Abstract
Background
Brain tumor related epilepsy (BTRE) is a common complication of cerebral tumors and its incidence is highly dependent on the type of tumor, ranging from 10–15% in brain metastases to > 80% in low grade gliomas. Clinical management is challenging and has to take into account aspects beyond the treatment of non-tumoral epilepsy.
Main body
Increasing knowledge about the pathophysiology of BTRE, particularly on glutamatergic mechanisms of oncogenesis and epileptogenesis, might influence management of anti-tumor and BTRE treatment in the future. The first seizure implies the diagnosis of epilepsy in patients with brain tumors. Due to the lack of prospective randomized trials in BTRE, general recommendations for focal epilepsies currently apply concerning the initiation of antiseizure medication (ASM). Non-enzyme inducing ASM is preferable. Prospective trials are needed to evaluate, if AMPA inhibitors like perampanel possess anti-tumor effects. ASM withdrawal has to be weighed very carefully against the risk of seizure recurrence, but can be achievable in selected patients. Permission to drive is possible for some patients with BTRE under well-defined conditions, but requires thorough neurological, radiological, ophthalmological and neuropsychological examination.
Conclusion
An evolving knowledge on pathophysiology of BTRE might influence future therapy. Randomized trials on ASM in BTRE with reliable endpoints are needed. Management of withdrawal of ASMs and permission to drive demands thorough diagnostic as well as neurooncological and epileptological expertise.
Keywords: Brain tumor related epilepsy, Antiseizure medication, Glioma, Brain metastasis
Background
Primary brain tumors account for about 1.6% of all cancers [1]. Incidence of primary malignant and non-malignant brain tumors was 23.79 per 100,000 inhabitants per year in the U.S. for the years 2013–2017 (data from the central brain tumor registry of the United States, CBTRUS) [2]. Brain metastasis occur in about 25% of solid tumors [3]. The risk of brain tumor related epilepsy (BTRE) is highly dependent on tumor histology. Patients with diffuse low-grade gliomas suffer from BTRE in > 80% of cases [4, 5], while 62–68% patients with glioblastomas [6, 7] and 40–47% of patients with meningiomas [8, 9] have seizures. In patients with brain metastases the frequency of BTRE is 10–15% [10, 11].
Frontal, parietal and temporal localization of the brain tumor is reportedly associated with a higher risk of seizures compared to occipital localization [12, 13]. In patients with brain metastases, > 4 metastases, high risk location of metastases (defined as frontal, parietal, temporal, or occipital cortex) and melanoma as the primary tumor are risk factors for the occurrence of BTRE [11]. BTRE has a negative impact on quality of life [14]. In this review, an overview of the pathophysiology of BTRE is given. Rational antiseizure medication (ASM) after the first seizure, in case of persistent seizures and in refractory BTRE is discussed (taking into account possible anti-tumor effects of ASM). Further, the duration of ASM and clinical management concerning fitness to drive are addressed in this article. We do not discuss the role of tumor specific treatment (surgery, radiotherapy, chemotherapy) for the reduction of seizure frequency. We neither address the topic of prophylactic ASM in seizure free brain tumor patients.
Main text
Pathophysiology of BTRE: what the clinician needs to know
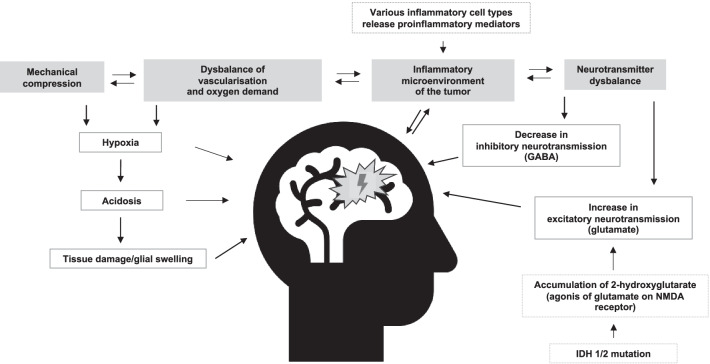
Multiple mechanisms driving the pathophysiology of BTRE have been described. Mechanical compression, imbalance of vascularization and oxygen demand of the tumor, inflammatory processes and neurotransmitter dysbalance play the major roles in epileptogenesis in brain tumor patients (Fig. 1).
Fig. 1.
Overview of mechanisms driving brain tumor related epilepsy (simplified)
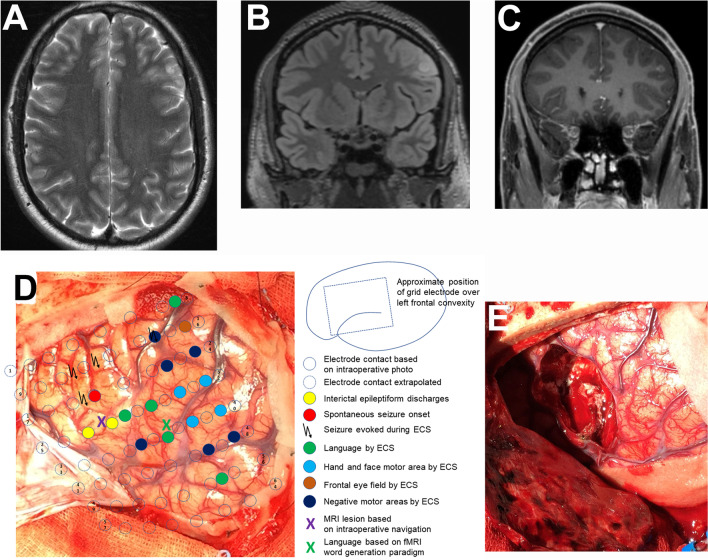
Changes in neurotransmitter balance lead to epileptogenicity of the tumor itself as well as of the tissue adjacent to the lesion, which means that the “epileptogenic zone” [15] includes the peritumoral tissue. Thus, even a complete resection of a brain tumor does not necessarily mean that the epileptogenic zone has also been removed, since a relevant part of seizures in BTRE is generated by the surrounding tissue (Fig. 2).
Fig. 2.
Brain tumor in the left middle frontal gyrus with cortical and subcortical T2/FLAIR hyperintense signal (A, B) and partial Gadolinium enhancement (C) in a 24-year-old male patient. A Axial T2, B coronal FLAIR, C coronal T1 with Gadolinium, D intraoperative situs with superimposed results from extraoperative subdural electrode recording and direct cortical stimulation, E intraoperative situs following resection of the tumor and adjacent epileptogenic area (histology: angiocentric glioma WHO grade 1).
Figure modifed from Wehner et al. [85]
Mechanical compression may induce ischemia and metabolic changes with subsequent blood brain barrier disruption leading to a higher risk of seizures. The vascular supply of brain tumors is often unbalanced and insufficient for the oxygen demand of the tumor and the peritumoral region, leading to hypoxia of the tissue and subsequently to acidosis, glial swelling and tissue damage. These factors contribute to epileptogenesis in brain tumor patients [16].
Inflammatory processes play an important role in oncogenesis and malignant progression of brain tumors through various mechanisms [17]. On the other hand, an interplay of inflammation and occurrence of seizures has been repeatedly reported. While brain inflammation can induce seizures, recurrent or ongoing seizure activity can maintain chronic inflammation [18, 19]. In this context, it is of note that immune checkpoint inhibitors, which reinforce antitumor activity of the immune system, might also lead to a higher risk of status epilepticus. In a retrospective analysis an increasing number of status epilepticus in brain metastasis patients had been observed since the approval and increasing use of immune checkpoint inhibitors [20].
The influence of neurotransmitter imbalance on epileptogenesis in BTRE, in particular a decrease in inhibitory GABA-ergic neurotransmission and an increase in excitatory glutamatergic synaptic input, has been shown in several preclinical and clinical studies [21]. Further, within the last decade, several studies supporting an overlap of mechanisms involved in oncogenesis as well as in epileptogenesis have been published [22, 23]. One fundamental finding was the ability of glioma and breast cancer brain metastasis cells to integrate into neuronal circuits. Gliomas are able to form microtubes, which are thin tubes with membranes, that look like axonal and dendritic growth of developing neurons. On the surface of these microtubes functional synapses between neurons and glioma cells (neurogliomal synapses) were found that communicate via postsynaptic currents mediated by α-Amino-3-hydroxy-5-methylisoxazol-4-propionsäure (AMPA) glutamate receptors [24, 25]. Further, breast cancer brain metastasis [26] and glioma cells [24] were able to form tripartite glutamatergic synapses of cancer cells and pre- and postsynaptic neuron. Perturbation of the glutamatergic pathways in functional neurogliomal synapses as well as perturbation of the indirect perisynaptic communication of neurons and breast cancer cells led to a reduction of invasive growth and slower proliferation of the tumor cells in preclinical studies. This implies that seizure activity can induce brain tumor proliferation [24, 26]. Conversely, glioma progression can lead to neuronal hyperexcitability, which is a typical feature of epilepsy [27]. In line with these findings, median overall survival of patients with brain metastases or glioblastomas and status epilepticus was inferior to that of patients with the same diseases without status epilepticus in a retrospective analysis on 1792 patients (742 meningiomas, 249 glioblastomas, 801 brain metastases) [28]. In this study, the OS of brain metastasis patients with BTRE was significantly inferior to that of patients without epilepsy. An influence of BTRE on overall survival was not found for patients with glioblastoma or meningioma. It is of note that for patients with meningiomas, synapses between neurons and tumor cells have not been not reported [24].
