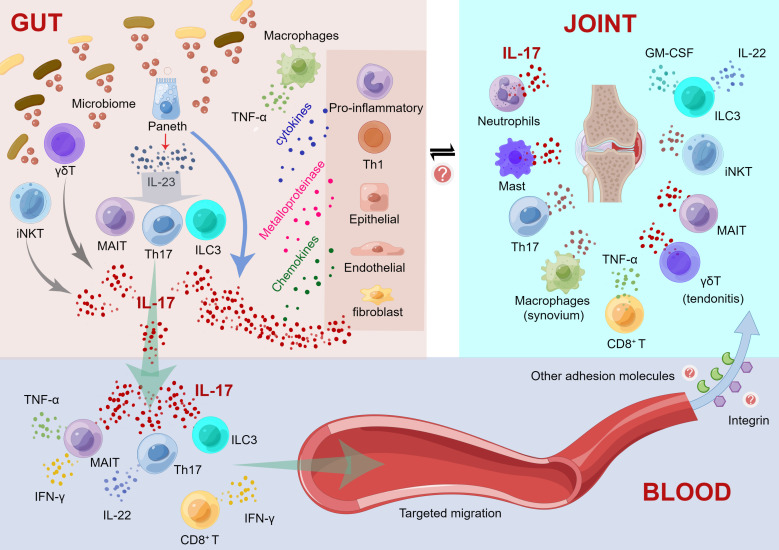
Figure 1.
Mechanistic model regarding the intestinal inflammation driving immune damage in peripheral joints. (1) Immunological changes in the gut. a) Activated Paneth cells produce IL-23 and IL-17 after recognizing the altered microbiome; IL-23 causes the differentiation of Th17, ILC3 and MAIT cells; and these activated cells foster the production of elevated levels of IL-17. IL-17 acts as an inflammatory mediator to stimulate the production of cytokines by other proinflammatory cells and Th1 cells and promotes the production of metalloproteinases and chemokines by macrophages, epithelial cells, endothelial cells, and fibroblasts, thereby triggering and maintaining inflammation. b) γδ T and iNKT cells can recognize microbial antigens and release IL-17. c) Simultaneously, macrophage recruitment promoted the secretion of TNF-α. (2) Cytokine cascades initiated in blood vessels. a) IL-17, Th17 cells, ILC3 and MAIT cells can migrate through the intestinal mucosal barrier to the blood, and these cells may transfer inflammation to the joints. b) Th17, γδT, ILC3 cells and MAIT cells are induced to produce IL-17 in the bloodstream; Th17 cells also produce IL-22. c) MAIT cells also contribute to the production of TNF-α and IFN-γ. d) CD8+ T cells produce IFN-γ. (3) Targeting migration and immune response of extraintestinal joint sites. a) Activated cytokines migrate to inflammatory sites, such as the axial/peripheral joints, for immune interference. b) Some adhesion molecules, such as integrins, may contribute to the target migration of these immune cells circulating in the blood to peripheral joints. c) In peripheral joints, neutrophils, mast cells, Th17 cells, CD8+ T cells, MAIT cells and iNKT cells induce IL-17 production. ILC3 cells produce IL-22 and GM-CSF, whereas IL-17 is only produced in axial joints. d) γδT cells promote tendonitis through elevated IL-17. e) Macrophages induce TNF-α production in the synovium. This figure was drawn by Figdraw.