-table to permit the leg’s traction and lowering or a regular operative-table where the leg is placed in figure-four adduction during femoral exposure (2.3). Some reports on this surgical approach showed higher rate of intra-operative and post-operative complications, higher operative time and a long and steep learning curve for surgeons (4,5).
In 2007, Michel et al. introduced anterior approach for THA positioning patients in lateral decubi-tus (MicroHip procedure) (6).
Since 2011, others authors (3,4,7-9) have performed the anterior approach placing patients in the lateral decubitus to minimize feasible complications of DAA in supine position as femoral fractures and lateral femoral cutaneous nerve injury.
In 2019 Carta et al.(7) has proposed the “ALDI (Anterior Lateral Decubitus Intermuscular) Approach” to promote the shift to an anterior approach to the hip among surgeons accustomed to the posterior (Moore or Southern) or direct lateral (Hardinge) hip approaches.
Performing the DAA in lateral decubitus enables to have the acetabulum in the same position of posterolateral approach (PLA), the buttock down for gravity, and an easier exposure of the femur with preservation of the posterior capsule and extrarotators cuff (7).
The previous experiences seem to prove satisfactory implant placement and clinical outcomes of DAA in lateral decubitus (9,10). For this reason, we started in 2017 to perform DAA for THA in the lateral de-cubitus.
The aim of this paper was to report our early experience comparing the THA outcomes between patients’ sample for ALDI approach and standardized results with PLA in a retrospective analysis.
Materials and methods
In September 2017, three senior surgeons (FT, GLB, LD) of our Orthopedics and Traumatology Department that were accustomed to the PLA began to perform “ALDI approach” for THA.
Under the endorsement of our institutional review board, we collected patients’ data by our electronic hospital database and we identified all patients submitted to DAA for THA in lateral decubitus and the PLA group of patients who received THA in pos-terolateral approach. All patients signed an informed consent for the surgical procedure. This study was conducted under the principles of Declaration of Helsinki.
For the ALDI group we have recruited patients with end-stage hip osteoarthrosis, age of 20 to 90 years, BMI < 30 kg/m2.
Other inclusion criteria were patients with a complete follow-up of 3 months and proper radiographs.
Exclusion criteria, instead, included hip dyspla-sia, femoral neck fracture, previous hip surgery, con-trolateral hip pain and osteoarthrosis, neuromuscular disorders, inflammatory arthropathy, and other mus-culoskeletal disorders that prevented early postoperative rehabilitation and weight bearing.
We collected all patients, 55 patients (60 hips), for primary THAs with ALDI experience from September 2017 to January 2020, all after the end of a learning curve of 20 patients.
Thirty-five patients were males and 25 were females, the mean age was 65 years (range 37-82).
In the same period, we performed 219 THA in PLA on 213 patients, 104 patients were males and 115 were females, the mean age was 69.3 years (range 35-85).
Before surgery we performed preoperative planning on pelvic radiographs by means of a software called Sectra 2D Planning System (11,12).
All patients in both groups received press-fit un-cemented cups (Trabecular Metal1; Modular Acetabular System) (13); press-fit Zimmer Biomet’s Taperloc hip system stems were employed in ALDI group for the proximal femur shape to overcome the difficulties of the exposure of the proximal femur and to respect the greater trochanter in broaching and implanty the stem (14,15), while according to Dorr classification we implanted cementless MIA (Smith&Nephew) (for femur type B and C) and CLS (Zimmer Biomet) (for femur type A) stems in PLA group.
No fluoroscopic check was performed during surgery at any time. Every patient received an AP hip and pelvic x-ray control immediately after surgery.
A fast-track protocol was applied to all patients (16,17). Fast-track protocol includes pre-operative patient education, anti-hemetic (dexamethasone) and bleeding profilaxis (tranexamic acid), intraoperative administration of L.I.A. (18) (local infiltration anesthesia) and no drain retention (19), early assisted verticalization and mobilization 2 or 3 hours after surgery and post-operative opioid sparing analgesia by means of elastomeric devices. Clinical and radio-graphic outcomes were assessed by an experienced and well-trained orthopedic surgeon at 15-30-90 days post-operatively. Clinical assessment included Harris Hip Score (20) registration at every follow up assessment, hip disability and osteoarthritis outcome score (HOOS) (21) at one-month follow-up. Operative time (min), intraoperative and postoperative complications, hemoglobin dropping and blood transfusion rate, hospital length of stay (days) were also recorded.