The interplay of neurons and brain tumor cells implies on the one hand a possible role of seizures to promote brain tumor progression and on the other hand potential therapeutic targets to treat both tumor and BTRE [27]. One of the possible therapeutic targets is an inhibition of the AMPA signaling via α-Amino-3-hydroxy-5-methylisoxazol-4-propionsäure receptor (AMPAR) inhibitors. While talampanel, a non-competitive AMPAR inhibitor, has not found its way into clinical practice due to its unfavorable pharmacokinetic profile [29], perampanel, also a non-competitive AMPAR inhibitor, is an approved and increasingly used medication in focal epilepsies. Randomized placebo controlled clinical trials on the use of perampanel in brain tumor patients have not been published to date, but are planned for the foreseeable future. A different approach of targeting glutamatergic mechanisms might be blocking of the overexpression of the cystine-glutamate transporter (xCT), which is common in glioma cells. The xCT exchanges intracellular glutamate for extracellular cystine, thus upregulating both, extracellular glutamate and intracellular cystine, which is used by glioma cells for production of the antioxidant glutathione. Sulfasalazine is a drug able to block the overexpression of xCT, however, data evaluating the use of this drug in clinical practice is lacking [30]. Further, drugs that target the receptor PPAR-λ (e.g., glitazones) are able to induce amino acid transporters on astrocyte membranes, which increases reuptake of glutamate from the extracellular space. These drugs have also shown potential to diminish tumor growth in the preclinical setting [30].
Aberrant GABA signaling leads to accumulation of chloride in glioma cells, which influences both epileptogenicity and oncogenesis. Dysfunction of the mammalian target of rapamycin (mTOR) pathway can lead to modification of glutamate and GABA signaling. Both mechanisms might be potential targets for concomitant treatment of the tumor and of BTRE [30].
Of the molecular markers, which are of increasing importance for treatment decisions in glioma patients, isocitrate-dehydrogenase isoenzyme 1 or 2 (IDH 1/2) is to date the only marker that has been reported to be associated with a higher incidence of seizures. Several clinical studies have shown that an IDH 1/2 mutation confers a risk for preoperative [31, 32] and perioperative [33] seizures in brain tumors. The IDH 1/2 mutation leads to a loss of the ability of the IDH to catalyze the conversion of isocitrate to α-ketoglutarate and further results in a gain of the ability of the IDH to catalyze the reduction of α-ketoglutarate to 2-hydroxyglutarate [34]. This mechanism leads to an accumulation of 2-hydroxyglutarate, which has structural similarity to glutamate and is able to activate the NMDA receptor, therefore acting as a glutamate agonist. A higher glutamate level results in a higher seizure probability. This agonistic mechanism explains the epileptogenic potential of the IDH mutations [35]. While IDH mutations were associated with the occurrence of seizures in a cohort of 442 glioma patients with preoperative seizures in China, p53 expression, ATRX loss, MGMT gene promotor methylation, TERT promoter mutation and 1p/19q co-deletion status were not associated with a higher risk of seizures in this retrospective analysis [36].
Management of BTRE after first seizure
In brain tumor patients, the occurrence of one seizure implies the diagnosis of epilepsy [37]. As brain tumors may grow continuously over time (according to the tumor type), the concept of acute symptomatic seizures does not apply for brain tumor patients. Thus, ASM are usually initiated after the first seizure according to the general recommendations of the International League against Epilepsy (ILAE). Histology, grading, location and molecular markers of the tumor currently do not play a role for the choice of ASM [38]. For valproic acid (VPA) [7, 39–41] and levetiracetam [42, 43], several clinical studies had suggested an antineoplastic effect in patients with glioblastomas, however, a combined metanalysis of four prospective trials did not confirm this effect [44]. Small series on the antiseizure effectivity of perampanel in BTRE have been published [45], clinical studies on its influence on oncogenesis and tumor proliferation are planned for the future. Thus, ASMs in BTRE at present should be chosen based on their pharmacokinetic and pharmacodynamic properties, tolerability and side effects and not for a possible anti-tumor effect. Consensus exists that non-enzyme inducing ASMs should be preferred to enzyme inducing ASMs to avoid interference with antineoplastic and other drugs (e.g., dexamethasone) [38]. Non-enzyme inducing drugs commonly used as monotherapy are: lacosamide (LCM), lamotrigine (LTG), levetiracetam (LEV), topiramate (TPM), valproic acid (VPA) and zonisamide (ZNS) [46]. Larger series (> 25 patients) on GBP and ZNS use in BTRE are lacking. For the other ASMs an overview of studies in BTRE that reported results for each drug is given in Table 1.
Table 1 .
Overview of studies on lacosamide, lamotrigine, levetiracetam, topiramate and valproic acid in brain tumor related epilepsy (studies that included ≥ 25 patients on adults with ≥ 3 months observation time)
| Article | No. of patientsa | Study design | Type of tumor | Mono-/polytherapy | Follow-up (months) | Outcome/main endpoints |
|---|---|---|---|---|---|---|
| Lacosamid | ||||||
| Maschio et al. (2017) [57] | 25 | Pros |
Glioma “High-grade” n = 12 “Low-grade” n = 13 |
Poly | 5.8 (mean) |
Seizure free at final follow-up: 28% Reduction of seizures ≥ 50%: 48% (additional to seizure free patients) |
| Mo et al. (2022) [63] | 132 | Retro | Primary brain tumor | Mono | Follow up at 3 and 6 months |
3-months seizure-free: 64.4% 6-months seizure-free: 55% |
| Van Opijnen et al. (2021)b [48] | 78 | Retro |
Glioma Grade 2 (n = 31) Grade 3 (n = 11) Grade 4 (n = 36) |
Poly (71%) | Maximum of 36 months |
12-months cumulative incidence of treatment failure: 30% 12-months cumulative incidences of treatment failure uncontrolled seizures: 11% 12-months cumulative incidences of treatment failure due to adverse events: 19% |
| Ruda et al. (2017) [58] | 71 | Pros |
Glioma Grade 2 (n = 26) Grade 3 (n = 20) Grade 4 (n = 25) |
Poly | Follow-up at 3, 6, 9 months |
3-, 6- and 9-months seizure reduction ≥ 50%: 74.6, 76.0, 86.2% (including seizure free patients) 3-, 6- and 9-months seizure free: 42.2, 43.0, 50% |
| Ruda et al. (2020) [59] | 93 | Pros |
Glioma “Low-grade” (n = 84) Grade 3 (n = 1) Suspected glioma (n = 3) Meningeoma (n = 3) Other (n = 2) |
Poly | 6 months observation |
6-months seizure reduction ≥ 50%: 76.7% 6-months improvement of Patient’s Global Impression of Change (PGIC): 64.5% 6-months seizure-free: 34.9% |
| Saria et al. (2013) [60] | 70 | Retro |
Glioma Grade 2 (n = 25) Grade 3 (n = 12) Grade 4 (n = 28) Meningeoma (n = 3) Other (n = 2) |
Poly | 6.2 (median) |
Decrease in seizures: 66% 6-months seizure reduction ≥ 50%: 54% No reported toxicities: 77% |
| Sepulveda-Sanchez et al. (2016) [61] | 39 | Retro |
Primary brain tumor (n = 31) Metastasis (n = 7) Not reported (n = 1) |
Poly | Follow-up at 3 and 6 months |
6-months reduction of seizure frequency from 26.4 (mean) to 9.4 (mean) Adverse event: 12% |
| Villanueva et al. (2016) [62] | 105 | Retro |
“Astrocytoma” (n = 42) Glioblastoma (n = 13) Brain metastasis (n = 11) Meningioma (n = 11) Oligodendroglioma (n = 7) Ganglioglioma (n = 6) Oligoastrocytoma (n = 5) DNET (n = 3) Other (n = 4) |
Poly | 6 months observation |
6 months seizure-free: 30.8% 6-months seizure reduction ≥ 50%: 66.3% (including seizure free patients) Adverse events: 41.9% |
| Lamotrigin | ||||||
| Van Opijnen et al. 2021b [48] | 61 | Retro |
Glioma Grade 2 (n = 31) Grade 3 (n = 13) Grade 4 (n = 17) |
Poly (66%) | Maximum of 36 months |
12 months cumulative incidence of treatment failure: 38% 12 months cumulative incidences of treatment failure due to uncontrolled seizures: 18% 12 months cumulative incidences of treatment failure due to adverse events: 17% |
| Levetiracetam | ||||||
| De Groot et al. (2011) [49] | 40 (n = 34 evaluable) | Pros |
Glioma Grade 2 (n = 7) Grade 3 (n = 12) Grade 4 (n = 15) |
Mono | 6 months observation |
6-months seizure free: 59% 6-months seizure reduction ≥ 50%: 74% |
| Kerkhof et al. (2013)d [7] | 36 | Retro | Glioblastoma (n = 36) | Mono | 9 (median) | Seizure free at the end of follow-up (minimum of 6 months): 69.5% |
| Maschio et al. (2011) [50] | 29 | Pros |
Glioma Grade 2 (n = 6) Grade 3 (n = 10) Grade 4 (n = 9) Meningeoma (n = 2) Other (n = 2) |
Mono |
12-months seizure freedom for n = 15 patients who reached this endpoint: 93.3% 12-months ≥ 50% seizure reduction: 6.7% (responder rate 100%) |
|
| Rosati et al. (2010) [52] | 82 | Pros |
Glioma: Grade 1/2 (n = 13) Grade 3 (n = 15) Grade 4 (n = 54) |
Mono | 13.1 (mean) | Seizure free with monotherapy levetiracetam at last follow up: 89% |
| Rossetti et al. (2013) [53] | 25 | Pros |
Glioma Grade 3 or 4 (n = 17) No further details |
Mono (n = 9) Poly (n = 14) |
12 months observation |
Composite endpoint (discontinuation of the study drug, add-on of a further ASM, ≥ 2 seizures with impaired consciousness) during 1 year follow-up: 36% Discontinuation due to side effects: 24% |
| Van der Meer et al. (2020)c [55] | 429 | Retro |
Glioma, grade 2–4 Grade 2 (n = 108) Grade 3 (n = 44) Grade 4 (n = 277) |
Mono | 86.2 (median) |
Treatment failure for any reason within 36-months follow-up: 40% Treatment failure because of AE within 36-months follow-up: 16% Treatment failure because of uncontrolled seizures within 36-months follow-up: 19% |
| Wagner et al. (2003) [54] | 26 | Pros |
Glioma Grade 3 and 4 (n = 18) Grade 2 (n = 8) |
Poly (n = 25) Mono (n = 1) |
9.3 (median) |
Seizure free 38% 6-months ≥ 50% seizure reduction: 35% |
| Topiramat | ||||||
| Maschio et al. (2007) [84] | 47 (45 evaluable) | Pros |
Glioma Grade 4 (n = 8) Grade 3 (n = 20) “Low grade” (n = 13) Meningeoma (n = 4) Metastasis (n = 2) |
Mono (n = 33) Poly (n = 14) |
16.5 (mean) |
Seizure free: 55.6%, ≥ 50% seizure reduction: 20% Discontinued TPM for severe side effects: 6.4% |
| Valproic acid | ||||||
| Van der Meer et al. (2020)c [55] | 429 | Retro |
Glioma Grade 2 (n = 105) Grade 3 (n = 44) Grade 4 (n = 280) |
Mono | 86.2 (median) |
Treatment failure for any reason within 36-months follow-up: 56% Treatment failure because of AE within 36-months follow-up: 32% Treatment failure because of uncontrolled seizures within 36-months follow-up: 17% |
| Kerkhof et al. (2013)d [7] | 36 | Retro | Glioblastoma (n = 36) | Mono | 9 (median) | Seizure free at the end of follow-up (minimum of 6 months): 77.8% |
aNumber patients in the study treated with the respective ASM
bRetrospective study comparing n = 61 patients with lamotrigine and n = 78 with lacosamide
cRetrospective observational study with matched groups of n = 429 patients each with levetiracetam and valproic acid
dRetrospective study on 291 patients with glioblastoma treated with levetiracetam or valproic acid monotherapy or polytherapy of both, efficacy of AED therapy was calculated only for patients who had a minimum follow-up period of 6 months
AE adverse event, ASM antiseizure medication, BTRE brain tumor related epilepsy
The trials reported heterogenous endpoints, most trials had included a variety of different tumor types and investigated variable ASM combinations additional to the study drug, partly due to drug approval only as add-on treatment at the time of the study. Hence, in general, recommendations for ASM choice in BTRE are currently based on therapy recommendations for focal epilepsies. LEV or LTG are valuable treatment options in focal epilepsies [46]. Recently the single-blind SANAD II study (in which, however, existence of a brain tumor had been an exclusion criteria) demonstrated superiority of lamotrigine compared to levetiracetam in focal epilepsies. In particular, the rate of treatment failures due to adverse reactions had been higher with levetiracetam than with lamotrigine [47]. If these results are transferable for brain tumor patients is a currently unresolved question. It has to be taken into account that while LTG itself is not an enzyme inducing drug, its metabolism is influenced by medications that induce the cytochrome P450-3A4 system. The number of studies on lamotrigine in BTRE is very limited. In one retrospective study, the 12-months cumulative incidence of treatment failure had been 38% and the incidence of adverse events 17% with a second line lamotrigine monotherapy (which had been comparable to the alternative treatment with LCM in this study) [48]. Besides potential interaction with anti-tumor medication, disadvantages of LTG are its availability only as an oral formulation and the slow titration at initiation of the medication. Both aspects can be especially relevant in patients with brain tumors in case of reduced consciousness, dysphagia and/or need of immediate seizure control.
Several studies have demonstrated that a medication with LEV is efficacious in BTRE [7, 49–54]. In contrast to lamotrigine, LEV can be applied intravenously, fast titration is possible and virtually no pharmacokinetic interaction has been reported. In a retrospective observational study on two matched groups of 429 patients the cumulative incidence of treatment failure had been lower in patients treated with LEV monotherapy than with VPA monotherapy. While the rate of adverse events was similar in both groups, LEV was more efficacious in seizure control [55]. However, a medication with LEV can lead to relevant neuropsychiatric side effects, particularly in patients with frontal tumors [56].
Another therapeutic option for treatment of BTRE is LCM. An intravenous application is available, titration is fast, the rate of neuropsychiatric side effects is low and there are very few interactions with other drugs. It has shown efficacy in BTRE in several trials, mostly as add-on treatment [57–62]. Recently, a retrospective analysis on LCM as monotherapy in 132 primary brain tumor patients reported seizure freedom in 64.4% of patients at 3 months and 55% at 6 months [63]. It is of note that before initiation of LCM an atrioventricular block of second or higher degree has to be excluded via electrocardiogram. A retrospective study in glioma patients, in which LTG (n = 61 patients) and LCM (n = 78 patients) were compared reported similar efficacy and a similar incidence of treatment failure due to adverse events for both ASMs [48].
In addition to the typical side effects of the individual ASMs, potentially beneficial concomitant effects of the medication (e.g., anxiolysis, mood stabilization, sedation) should also be considered when selecting the appropriate ASM.
Beyond choosing an effective ASM with few or no interaction with other medication, relevant criteria for the choice of ASM in patients with BTRE are (1) potentially beneficial side effects, (2) dosage form (oral, intravenous) and (3) avoidance of impairing side effects.
Management of persistent seizures
In case of remanifestation of seizures in brain tumor patients after former seizure control, tumor progression has to be excluded. Particularly in high grade gliomas recurrent seizures can be a sign of progression [64]. In case of tumor progression in combination with (or diagnosed because of) remanifestation of seizures, the goal of tumor specific treatment can be both: the control of tumor growth and of seizure frequency.
There is no sufficient data in BTRE to determine if an alternative ASM monotherapy or a polytherapy should be preferred in patients who do not become seizure free with their first monotherapy, neither is one ASM superior to others if applied as a second medication [38].