Radiographic measurements for cup orientation were performed on anteroposterior (AP) pelvic radiographs.
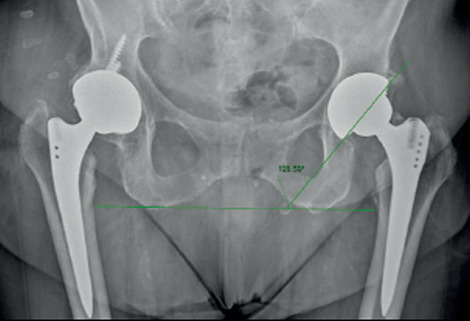
Cup inclination angle was determined as the angle between the line passing through the tip of both ischiatic tuberosity and the line passing through the medial and lateral edges of the cup (Fig. 1) (22).
Figure 1. Cup inclination angle determined on AP pelvic radiographs.
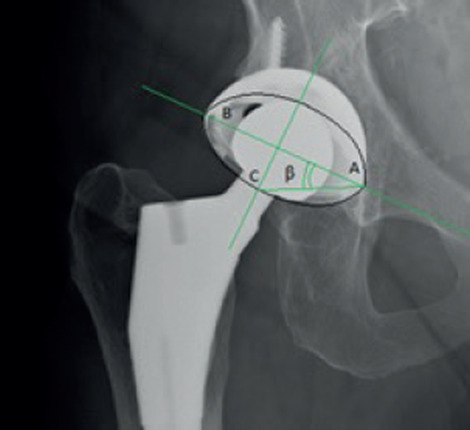
Cup anteversion angle was calculated by means of a trigonometric method developed by Liaw et al. (23). This method estimates cup anteversion of the acetabular component calculated through the trigonometric formula “sin”1 tan P”. P angle is the angle between the long axis of the component and the line connecting the end of AB axis with the end-point of the ellipse (Fig. 2).
Figure 2. Cup anteversion angle determined on AP hip radiographs by means of a trigonometric method developed by Liaw et al.(23).
We accounted target values of 40 ± 10° of cup inclination and 15 ± 10° of cup anteversion defined by Lewinnek et al. (24), although recent analyses have shown the Lewinnek “safe zone” in cup replacement in THA is not always predictive of stability (25).
Moreover, we reviewed femoral stem alignment on a simple AP view radiographs (22).
Statistical methods
We conducted exploratory statistical analysis of frequencies and percentages for categorical variables, means and standard deviations for quantitative data (Table 1).
Table 1. Patients demographic, clinical and radiographic data, and statistical analysis.
| ALDI group | PLA group | Statistical analysisp-value | |
| N° of hips | 60 hips 55 patients, 5 patients with bilateral hips | 219 hips 213 patients, 6 patients with bilateral hips | |
| Mean age | 65 years (37-82) | 69.3 years (35-85) | 0.0036 |
| BMI | 25.6 (20-30) kg/m2 | 25 (17-30) kg/m2 | 0.8284 |
| Male : Female | 35 M ; 25F | 104 M ; 115 F | 0.1366 |
| Hip side R:L | 33 R; 27 L | 120R: 99 L | 0.9774 |
| Diagnosis | 56 hip osteoarthrosis 4 AVN of FH | 198 hip osteoarthrosis 21 AVN of FH | |
| Mean Operative time | 1.49 (1.04-2.51) hours | 1.18 (0:51-2:00) hours | |
| Length of hospital stay | 4.7 (3-7) days | 5.16 (3-9) days | 0.0026* |
| Delta Hb | 3.5 (1.6-6.1) g/dL | 3 (0.6-5.8) g/dL | 0.0002* |
| N° of bloodtrasfusions | 0 | 4 patients 10 bloodbags (6;2;1;1) | - |
| HHS 2 weeks FU | 86.3 (81-97) | 76.4 (60-91) | <.0001* |
| HHS 1 month FU | 94.5 (64-100) | 92.73 (75-99) | 0.0009* |
| HHS 3 months FU | 97.75 (95 -100) | 95.93 (93-100) | 0.3291 |
| HOOS1 month FU | 80.8 (56-95) | 78.2 (44-99.4) | 0.1670 |
| Complications | 4 (6.6%)0 THA Dislocations1 Intraoperativefractures (1.6%) | 16 (7.3%): 3.19% THA Dislocations 0.91% THA Revisions 1.37% Intraoperative fractures | |
| Mean Cup Inclination angle | 30.17 (20-45) degrees | 34.5 (17-57) degrees | 0.0005* |
| Mean Cup anteversion angle | 19.2 (5-43) degrees | 28.3 (6.5-49.5) degrees | <.0001* |
| Mean stem alignment | 0.66 (0-7) degrees | 1.74 (-3;6) degrees | <.0001* |
| *Significancedifference (p < 0.05) | |||
Continuous variables were compared with the Mann-Whitney’s U test and categorical variables using Pearson’s % 2 test. A P-value < 0.05 was accounted statistically significant. All statistical analyses were carried out using the MedCalc statistical software for biomedical research.