Perampanel and brivaracetam are two more recently approved non enzyme inducing treatment options often used as add-on treatment in focal epilepsies and have shown potential in smaller series in BTRE. In a pilot study on 26 glioma, meningioma and brain metastasis patients (21 patients could be evaluated at 6 months) treated with perampanel as add-on treatment, eight of 21 patients (31%) were seizure free at 6 months and 20 of 21 patients (95%) had a ≥ 50% seizure reduction [45]. In another study on perampanel in BTRE, 21 of 36 patients were evaluable for response to perampanel at 12-months follow-up. Of 21 patients seven patients were seizure free (33%) and 12 more patients had a seizure reduction ≥ 50% (≥ 50% seizure free rate 90%, 19/21 patients) [65]. For Brivaracetam a reduction of the seizure frequency from 7 per month to 2 per month was reported in a retrospective analysis on 33 primary brain tumor patients [66].
If cenobamate, a recently approved drug for focal epilepsies with promising results in two randomized placebo-controlled trials, might be able to play a therapeutic role for BTRE will have to be determined in the future [67, 68]. In the approval studies patients with potentially progressive causes of epilepsy were not eligible for inclusion.
As a practical approach, combination therapy is preferable if the first ASM has reduced seizure frequency, but has failed to control epilepsy completely. If the first ASM did not have any effect on seizure frequency, a second monotherapy should be initiated. The general recommendation to prefer non-enzyme inducing drugs whenever possible also applies for the remanifestation of seizures or for refractory seizures. A combination of two ASMs with the same mechanism of action is often associated with increased side effects.
Treatment of refractory seizures and status epilepticus
About 60% of patients with brain tumors do not become seizure free with the first ASM and of those patients, only 40% eventually become seizure-free with a second line monotherapy or polytherapy [69].
For patients with refractory BTRE (who usually require an antiseizure polytherapy, often including > 2 drugs), weighing side effects of ASM against a lack of seizure control is very important, especially at an advanced disease stage, when the therapeutic goal shifts from tumor control to mere symptom control. A retrospective study that included 100 patients with BTRE reported significantly more side effects, cognitive deficits and a lower quality of life in patients with antiseizure polytherapy, while the number of seizures was not related to quality of life [14].
In adults, 7% of status epilepticus (SE) are due to brain tumors and SE in BTRE is associated with significant mortality [70]. In their systematic review, Arik et al. found no evidence for the superiority of a particular ASM in tumor-related SE. Further data regarding the specificities in duration, prognosis and efficacy of ASM in tumor-related SE is needed. At present, treatment recommendations for SE in BTRE are based on treatment recommendations for SE in all epilepsies [71].
Especially at the advanced tumor stage, quality of life impairment caused by medication must be critically examined and individually weighed against the impairment by recurrent seizures. In very few patients with refractory seizures or status epilepticus, palliative tumor/epilepsy surgery may be considered as a treatment option for seizure reduction after careful individual evaluation in centers with combined neurooncology and epilepsy surgery expertise.
Adjustment of therapy for dysphagia in BTRE patients
Dysphagia is a frequently observed symptom in brain tumor patients. While some patients have swallowing difficulties in an early disease stage, dysphagia is a symptom more often observed in an advanced tumor stage. It can be caused by the tumor itself, by recurrent seizures or SE. Therefore, the dosage forms available for the various preparations should be taken into account for the choice of ASM in individual treatment situations. Many ASMs are available as oral liquids, which often are easier to swallow. For some of the new anticonvulsants (e.g., LEV, LCM), clinical experience in off-label subcutaneous use has been reported and has shown practical applicability in the palliative setting [72]. LEV can be applied as a continuous infusion via a syringe driver or as intermittent boli diluted in 100 ml 0.9% sodium chloride every 12 h over 30 min [73]. Case reports for subcutaneous use of LCM [74] (as an undiluted solution over 10 min) and BRV [75] (as a continuous infusion via syringe driver) have been published before. The oral to subcutaneous conversion rate was 1:1 for LEV, LCM and BRV. Proactively changing the dosage form in patients with dysphagia before a decrease in serum levels of ASM occurs might avoid seizures and SE.
Withdrawal of ASM
There is limited data on a possible cessation or withdrawal of ASM in brain tumor patients with epilepsy. To evaluate the risk of seizure recurrence and to guide patients with the wish to taper the ASM, risk calculators can be a valuable option, however, these calculators were not specifically designed for epilepsy patients with brain tumors [76]. These tools are on the one hand helpful for physicians to determine the recurrence risk in individual patients and on the other hand the visualization of a concrete percentage of risk of seizure recurrence can sometimes help to convince patients, who are not candidates for ASM withdrawal, to continue the medication.
In a prospective study on 83 patients with low grade or anaplastic glioma (of which 71 could be analyzed), who had been seizure free ≥ 1 year since last antitumor treatment or ≥ 2 years since the last seizure, a seizure recurrence in 26% (12/46) of patients who withdrew ASM and 8% (2/25) of patients who continued ASM was reported [77].
ASM should not be withdrawn in patients with progressive tumor, should not be stopped in patients with highly malignant tumors and short life expectancy and in those with difficult to control seizures in the past. In view of these authors, withdrawal of ASM is problematic in patients with little or no side effects of AEDs, with good social and professional reintegration after brain tumor therapy but with a high burden of social disadvantages if seizures recur.
ASM withdrawal is not recommended in patients with high risk of seizure recurrence independent of the duration of seizure freedom, however, determining the risk of seizure recurrence is difficult as it is influenced by multiple factors (e.g., tumor grade, location, type of treatment). In patients with grade 2 or 3 gliomas with a molecular profile that predicts favorable prognosis, stable disease of the tumor and long-term seizure freedom, tapering the medication might be considered in the following circumstances: if patients suffer from severe side effects (not solvable by changing the medication) or if there is an explicit patient wish even after detailed information about the risk of seizure recurrence and the consequences for daily living (e.g., fitness to drive) [78].
Fitness to drive in brain tumor patients with epilepsy
The fitness to drive in brain tumor patients can not only be impaired by epilepsy but also by motor, sensory and coordination deficits, impaired vision, and neurocognitive deficits.
The regulations if and when patients with brain tumors, particularly in case of BTRE, are able to resume driving are complex and guidelines differ substantially between countries. In Germany, the Ministry for Transport and Digital Infrastructure (Bundesanstalt für Straßenwesen, BASt) publishes guidelines for the assessment of the ability to drive. These guidelines do currently (version of December 31, 2019) include no chapter that focuses explicitly on brain tumor patients. For patients who have undergone brain surgery, the German guidelines prohibit driving for three months after surgery [79]. For patients with epilepsy driving is prohibited for 12 months after the last seizure. For patients with BTRE both prohibitions apply (and both together determine the duration of the inability to drive). The prerequisite to allow driving again is a regular follow-up depending on the underlying tumor (e.g., three months in patients with glioblastomas, 6 months in patients with diffuse low-grade gliomas) [79]. In Switzerland a consensus paper has been published in 2021 requiring the following examinations every three months to acquire or to maintain fitness to drive for glioblastoma patients: cranial magnetic resonance imaging (MRI) according to Response Assessment in Neuro-Oncology (RANO) criteria, medical history and comprehensive neurological examination (optional plus electroencephalography), optional ophthalmological examination including examination of visual field, optional neuropsychological assessment (with “optional” meaning, if careful assessment of history and/or neurological examination gives hint to pathology in this respect) [80]. In patients with brain metastases a clinical neurological examination had shown very low sensitivity to predict fitness to drive in 41 patients, who subsequently underwent a standardized assessment (occupational therapy driving assessment). The authors assumed that this was due to the fact that neurological examination can only limitedly or not predict judgment, reaction speed and complex visual-motor functions [81].
In summary, to evaluate the fitness to drive again for brain tumor patients is a major challenge for clinicians demanding for a multidisciplinary approach, involving neurologists, radiologists, ophthalmologists and neuropsychologists. However, the prohibition or permission to drive is one of the crucial factors of participation in daily living and the evaluation can be worth the effort in appropriate candidates (i.e., stable brain tumor, long-term seizure freedom).
Conclusions
Many patients with brain tumors suffer from epilepsy and treatment of BTRE is challenging. The evolving knowledge about the pathophysiological aspects of BTRE might influence future therapeutic recommendations. Current recommendations for ASM are based mostly on therapeutic recommendation in focal epilepsies in general, even though many trials on ASM excluded patients with brain tumors [47, 82]. LEV, LTG and LCM are non-enzyme inducing ASMs frequently used in BTRE. Randomized trials with matched patients concerning tumor type and additional medication, with reliable endpoints and careful assessment of side effects and quality of life are needed to determine optimal management of BTRE. Seizure freedom and ≥ 50% seizure reduction rate are commonly used endpoints in epilepsy trials, however, patients with brain tumors often have cognitive impairment preventing them to reliably report on their seizure frequency. Thus, ASM retention might be a more reliable endpoint with regard to therapeutic efficacy and is easily and routinely documentable during neurooncological follow-up [83]. ASM withdrawal and fitness to drive are aspects that require thorough work up before clinical decision making. Combined neurooncological end epileptological expertise is required to make decisions in these clinical situations.