Results
Both groups were homogeneous regarding age, gender, BMI, preoperative diagnosis (Table 1). The average operative time was 109 (64-171) minutes in the ALDI group versus 78 (51-120) minutes in the PLA group, average blood loss 3.5 (1.6-6.1) g/dL versus 3 (0.6-5.8) g/dL (p= 0.0002), average hospital length of stay 4.7 (3-7) days versus 5.16 (3-9) days (p=0.0002), respectively. No patient was transfused in the ALDI group while 4 patients (10 blood bags) of the PLA group were transfused. This finding collides with the blood loss data recorded in the two groups. Blood transfusion rate is greater in the PLA group for the following postoperative complications: one case of postoperative haemorrhage from the superior gluteal artery treated by percutaneous embolization after blood transfusion with 6 blood bags; two blood bags were transfused in one case of postoperative hematoma and hypoalbuminemia; one blood bag was transfused in one patient affected by acute renal failure and in one patient who had an hemoglobin level at 7.5 g/dl on the third postoperative day. As a result of these complications they have prolonged hospital length of stay. Regarding hip function, after 15-day follow-up we found the mean HHS to be significantly higher in the ALDI group than in the PLA group, 86.3 (81-97) versus 76.4 (60-91) (p <0.0001). After 1 month, the mean HHS improved in both groups but was still significantly higher in the ALDI group compared to the PLA group, 94.5 (64-100) versus 92.73 (75-99) (p= 0.0009). The two groups were no significantly different in the mean HOOS, 80.8 (56-95) for the ALDI group versus 78.2 (44-99.4) in the PLA group (p= 0.1670). The mean HHS after 3-month follow-up showed no significant differences between the two groups, 97.75 (95 -100) for the ALDI group versus 95.93 (93-100) for the PLA group (p = 0.3291). The incidence of surgical complications was 6.6% (4 patients) in the ALDI group and 7.3% in PLA group (16 patients). Intra-operative femur fractures occurred in one patient belonging to the ALDI group and 3 patients belonging to the PLA group. No lateral femoral cutaneous nerve injury was found in the ALDI group. THA dislocation occurred in seven patients in the PLA group (Table 2), five cases were treated with closed reduction and did not recur. THA revision was necessary in two cases of recurrent dislocations. The mean cup anteversion angle was significantly wider in the PLA compared to the ALDI group (28.3° versus 19.2°, p < 0. 0001). In addition, mean inclination angle was also wider in the PLA group (34.5° versus 30.17°, p= 0.0005). Significant differences were seen also in the stem alignment in AP view radiographs between the two groups, mean 0.66 degrees of varus alignment in the ALDI group versus mean 1.74 degrees varus alignment in the PLA group (p <0.0001).
Table 2. Cup angle values in THA dislocation in the PLA group.
| THA dislocation in the PLA group | Cup Inclination angle | Cup anteversion angle | Treatment |
|---|---|---|---|
| 28° | 34° | conservative | |
| 35° | 26° | conservative | |
| 26° | 33 | conservative | |
| 39° | 26° | conservative | |
| 41.2° | 22.7° | THA revision | |
| 45° | 29° | THA revision | |
| 50° | 21.1° | conservative |
,
Discussion
The DAA remains a suggestive approach in THA for surgeons and patients. The DAA is a tissue-sparing technique as no muscle detachment is necessary, small external rotator tendons are retained, only the anterior aspect of the capsule is excised, and tensor fascia latae (TFL) and rectus femoris muscles are minimally damaged (26).
Moreover, length of stay in hospital was significantly shorter after DAA than the PLA (2.9 days vs 4.0 days) (27). Therefore, DAA shows earlier restoration of THA function compared to PLA approach.
The randomized controlled trials (28,29,30) demonstrated no difference in functional outcomes at 6 weeks postoperatively in both approaches. Taunton et al.(30) showed the time to discontinue the walker use and time to discontinue all gait aids was 17 vs 24 days for DAA and PLA, respectively. Other authors reported HOOS Symptoms score and the HHS percent walking unlimited distance remains significantly higher in DAA at three months postoperatively and there were no significant differences in outcomes between surgical approaches at later time points (1,31).
Recent investigations introduced a modification of the DAA, placing patients in the lateral decubitus. ALDI approach resolves the absence of a special operating room table, permits a more accurate cup orientation compared to PLA, helping surgeons accustomed to other surgical approaches to decide to perform THA in
As far as we know, this is one of few studies that compares THA clinical outcomes and implant alignment between ALDI and PLA approaches.
The present study assessed the patients in both groups during 3 months after surgery to check in early postoperative outcome differences. The study revealed that the mean HHS score was significantly higher in ALDI group than in the PLA group at 15 days and 30 days after surgery, while the HHS score showed no significant differences between the two groups at the final follow-up. At 1-month follow-up, the HOOS score was not statistically different between the two groups.
Operative time in the ALDI group appeared higher compared to the PLA group despite the already completed learning curve. Perioperative complications occurred in 2 patients from the ALDI group and 3 patients from the PLA group. Postoperative complications occurred in 2 patients from the ALDI group and 13 patients from the PLA group. In the PLA group 1 patient had traumatic periprosthetic fractures 10 days after surgery.
In literature, the DAA shows a lower dislocation rate (0.6-1.5%) compared to PLA (mean, 6.9%) (32).
In our series, THA dislocation occurred only in 7 patients from the PLA group. It was treated with closed reduction in 5 patients and did not recur, but 2 patients had a recurrent hip dislocation that required revision surgery.
Lateral femoral cutaneous nerve injury is a feasible complication of DAA. The risk of nerve injury ranging from 0.61% to 67% is due to excessive traction of the soft tissues. In the current study we didn’t observe lateral femoral cutaneous nerve injury in the ALDI group.
In our series, the cup anteversion angle was closer to the Lewinnek target in the ALDI group than in the PLA group.
Based on previous experiences, the ALDI approach might offer better acetabular exposure, preparation and placement than PLA. Moreover, it allows to expend less effort to expose the femur than the patient in supine placement during surgery avoiding stem implant in flexion or posterior femoral cortex fracture (10).
Fei Hu et al.(10) in their series showed that the cup anteversion angle was significantly higher in the DAA compared to the PLA group, while the difference of inclination angle between the two groups was not meaningful.
According to Lewinnek criteria, in our study, cup had successful inclination angle in all ALDI THA and in 210 PLA THA (95.89%), while cup anteversion angle was oriented correctly in 48 ALDI THA (80%) and 66 PLA THA (30.14%).
The frequency of the safe zone in acetabular placement tended to be more favourable in the ALDI group than in the PLA group, indicating that ALDI approach can achieve a more accurate cup orientation.
Out of 7 dislocations in the PLA group, two THAs were in the normal range of Lewinnek criteria, one of which underwent to revision surgery; two THAs had both inclination and anteversion angle out of Lewinnek range; 3 THAs had anteversion angle only out of Lewin-nek range, one of which underwent to revision surgery.
Currently, the Lewinnek safe zone is known not to be always predictive of stability after THA. Our series, indeed, shows how THA dislocations also occurred in the safe zone of Lewinnek.