Individualization of treatment approaches is increasingly addressed in both fields, epilepsy and neuro-oncology. Thus, the ideal future of BTRE treatment might comprise individualized antiseizure medication for different tumor types and stages with an additional effect on brain tumor proliferation. If perampanel might be such a drug needs to be evaluated in future studies.
Acknowledgements
Not applicable.
Abbreviations
- ASM
Antiseizure medication
- AMPA
α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
- AMPAR
α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor
- BTRE
Brain tumor related epilepsy
- GBP
Gabapentine
- IDH
Isocitrate dehydrogenase
- ILAE
International league against epilepsy
- LCM
Lacosamide
- LEV
Levetiracetam
- LTG
Lamotrigine
- MRI
Magnet resonance imaging
- OS
Overall survival
- RANO
Response assessment in neurooncology
- SE
Status epilepticus
- TPM
Topiramate
- VPA
Vaproic acid
- ZNS
Zonisamide
Author contributions
The concept of the project was created by SS, US and WG. SS performed the literature research. Writing of the original draft was done by SS and WG. The figures were created by SS, TW and DM. Review and editing of the manuscript was done by TW, DM, JW and US. JW and US supervised the project. All authors read and approved the final manuscript.
Funding
This research received no external funding.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
As this was a review article no ethics approval was applied for and as no patient data was analyzed for this review article consent to participate was not necessary.
Consent for publication
The manuscript does not contain any individual person’s data.
Competing interests
T.W. has received of honoraria or consultation fees Eisai, UCB, GW, Angelini, Precisis and is a stock shareholder of Amgen. J.W. has received speaker fees from UCB, Eisai, Bial, GW pharmaceuticals, and Desitin. U.S. received speaker’s honoraria from Medac, GSK and Novartis. W.G. has received speaker´s honoraria, travel or accommodation payment fees from UCB, Eisei, Bial and Desitin. The other authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, Bray F. Cancer statistics for the year 2020: An overview. International Journal of Cancer. 2021;149(4):778–789. doi: 10.1002/ijc.33588. [DOI] [PubMed] [Google Scholar]
- 2.Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS. CBTRUS Statistical Report: Primary brain and other central nervous system tumors diagnosed in the United States in 2013–2017. Neuro-Oncology. 2020;22(12 Suppl 2):iv1–iv96. doi: 10.1093/neuonc/noaa200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.le Rhun E, Guckenberger M, Smits M, Dummer R, Bachelot T, Sahm F, Galldiks N, de Azambuja E, Berghoff AS, Metellus P, Peters S, Hong Y-K, Winkler F, Schadendorf D, van den Bent M, Seoane J, Stahel R, Minniti G, Wesseling P, Weller M, Preusser M. EANO-ESMO clinical practice guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Annals of Oncology. 2021;32(11):1332–1347. doi: 10.1016/j.annonc.2021.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Pallud J, Audureau E, Blonski M, Sanai N, Bauchet L, Fontaine D, Mandonnet E, Dezamis E, Psimaras D, Guyotat J, Peruzzi P, Page P, Gal B, Párraga E, Baron M-H, Vlaicu M, Guillevin R, Devaux B, Duffau H, Taillandier L, Capelle L, Huberfeld G. Epileptic seizures in diffuse low-grade gliomas in adults. Brain. 2014;137(2):449–462. doi: 10.1093/brain/awt345. [DOI] [PubMed] [Google Scholar]
- 5.Pallud J, McKhann GM. Diffuse low-grade glioma-related epilepsy. Neurosurgery Clinics of North America. 2019;30(1):43–54. doi: 10.1016/j.nec.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Liang S, Zhang J, Zhang S, Fu X. Epilepsy in adults with supratentorial glioblastoma: Incidence and influence factors and prophylaxis in 184 patients. PLoS ONE. 2016;11(7):e0158206. doi: 10.1371/journal.pone.0158206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerkhof M, Dielemans JCM, van Breemen MS, Zwinkels H, Walchenbach R, Taphoorn MJ, Vecht CJ. Effect of valproic acid on seizure control and on survival in patients with glioblastoma multiforme. Neuro-Oncology. 2013;15(7):961–967. doi: 10.1093/neuonc/not057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wirsching H-G, Morel C, Gmür C, Neidert MC, Baumann CR, Valavanis A, Rushing EJ, Krayenbühl N, Weller M. Predicting outcome of epilepsy after meningioma resection. Neuro-Oncology. 2016;18(7):1002–1010. doi: 10.1093/neuonc/nov303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lieu A-S, Howng S-L. Intracranial meningiomas and epilepsy: Incidence, prognosis and influencing factors. Epilepsy Research. 1999;38(1):45–52. doi: 10.1016/S0920-1211(99)00066-2. [DOI] [PubMed] [Google Scholar]
- 10.Chan V, Sahgal A, Egeto P, Schweizer T, Das S. Incidence of seizure in adult patients with intracranial metastatic disease. Journal of Neuro-Oncology. 2017;131(3):619–624. doi: 10.1007/s11060-016-2335-2. [DOI] [PubMed] [Google Scholar]
- 11.Lamba N, Catalano PJ, Cagney DN, Haas-Kogan DA, Bubrick EJ, Wen PY, Aizer AA. Seizures among patients with brain metastases. Neurology. 2021;96(8):e1237. doi: 10.1212/WNL.0000000000011459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang J, Yao L, Peng S, Fang Y, Tang R, Liu J. Correlation between glioma location and preoperative seizures: A systematic review and meta-analysis. Neurosurgical Review. 2019;42(3):603–618. doi: 10.1007/s10143-018-1014-5. [DOI] [PubMed] [Google Scholar]
- 13.Penfield W, Erickson TC, Tarlov I. Relation of intracranial tumors and symptomazic epilepsy. Archives of Neurology & Psychiatry. 1940;44(2):300–315. doi: 10.1001/archneurpsyc.1940.02280080060002. [DOI] [Google Scholar]
- 14.Maschio M, Sperati F, Dinapoli L, Vidiri A, Fabi A, Pace A, Pompili A, Carapella CM, Cantelmi T. Weight of epilepsy in brain tumor patients. Journal of Neuro-Oncology. 2014;118(2):385–393. doi: 10.1007/s11060-014-1449-7. [DOI] [PubMed] [Google Scholar]
- 15.Rosenow F, Lüders H. Presurgical evaluation of epilepsy. Brain. 2001;124(9):1683–1700. doi: 10.1093/brain/124.9.1683. [DOI] [PubMed] [Google Scholar]
- 16.Shamji MF, Fric-Shamji EC, Benoit BG. Brain tumors and epilepsy: Pathophysiology of peritumoral changes. Neurosurgical Review. 2009;32(3):275–285. doi: 10.1007/s10143-009-0191-7. [DOI] [PubMed] [Google Scholar]
- 17.Mostofa AGM, Punganuru SR, Madala HR, Al-Obaide M, Srivenugopal KS. The process and regulatory components of inflammation in brain oncogenesis. Biomolecules. 2017;7(2):34. doi: 10.3390/biom7020034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vezzani A, French J, Bartfai T, Baram TZ. The role of inflammation in epilepsy. Nature Reviews Neurology. 2011;7(1):31–40. doi: 10.1038/nrneurol.2010.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soltani Khaboushan A, Yazdanpanah N, Rezaei N. Neuroinflammation and proinflammatory cytokines in epileptogenesis. Molecular Neurobiology. 2022;59(3):1724–1743. doi: 10.1007/s12035-022-02725-6. [DOI] [PubMed] [Google Scholar]
- 20.Urban H, Willems LM, Ronellenfitsch MW, Rosenow F, Steinbach JP, Strzelczyk A. Increased occurrence of status epilepticus in patients with brain metastases and checkpoint inhibition. OncoImmunology. 2020;9(1):1851517. doi: 10.1080/2162402X.2020.1851517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pallud J, Capelle L, Huberfeld G. Tumoral epileptogenicity: How does it happen? Epilepsia. 2013;54(s9):30–34. doi: 10.1111/epi.12440. [DOI] [PubMed] [Google Scholar]
- 22.Cucchiara F, Pasqualetti F, Giorgi FS, Danesi R, Bocci G. Epileptogenesis and oncogenesis: An antineoplastic role for antiepileptic drugs in brain tumours? Pharmacological Research. 2020;156:104786. doi: 10.1016/j.phrs.2020.104786. [DOI] [PubMed] [Google Scholar]
- 23.Lange F, Hörnschemeyer J, Kirschstein T. Glutamatergic mechanisms in glioblastoma and tumor-associated epilepsy. Cells. 2021;10(5):1226. doi: 10.3390/cells10051226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Venkataramani V, Tanev DI, Strahle C, Studier-Fischer A, Fankhauser L, Kessler T, Körber C, Kardorff M, Ratliff M, Xie R, Horstmann H, Messer M, Paik SP, Knabbe J, Sahm F, Kurz FT, Acikgöz AA, Herrmannsdörfer F, Agarwal A, Bergles DE, Chalmers A, Miletic H, Turcan S, Mawrin C, Hänggi D, Liu H-K, Wick W, Winkler F, Kuner T. Glutamatergic synaptic input to glioma cells drives brain tumour progression. Nature. 2019;573(7775):532–538. doi: 10.1038/s41586-019-1564-x. [DOI] [PubMed] [Google Scholar]
- 25.Venkatesh HS, Morishita W, Geraghty AC, Silverbush D, Gillespie SM, Arzt M, Tam LT, Espenel C, Ponnuswami A, Ni L, Woo PJ, Taylor KR, Agarwal A, Regev A, Brang D, Vogel H, Hervey-Jumper S, Bergles DE, Suvà ML, Malenka RC, Monje M. Electrical and synaptic integration of glioma into neural circuits. Nature. 2019;573(7775):539–545. doi: 10.1038/s41586-019-1563-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeng Q, Michael IP, Zhang P, Saghafinia S, Knott G, Jiao W, McCabe BD, Galván JA, Robinson HPC, Zlobec I, Ciriello G, Hanahan D. Synaptic proximity enables NMDAR signalling to promote brain metastasis. Nature. 2019;573(7775):526–531. doi: 10.1038/s41586-019-1576-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Venkataramani V, Tanev DI, Kuner T, Wick W, Winkler F. Synaptic input to brain tumors: Clinical implications. Neuro-Oncology. 2021;23(1):23–33. doi: 10.1093/neuonc/noaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mastall M, Wolpert F, Gramatzki D, Imbach L, Becker D, Schmick A, Hertler C, Roth P, Weller M, Wirsching H-G. Survival of brain tumour patients with epilepsy. Brain. 2021;144(11):3322–3327. doi: 10.1093/brain/awab188. [DOI] [PubMed] [Google Scholar]
- 29.Langan YM, Lucas R, Jewell H, Toublanc N, Schaefer H, Sander JWAS, Patsalos PN. Talampanel, a new antiepileptic drug: Single- and multiple-dose pharmacokinetics and initial 1-week experience in patients with chronic intractable epilepsy. Epilepsia. 2003;44(1):46–53. doi: 10.1046/j.1528-1157.2003.128902.x. [DOI] [PubMed] [Google Scholar]
- 30.Huberfeld G, Vecht CJ. Seizures and gliomas—Towards a single therapeutic approach. Nature Reviews Neurology. 2016;12(4):204–216. doi: 10.1038/nrneurol.2016.26. [DOI] [PubMed] [Google Scholar]
- 31.Skardelly M, Brendle E, Noell S, Behling F, Wuttke TV, Schittenhelm J, Bisdas S, Meisner C, Rona S, Tatagiba MS, Tabatabai G. Predictors of preoperative and early postoperative seizures in patients with intra-axial primary and metastatic brain tumors: A retrospective observational single center study. Annals of Neurology. 2015;78(6):917–928. doi: 10.1002/ana.24522. [DOI] [PubMed] [Google Scholar]
- 32.Stockhammer F, Misch M, Helms H-J, Lengler U, Prall F, von Deimling A, Hartmann C. IDH1/2 mutations in WHO grade II astrocytomas associated with localization and seizure as the initial symptom. Seizure. 2012;21(3):194–197. doi: 10.1016/j.seizure.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 33.Gonen T, Grossman R, Sitt R, Nossek E, Yanaki R, Cagnano E, Korn A, Hayat D, Ram Z. Tumor location and IDH1 mutation may predict intraoperative seizures during awake craniotomy: Clinical article. Journal of Neurosurgery JNS. 2014;121(5):1133–1138. doi: 10.3171/2014.7.JNS132657. [DOI] [PubMed] [Google Scholar]
- 34.Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, Fantin VR, Jang HG, Jin S, Keenan MC, Marks KM, Prins RM, Ward PS, Yen KE, Liau LM, Rabinowitz JD, Cantley LC, Thompson CB, vander Heiden MG, Su SM. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462(7274):739–744. doi: 10.1038/nature08617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen H, Judkins J, Thomas C, Wu M, Khoury L, Benjamin CG, Pacione D, Golfinos JG, Kumthekar P, Ghamsari F, Chen L, Lein P, Chetkovich DM, Snuderl M, Horbinski C. Mutant IDH1 and seizures in patients with glioma. Neurology. 2017;88(19):1805–1813. doi: 10.1212/WNL.0000000000003911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shen S, Bai Y, Zhang B, Liu T, Yu X, Feng S. Correlation of preoperative seizures with a wide range of tumor molecular markers in gliomas: An analysis of 442 glioma patients from China. Epilepsy Research. 2020;166:106430. doi: 10.1016/j.eplepsyres.2020.106430. [DOI] [PubMed] [Google Scholar]
- 37.Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, Engel J, Jr, Forsgren L, French JA, Glynn M, Hesdorffer DC, Lee BI, Mathern GW, Moshé SL, Perucca E, Scheffer IE, Tomson T, Watanabe M, Wiebe S. ILAE Official Report: A practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–482. doi: 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 38.Maschio M, Aguglia U, Avanzini G, Banfi P, Buttinelli C, Capovilla G, Casazza MML, Colicchio G, Coppola A, Costa C, Dainese F, Daniele O, de Simone R, Eoli M, Gasparini S, Giallonardo AT, La Neve A, Maialetti A, Mecarelli O, Melis M, Michelucci R, Paladin F, Pauletto G, Piccioli M, Quadri S, Ranzato F, Rossi R, Salmaggi A, Terenzi R, Tisei P, Villani F, Vitali P, Vivalda LC, Zaccara G, Zarabla A, Beghi E. Management of epilepsy in brain tumors. Neurological Sciences. 2019;40(10):2217–2234. doi: 10.1007/s10072-019-04025-9. [DOI] [PubMed] [Google Scholar]
- 39.Krauze AV, Myrehaug SD, Chang MG, Holdford DJ, Smith S, Shih J, Tofilon PJ, Fine HA, Camphausen K. A phase 2 study of concurrent radiation therapy, temozolomide, and the histone deacetylase inhibitor valproic acid for patients with glioblastoma. International Journal of Radiation Oncology, Biology, Physics. 2015;92(5):986–992. doi: 10.1016/j.ijrobp.2015.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weller M, Gorlia T, Cairncross JG, van den Bent MJ, Mason W, Belanger K, Brandes AA, Bogdahn U, Macdonald DR, Forsyth P, Rossetti AO, Lacombe D, Mirimanoff R-O, Vecht CJ, Stupp R. Prolonged survival with valproic acid use in the EORTC/NCIC temozolomide trial for glioblastoma. Neurology. 2011;77(12):1156. doi: 10.1212/WNL.0b013e31822f02e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barker CA, Bishop AJ, Chang M, Beal K, Chan TA. Valproic acid use during radiation therapy for glioblastoma associated with improved survival. International Journal of Radiation Oncology, Biology, Physics. 2013;86(3):504–509. doi: 10.1016/j.ijrobp.2013.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim Y-H, Kim T, Joo J-D, Han JH, Kim YJ, Kim IA, Yun C-H, Kim C-Y. Survival benefit of levetiracetam in patients treated with concomitant chemoradiotherapy and adjuvant chemotherapy with temozolomide for glioblastoma multiforme. Cancer. 2015;121(17):2926–2932. doi: 10.1002/cncr.29439. [DOI] [PubMed] [Google Scholar]