Stem alignment in the AP plane was significantly better in the ALDI group than in the PLA group (<0.0001), but different hip stems were implanted in the two groups.
Our results show satisfactory clinical and radio-graphic outcomes of the ALDI approach with acceptable complication rate. Analyzing the other experiences (Table 3) on DAA in lateral decubitus, we showed better clinical results after 1 month (HHS 94.5 VS 82.1) (3) and 3 months (HHS 97.75 VS 86) (3), an acceptable complication rate, 6.6% (ranging between 3.6-42.7%) (3,4,7,9,10) with zero cases of THA dislocation (ranging between 0-1.7%), no lateral femoral cutaneous nerve injury (ranging between 0-36.75%) and zero transfusion rates (0 VS 9.3%) (7). Unlike the other authors, we reported a higher operative time (median time 107 min VS 82 min (9); mean time 109 min VS 51.38 min.) (7), while the average hospital length of stay was in line with the other studies (4.7 days VS 3 and 5 days) (7,9). Compared to the radiographic outcomes of the other authors, the mean cup inclination was lower, while the mean cup anteversion was higher, but its calculation was performed with different methods. Stem position was neutral in 90% of cases (ranging between 91.8-99.2%) (3,4,10). This study has several limitations. The major differences are the size of the two groups, the different hip stems implantation in the two groups, and the lack of a randomized study design. Moreover, the radiological evaluation includes cup and stem orientation on AP x-ray. Only CT scan could provide a more reliable analysis, but it exposes patients to more radiation.
Table 3. Comparison of other paper outcomes related to anterior approach and lateral decubitus from biomedical literature.
| Cup Inclination angle (degrees) | Cup Anteversion angle (degrees) | Neutral Rate of stem Total alignment complications | THA Dislocations | Lateral Femoral cutaneus nerve injury | Intraoperative fractures | Lengthofhospital stay | Blood trasfusions | Operative time | HHS HHS1 3month months | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| elman et al. 2015 | 49° | 13°Calculated with Lu method | _ 9.9% | 1.65% | 0 | 2.75% | 3 days | _ | Median time 82 min | _ | _ |
| Chenet al. 2017 | 43.5° | 16.5° Calculated with Lewinnek method | 95.7% 42.7% | 1.7% | 36.75% | 0.85% | 82.1 | 86 | |||
| Camenzid et al. 2018 | <35°: 10.9%35-40°: 32.6% 41-45°:40.6% 46-50°:14.5%>50°: 1.4% | <10°: 8.7%10-15°: 60.1%>15°: 31.2% Calculated with Widmer method | 99.2% 3.6% | 0 | 0 | 1.45% | |||||
| Carta et al. 2019 | _ | _ | 4.66% | 0.8% | 0.6% | 0 | 5 days | 9.3% | Mean time 51.38 min | _ | _ |
| FeiHu et al. 2020 | 41.17° | 13.92° Calculated with Widmer method | 91.8% 21% | 0 | 12.7% | 3.6% | |||||
| Niccoli et al. 2021 | 30.17° (20-45) | 19.2° (5-43) Calculated with Liaw method | 90% 6.6% | 0 | 0 | 1.66% | 4.7 days | 0 | Median time107min;Mean time109 min | 94.5 | 97.75 |
Conclusions
Nevertheless, the ALDI approach can represent a quick and safe solution for surgeons accustomed to other approaches who want to perform THA in DAA. Our early results are promising and show that ALDI is a reliable surgical approach, but for the above-mentioned reasons further and extensive investigations with larger samples and a longer surgical experience are needed.
Conflict of Interest:
Each author declares that he has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article. No study design protocol approved by the IRB was necessary for this study, as a standard and approved technique was applied and no sensible data are presented.