- 43.Cardona AF, Rojas L, Wills B, Bernal L, Ruiz-Patiño A, Arrieta O, Hakim EJ, Hakim F, Mejía JA, Useche N, Bermúdez S, Carranza H, Vargas C, Otero J, Mayor LC, Ortíz LD, Franco S, Ortíz C, Gil-Gil M, Balaña C, Zatarain-Barrón ZL. Efficacy and safety of levetiracetam versus other antiepileptic drugs in hispanic patients with glioblastoma. Journal of Neuro-Oncology. 2018;136(2):363–371. doi: 10.1007/s11060-017-2660-0. [DOI] [PubMed] [Google Scholar]
- 44.Happold C, Gorlia T, Chinot O, Gilbert MR, Nabors LB, Wick W, Pugh SL, Hegi M, Cloughesy T, Roth P, Reardon DA, Perry JR, Mehta MP, Stupp R, Weller M. Does valproic acid or levetiracetam improve survival in glioblastoma? A pooled analysis of prospective clinical trials in newly diagnosed glioblastoma. Journal of Clinical Oncology. 2016;34(7):731–739. doi: 10.1200/JCO.2015.63.6563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maschio M, Zarabla A, Maialetti A, Giannarelli D, Koudriavtseva T, Villani V, Zannino S. Perampanel in brain tumor-related epilepsy: Observational pilot study. Brain and Behavior. 2020;10(6):e01612. doi: 10.1002/brb3.1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kanner AM, Ashman E, Gloss D, Harden C, Bourgeois B, Bautista JF, Abou-Khalil B, Burakgazi-Dalkilic E, Park EL, Stern J, Hirtz D, Nespeca M, Gidal B, Faught E, French J. Practice guideline update summary: Efficacy and tolerability of the new antiepileptic drugs I: Treatment of new-onset epilepsy. Epilepsy Currents. 2018;18(4):260–268. doi: 10.5698/1535-7597.18.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marson A, Burnside G, Appleton R, Smith D, Leach JP, Sills G, Tudur-Smith C, Plumpton C, Hughes DA, Williamson P, Baker GA, Balabanova S, Taylor C, Brown R, Hindley D, Howell S, Maguire M, Mohanraj R, Smith PE. The SANAD II study of the effectiveness and cost-effectiveness of levetiracetam, zonisamide, or lamotrigine for newly diagnosed focal epilepsy: An open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet (London, England) 2021;397(10282):1363–1374. doi: 10.1016/S0140-6736(21)00247-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Opijnen MP, van der Meer PB, Dirven L, Fiocco M, Kouwenhoven MCM, van den Bent MJ, Taphoorn MJB, Koekkoek JAF. The effectiveness of antiepileptic drug treatment in glioma patients: Lamotrigine versus lacosamide. Journal of Neuro-Oncology. 2021;154(1):73–81. doi: 10.1007/s11060-021-03800-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.de Groot M, Aronica E, Heimans JJ, Reijneveld JC. Synaptic vesicle protein 2A predicts response to levetiracetam in patients with glioma. Neurology. 2011;77(6):532. doi: 10.1212/WNL.0b013e318228c110. [DOI] [PubMed] [Google Scholar]
- 50.Maschio M, Dinapoli L, Sperati F, Pace A, Fabi A, Vidiri A, Muti P. Levetiracetam monotherapy in patients with brain tumor-related epilepsy: Seizure control, safety, and quality of life. Journal of Neuro-Oncology. 2011;104(1):205–214. doi: 10.1007/s11060-010-0460-x. [DOI] [PubMed] [Google Scholar]
- 51.Merrell RT, Anderson SK, Meyer FB, Lachance DH. Seizures in patients with glioma treated with phenytoin and levetiracetam: Clinical article. Journal of Neurosurgery JNS. 2010;113(6):1176–1181. doi: 10.3171/2010.5.JNS091367. [DOI] [PubMed] [Google Scholar]
- 52.Rosati A, Buttolo L, Stefini R, Todeschini A, Cenzato M, Padovani A. Efficacy and safety of levetiracetam in patients with glioma: A clinical prospective study. Archives of Neurology. 2010;67(3):343–346. doi: 10.1001/archneurol.2009.335. [DOI] [PubMed] [Google Scholar]
- 53.Rossetti AO, Jeckelmann S, Novy J, Roth P, Weller M, Stupp R. Levetiracetam and pregabalin for antiepileptic monotherapy in patients with primary brain tumors. A phase II randomized study. Neuro-Oncology. 2014;16(4):584–588. doi: 10.1093/neuonc/not170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wagner GL, Wilms EB, van Donselaar CA, Vecht ChJ. Levetiracetam: Preliminary experience in patients with primary brain tumours. Seizure. 2003;12(8):585–586. doi: 10.1016/S1059-1311(03)00096-7. [DOI] [PubMed] [Google Scholar]
- 55.van der Meer PB, Dirven L, Fiocco M, Vos MJ, Kouwenhoven MCM, van den Bent MJ, Taphoorn MJB, Koekkoek JAF. First-line antiepileptic drug treatment in glioma patients with epilepsy: Levetiracetam versus valproic acid. Epilepsia. 2021;62(5):1119–1129. doi: 10.1111/epi.16880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Belcastro V, Pisani LR, Bellocchi S, Casiraghi P, Gorgone G, Mula M, Pisani F. Brain tumor location influences the onset of acute psychiatric adverse events of levetiracetam therapy: An observational study. Journal of Neurology. 2017;264(5):921–927. doi: 10.1007/s00415-017-8463-6. [DOI] [PubMed] [Google Scholar]
- 57.Maschio M, Zarabla A, Maialetti A, Fabi A, Vidiri A, Villani V, Giannarelli D. Quality of life, mood and seizure control in patients with brain tumor related epilepsy treated with lacosamide as add-on therapy: A prospective explorative study with a historical control group. Epilepsy & Behavior. 2017;73:83–89. doi: 10.1016/j.yebeh.2017.05.031. [DOI] [PubMed] [Google Scholar]
- 58.Rudà R, Pellerino A, Franchino F, Bertolotti C, Bruno F, Mo F, Migliore E, Ciccone G, Soffietti R. Lacosamide in patients with gliomas and uncontrolled seizures: Results from an observational study. Journal of Neuro-Oncology. 2018;136(1):105–114. doi: 10.1007/s11060-017-2628-0. [DOI] [PubMed] [Google Scholar]
- 59.Rudà R, Houillier C, Maschio M, Reijneveld JC, Hellot S, de Backer M, Chan J, Joeres L, Leunikava I, Glas M, Grant R. Effectiveness and tolerability of lacosamide as add-on therapy in patients with brain tumor-related epilepsy: Results from a prospective, noninterventional study in European clinical practice (VIBES) Epilepsia. 2020;61(4):647–656. doi: 10.1111/epi.16486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Saria MG, Corle C, Hu J, Rudnick JD, Phuphanich S, Mrugala MM, Crew LK, Bota DA, Dan Fu B, Kim RY, Brown T, Feely H, Brechlin J, Brown BD, Drappatz J, Wen PY, Chen CC, Carter B, Lee JW, Kesari S. Retrospective analysis of the tolerability and activity of lacosamide in patients with brain tumors: Clinical article. Journal of Neurosurgery JNS. 2013;118(6):1183–1187. doi: 10.3171/2013.1.JNS12397. [DOI] [PubMed] [Google Scholar]
- 61.Sepúlveda-Sánchez JM, Conde-Moreno A, Barón M, Pardo J, Reynés G, Belenguer A. Efficacy and tolerability of lacosamide for secondary epileptic seizures in patients with brain tumor: A multicenter, observational retrospective study. Oncology Letters. 2017;13(6):4093–4100. doi: 10.3892/ol.2017.5988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Villanueva V, Saiz-Diaz R, Toledo M, Piera A, Mauri JA, Rodriguez-Uranga JJ, López-González FJ, Gómez-Ibáñez A, Garcés M, González de la Aleja J, Rodríguez-Osorio X, Palao-Duarte S, Castillo A, Bonet M, Ruiz-Giménez J, Palau J, Arcediano A, Toledo M, Gago A. NEOPLASM study: Real-life use of lacosamide in patients with brain tumor-related epilepsy. Epilepsy & Behavior. 2016;65:25–32. doi: 10.1016/j.yebeh.2016.09.033. [DOI] [PubMed] [Google Scholar]
- 63.Mo F, Meletti S, Belcastro V, Quadri S, Napolitano M, Bello L, Dainese F, Scarpelli M, Florindo I, Mascia A, Pauletto G, Bruno F, Pellerino A, Giovannini G, Polosa M, Sessa M, Conti Nibali M, Di Gennaro G, Gigli GL, Pisanello A, Cavallieri F, Rudà R. Lacosamide in monotherapy in BTRE (brain tumor-related epilepsy): Results from an Italian multicenter retrospective study. Journal of Neuro-Oncology. 2022;157(3):551–559. doi: 10.1007/s11060-022-03998-6. [DOI] [PubMed] [Google Scholar]