References
- Maldonado DR, Laseter JR, Kyin C, Lall AC, Domb BG. Direct Anterior Approach in Total Hip Arthroplasty Leads to Superior Outcomes at 3-Month Follow-up When Compared With the Posterior Approach: A Matched Study Using Propensity Score Analysis. J Am Acad Orthop Surg Glob Res Rev. 2019 Dec;23(3(12)):e19. doi: 10.5435/JAAOSGlobal-D-19-00118. 00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galakatos GR. Direct Anterior Total Hip Arthroplasty. MoMed. 2018 Nov-Dec;115(6):537–541. [PMC free article] [PubMed] [Google Scholar]
- Chen M, Luo Z, Ji X, Cheng P, Tang G, Shang X. Direct Anterior Approach for Total Hip Arthroplasty in the Lateral Decubitus Position: Our Experiences and Early Results. J Arthroplasty. 2017 Jan;32(1):131–138. doi: 10.1016/j.arth.2016.05.066. [DOI] [PubMed] [Google Scholar]
- Camenzind RS, Stoffel K, Lash NJ, Beck M. Direct anterior approach to the hip joint in the lateral decubitus position for joint replacement. Oper Orthop Traumatol. 2018 Aug;30(4):276–285. doi: 10.1007/s00064-018-0550-z. [DOI] [PubMed] [Google Scholar]
- Stone AH, Sibia US, Atkinson R, Turner TR, King PJ. Evaluation of the Learning Curve When Transitioning From Posterolateral to Direct Anterior Hip Arthroplasty: A Consecutive Series of 1000 Cases. J Arthroplasty. 2018 Aug;33(8):2530–2534. doi: 10.1016/j.arth.2018.02.086. [DOI] [PubMed] [Google Scholar]
- Michel MC, Witschger P. MicroHip: a minimally invasive procedure for total hip replacement surgery using a modified Smith-Peterson approach. Ortop Traumatol Rehabil. 2007 Jan-Feb;9(1):46–51. [PubMed] [Google Scholar]
- Carta S, Fortina M. ALDI (Anterior Lateral Decubitus Intermuscular) approach to the hip: Comprehensive description of the surgical technique with operative video. Orthop Traumatol Surg Res. 2019 Sep;105(5):923–930. doi: 10.1016/j.otsr.2019.02.026. [DOI] [PubMed] [Google Scholar]
- Sendtner E, Schuster T, Wörner M, Kalteis T, Grifka J, Renkawitz T. Accuracy of acetabular cup placement in computerassisted, minimally-invasive THR in a lateral decubitus position. Int Orthop. 2011;35(6):809–815. doi: 10.1007/s00264-010-1042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melman WPR, Mollen BP, Kollen BJ, Verheyen CCPM. First Experiences with the Direct Anterior Approach in Lateral Decubitus Position: Learning Curve and 1 Year Complication Rate. HIP International. 2015;25(3):251–257. doi: 10.5301/hipint.5000221. [DOI] [PubMed] [Google Scholar]
- Hu F, Shang X, Zhang X, Chen M. Direct anterior approach in lateral position achieves superior cup orientation in total hip arthroplasty: a radiological comparative study of two consecutive series. Int Orthop. 2020 Mar;44(3):453–459. doi: 10.1007/s00264-019-04461-4. [DOI] [PubMed] [Google Scholar]
- Sectra 2D Planning System for orthopaedics | SectraMedical [Google Scholar]
- Opperer M, Lee YY, Nally F, BlanesPerez A, Goudarz-Mehdikhani K, Gonzalez Della Valle A. A critical analysis of radiographic factors in patients who develop dislocation after elective primary total hip arthroplasty. Int Orthop. 2016 Apr;40(4):703–8. doi: 10.1007/s00264-015-3022-1. [DOI] [PubMed] [Google Scholar]
- Matharu GS, Judge A, Murray DW, Pandit HG. Trabecular Metal Acetabular Components Reduce the Risk of Revision Following Primary Total Hip Arthroplasty: A Propensity Score Matched Study From the National Joint Registry for England and Wales. J Arthroplasty. 2018 Feb;33(2):447–452. doi: 10.1016/j.arth.2017.08.036. [DOI] [PubMed] [Google Scholar]
- Molli RG, Lombardi AV Jr, Berend KR, Adams JB, Sneller MA. A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin Orthop Relat Res. 2012 Feb;470(2):450–61. doi: 10.1007/s11999-011-2068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khemka A, Mograby O, Lord SJ, Doyle Z, Al Muderis M. Total Hip Arthroplasty by the Direct Anterior Approach Using a Neck-preserving Stem: Safety, efficacy and learning curve. Indian J Orthop. 2018 Mar-Apr;52(2):124–132. doi: 10.4103/ortho.IJOrtho_314_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002 Jun;183(6):630–41. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- Husted H, Jensen CM, Solgaard S, Kehlet H. Reducedlength of stay following hip and knee arthroplasty in Denmark 2000-2009: from research to implementation. ArchOrthop Trauma Surg. 2012 Jan;132(1):101–4. doi: 10.1007/s00402-011-1396-0. [DOI] [PubMed] [Google Scholar]
- Andersen LO, Kehlet H. Analgesic efficacy of local infiltration analgesia in hip and knee arthroplasty: a systematic review. Br J Anaesth. 2014 Sep;113(3):360–74. doi: 10.1093/bja/aeu155. [DOI] [PubMed] [Google Scholar]
- Di Benedetto P, Zangari A, Magnanelli S. Heterotopic Ossification in Primary Total Hip Arthroplasty: which his the role of drainage? Acta Biomed. 2019;90(1-S):92–97. doi: 10.23750/abm.v90i1-S.8077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969 Jun;51(4):737–55. [PubMed] [Google Scholar]
- Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Muscu-loskelet Disord. 2003 May;30(4):10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanrusselt J, Vansevenant M, Vanderschueren G, Vanhoenacker F. Postoperative radiograph of the hip arthroplasty: what the radiologist should know. Insights Imaging. 2015 Dec;6(6):591–600. doi: 10.1007/s13244-015-0438-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park YS, Shin WC, Lee SM, Kwak SH, Bae JY, Suh KT. The best method for evaluating anteversion of the acetabular component after total hip arthroplasty on plain radiographs. J Orthop Surg Res. 2018 Apr;2(13(1)):66. doi: 10.1186/s13018-018-0767-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978 Mar;60(2):217–20. [PubMed] [Google Scholar]
- Tezuka T, Heckmann ND, Bodner RJ, Dorr LD. Functional Safe Zone Is Superior to the Lewinnek Safe Zone for Total Hip Arthroplasty: Why the Lewinnek Safe Zone Is Not Always Predictive of Stability. J Arthroplasty. 2019 Jan;34(1):3–8. doi: 10.1016/j.arth.2018.10.034. [DOI] [PubMed] [Google Scholar]
- Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006 Dec;453:293–8. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- Martin CT, Pugely AJ, Gao Y, Clark CR. A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplasty. 2013 May;28(5):849–54. doi: 10.1016/j.arth.2012.10.029. [DOI] [PubMed] [Google Scholar]
- Christensen CP, Jacobs CA. Comparison of Patient Function during the First Six Weeks after Direct Anterior or Posterior Total Hip Arthroplasty (THA): A Randomized Study. J Arthroplasty. 2015 Sep;30(9 Suppl):94–7. doi: 10.1016/j.arth.2014.12.038. [DOI] [PubMed] [Google Scholar]
- Rykov K, Reininga IHF, Sietsma MS, Knobben BAS, TenHave BLEF. Posterolateral vs Direct Anterior Approach in Total Hip Arthroplasty (POLADA Trial): A Randomized Controlled Trial to Assess Differences in Serum Markers. J Arthroplasty. 2017 Dec;32(12):3652–3658. doi: 10.1016/j.arth.2017.07.008. e1. [DOI] [PubMed] [Google Scholar]
- Taunton MJ, Trousdale RT, Sierra RJ, Kaufman K, Pagnano MW. John Charnley Award: Randomized Clinical Trial of Direct Anterior and Miniposterior Approach THA: Which Provides Better Functional Recovery? Clin Orthop Relat Res. 2018 Feb;476(2):216–229. doi: 10.1007/s11999.0000000000000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013 Oct;28(9):1634–8. doi: 10.1016/j.arth.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 32 Falez F, Papalia M, Favetti F, Panegrossi G, Casella F, Mazzotta G. Total hip arthroplasty instability in Italy. IntOrthop. 2017 Mar;41(3):635–644. doi: 10.1007/s00264-016-3345-6. [DOI] [PubMed] [Google Scholar]