- 64.di Bonaventura C, Albini M, D’Elia A, Fattouch J, Fanella M, Morano A, Lucignani G, Manfredi M, Colonnese C, Salvati M, Vanacore N, Berardelli A, Giallonardo AT. Epileptic seizures heralding a relapse in high grade gliomas. Seizure. 2017;51:157–162. doi: 10.1016/j.seizure.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 65.Coppola A, Zarabla A, Maialetti A, Villani V, Koudriavtseva T, Russo E, Nozzolillo A, Sueri C, Belcastro V, Balestrini S, Ferlazzo E, Giannarelli D, Bilo L, Maschio M. Perampanel confirms to be effective and well-tolerated as an add-on treatment in patients with brain tumor-related epilepsy (PERADET Study) Frontiers in Neurology. 2020;11:592. doi: 10.3389/fneur.2020.00592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Maschio M, Maialetti A, Mocellini C, Domina E, Pauletto G, Costa C, Mascia A, Romoli M, Giannarelli D. Effect of brivaracetam on efficacy and tolerability in patients with brain tumor-related epilepsy: A retrospective multicenter study. Frontiers in Neurology. 2020;11:592. doi: 10.3389/fneur.2020.00813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Krauss GL, Klein P, Brandt C, Lee SK, Milanov I, Milovanovic M, Steinhoff BJ, Kamin M. Safety and efficacy of adjunctive cenobamate (YKP3089) in patients with uncontrolled focal seizures: A multicentre, double-blind, randomised, placebo-controlled, dose-response trial. The Lancet Neurology. 2020;19(1):38–48. doi: 10.1016/S1474-4422(19)30399-0. [DOI] [PubMed] [Google Scholar]
- 68.Chung SS, French JA, Kowalski J, Krauss GL, Lee SK, Maciejowski M, Rosenfeld WE, Sperling MR, Mizne S, Kamin M. Randomized phase 2 study of adjunctive cenobamate in patients with uncontrolled focal seizures. Neurology. 2020;94(22):e2311. doi: 10.1212/WNL.0000000000009530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vecht CJ, van Breemen M. Optimizing therapy of seizures in patients with brain tumors. Neurology. 2006;67(12 suppl 4):S10. doi: 10.1212/WNL.67.12_suppl_4.S10. [DOI] [PubMed] [Google Scholar]
- 70.Arik Y, Leijten FSS, Seute T, Robe PA, Snijders TJ. Prognosis and therapy of tumor-related versus non-tumor-related status epilepticus: A systematic review and meta-analysis. BMC Neurology. 2014;14(1):152. doi: 10.1186/1471-2377-14-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, Bare M, Bleck T, Dodson WE, Garrity L, Jagoda A, Lowenstein D, Pellock J, Riviello J, Sloan E, Treiman DM. Evidence-based guideline: Treatment of convulsive status epilepticus in children and adults: Report of the guideline committee of the American Epilepsy Society. Epilepsy Currents. 2016;16(1):48–61. doi: 10.5698/1535-7597-16.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grönheit W, Popkirov SG, Wehner T, Schlegel U, Wellmer J. Practical management of epileptic seizures and status epilepticus in adult palliative care patients. Frontiers in Neurology. 2018;9:595. doi: 10.3389/fneur.2018.00595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sutherland A, Meldon C, Harrison T, Miller M. Subcutaneous levetiracetam for the management of seizures at the end of life: An audit and updated literature review. Journal of Palliative Medicine. 2020;24(7):976–981. doi: 10.1089/jpm.2020.0414. [DOI] [PubMed] [Google Scholar]
- 74.Rémi C, Zwanzig V, Feddersen B. Subcutaneous use of lacosamide. Journal of Pain and Symptom Management. 2016;51(2):e2–e4. doi: 10.1016/j.jpainsymman.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 75.Bond KR, Rea E, Lawthom C. Seizures in palliative medicine: Brivaracetam. BMJ Supportive & Palliative Care. 2021 doi: 10.1136/bmjspcare-2021-003228. [DOI] [PubMed] [Google Scholar]
- 76.Lamberink HJ, Otte WM, Geerts AT, Pavlovic M, Ramos-Lizana J, Marson AG, Overweg J, Sauma L, Specchio LM, Tennison M, Cardoso TMO, Shinnar S, Schmidt D, Geleijns K, Braun KPJ. Individualised prediction model of seizure recurrence and long-term outcomes after withdrawal of antiepileptic drugs in seizure-free patients: A systematic review and individual participant data meta-analysis. The Lancet Neurology. 2017;16(7):523–531. doi: 10.1016/S1474-4422(17)30114-X. [DOI] [PubMed] [Google Scholar]
- 77.Kerkhof M, Koekkoek JAF, Vos MJ, van den Bent MJ, Taal W, Postma TJ, Bromberg JEC, Kouwenhoven MCM, Dirven L, Reijneveld JC, Taphoorn MJB. Withdrawal of antiepileptic drugs in patients with low grade and anaplastic glioma after long-term seizure freedom: A prospective observational study. Journal of Neuro-Oncology. 2019;142(3):463–470. doi: 10.1007/s11060-019-03117-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Koekkoek JAF, Dirven L, Taphoorn MJB. The withdrawal of antiepileptic drugs in patients with low-grade and anaplastic glioma. Expert Review of Neurotherapeutics. 2017;17(2):193–202. doi: 10.1080/14737175.2016.1219250. [DOI] [PubMed] [Google Scholar]
- 79.Retrieved March 25, 2022, from https://bast.opus.hbz-nrw.de/opus45-bast/frontdoor/deliver/index/docId/2330/file/M115-2019.pdf
- 80.Hofer S, Keller K, Imbach L, Roelcke U, Hutter G, Hundsberger T, Hertler C, le Rhun E, Vasella F, Cordier D, Neidert M, Hottinger A, Migliorini D, Pflugshaupt T, Eggenberger N, Baumert B, Läubli H, Gramatzki D, Reinert M, Pesce G, Schucht P, Frank I, Lehnick D, Weiss T, Wirsching H-G, Wolpert F, Roth P, Weller M. Fitness-to-drive for glioblastoma patients: Guidance from the Swiss Neuro-Oncology Society (SwissNOS) and the Swiss Society for Legal Medicine (SGRM) Swiss Medical Weekly. 2021;151:w20501. doi: 10.4414/smw.2021.20501. [DOI] [PubMed] [Google Scholar]
- 81.Valencia-Sanchez C, Gorelkin VC, Mrugala MM, Sharma A, Vora SA, Ashman JB, Daniels TB, Halyard MY, Rule WG, Zhang N, Butterfield RJ, Schild SE, Porter AB. Clinical evaluation of fitness to drive in patients with brain metastases. Neuro-Oncology Practice. 2019;6(6):484–489. doi: 10.1093/nop/npz027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Marson AG, Al-Kharusi AM, Alwaidh M, Appleton R, Baker GA, Chadwick DW, Cramp C, Cockerell OC, Cooper PN, Doughty J, Eaton B, Gamble C, Goulding PJ, Howell SJL, Hughes A, Jackson M, Jacoby A, Kellett M, Lawson GR, Leach JP, Nicolaides P, Roberts R, Shackley P, Shen J, Smith DF, Smith PEM, Smith CT, Vanoli A, Williamson PR. The SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: An unblinded randomised controlled trial. Lancet (London, England) 2007;369(9566):1000–1015. doi: 10.1016/S0140-6736(07)60460-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.van der Meer PB, Dirven L, Fiocco M, Taphoorn MJ, Koekkoek JA. Retention rates of antiepileptic drugs in glioma patients: The most appropriate outcome. CNS Oncology. 2020;9(2):CNS53–CNS53. doi: 10.2217/cns-2020-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maschio M, Dinapoli L, Zarabla A, Pompili A, Carapella CM, Pace A, Giannarelli D, Occhipinti E, Jandolo B. Outcome and tolerability of topiramate in brain tumor associated epilepsy. Journal of Neuro-Oncology. 2008;86(1):61–70. doi: 10.1007/s11060-007-9430-3. [DOI] [PubMed] [Google Scholar]
- 85.Wehner, T., Unnwongse, K., & Wellmer, J. How are patients selected for intracranial EEG recordings, figure 4. In N. Axmacher (Ed.), Intracranial EEG for Cognitive Neuroscientists. Springer Nature (in press).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.