Abstract
COVID-19 outbreak quickly spread to all corners of the globe. In Brazil, the outbreak was particularly frightening because it worsened existing health, political, economic, and social problems. The results already observed show the contagion ripple-spreading process across the country, causing the death of thousands of people each day and counting, added to a very serious wave of unemployment, scientific denial, and social precariousness. Based on this, this study reviews recent research that looked at the role of the government, the Brazilian health system, and the main economic and social impacts fostered by the pandemic. We perform a scoping review according to the PRISMA-ScR to structure the qualitative synthesis of the 67 associated documents. The results reinforce the negative effects of the country's mismanagement and its consequent impacts on the Brazilian economy and society. The battleground against COVID-19 has fueled political tensions, shaken the health system, and unleashed social despair tinged with thousands of deaths. Finally, in the present scoping review, we discuss concerns about the impacts of the COVID-19 outbreak in Brazil and what the world hopes the country has learned from the current crisis.
Keywords: public health, COVID-19, review, social impacts, health system
The COVID-19 outbreak caused by the coronavirus disease has been declared as a global public health emergency.1,2 COVID-19 pneumonia was first reported in Wuhan City, China, in December 2019 and from there spread around the world.3,4 In February, 2020, the World Health Organization (WHO) officially declared a global pandemic, and as of March 30, 2020, COVID-19 had already affected 203 countries.5 The transmission of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has had a detrimental effect on global health systems, whose patients mainly present clinical symptoms of dry cough, fever, fatigue, and dyspnea.6 Approximately 15% of patients contracted the severe form of the disease, resulting in millions of deaths globally.7
According to the WHO, 6,040,609 confirmed cases and 370,657 deaths were reported worldwide up to June 2020. More than two years later, precisely, on June 3, 2022, the number of confirmed cases had reached 528,816,317, with 6,294,969 confirmed deaths.8 The unprecedented outbreak is triggering public health interventions and causing a ripple effect on human life. The COVID-19 pandemic has worsened economic problems, recession, unemployment, and educational problems around the world9 and has been collapsing the health system of many countries, with Brazil as an example, considering the number of confirmed cases and deaths registered by the Brazilian Ministry of Health.10 In Brazil, COVID-19 cases have been persistently high until June 3, 2022, reaching 31,060,017 confirmed cases and 666,801 deaths reported to WHO,8 and these are probably substantial underestimates. Recent publications highlight the chaos by naming the country's experience of the pandemic the “valley of death”,11 “the march of folly”,12 “the crisis within the crisis”,13 and “Brazilian pandemic/monium”.14
The first case reported in Brazil was on February 25, 2020. The country quickly reached the highest number of coronavirus cases in Latin America and became the country with the highest rate of transmission in the world. Even more worryingly, Brazil is marked by economic and social inequalities fueled by political problems, which have made the fragile country the epicenter of the epidemic in Latin America.15 With the arrival of COVID-19 in the country, health, economic, social, and political problems increased on a large scale, collapsing the Brazilian public health system, which was already precarious.
In an attempt to understand the COVID-19 outbreak in Brazil, we summarize previous literature related to the current global pandemic in the Brazilian context. Therefore, we conducted the current scoping review to assess outbreak numbers and issues related to the government role, the Brazilian unified health system, and economic impacts. We also present some of the main social impacts amplified by the coronavirus disease in Brazil. Our results show that the COVID-19 outbreak deeply affects the country, worsening issues that were already serious. Brazilian health problems were worsened during the pandemic due to disbelief in science, lack of investment, and overcrowding of hospitals, causing the death of thousands of people. Political dilemmas put the country on a tightrope, leaving the population at the mercy of the virus, and the economic problems, which were fostered by the previous two issues, caused thousands of cases of unemployment and increased the number of people living in extreme poverty.
Brief Background
The current COVID-19 outbreak sparked a scientific race and a cascade of reactions from researchers and health care institutions around the world. Many global and local studies are being carried out to find solutions to the global health crisis. To understand the development of studies on the COVID-19 outbreak in Brazil, we started by identifying the main universities and research centers related to research on SARS-CoV-2. Up to the date of this research (August 14, 2021), the University of São Paulo had published 239 documents associated with the COVID-19 outbreak in Brazil, followed by the Oswaldo Cruz Foundation (Fiocruz) with 144 papers. Table 1 shows these and other universities responsible for the largest amount of research on COVID-19 in Brazil. It is important to mention that the search query limits the number of documents. Furthermore, this section presents an overview of the totality of studies in Brazil without focusing on the goals outlined by this research.
Table 1.
Most Productive Brazilian Universities.
| Institution | Documents |
|---|---|
| University of São Paulo (USP) | 239 |
| Oswaldo Cruz Foundation (Fiocruz) | 144 |
| Federal University of São Paulo (UNIFESP) | 90 |
| Federal University of Minas Gerais (UFMG) | 85 |
| State University of Campinas (UNICAMP) | 71 |
| Federal University of Rio de Janeiro (UFRJ) | 62 |
| University of Brasilia (UnB) | 45 |
| Federal University of Rio Grande do Sul (UFRGS) | 45 |
The journals with the greatest number of documents were Plos One with 50 articles and the International Journal of Environmental Research and Public Health with 34 papers. Public Environmental Occupational Health was the most important category with 270 studies, followed by Infectious Diseases (109) and Environmental Sciences (104).
Previous literature reviews explored the anti-vaccine movement and immunization challenges in Brazil,16 different tests for the diagnosis of COVID-19,17 and environmental detection of SARS-CoV-2.18 Neves and Guerrero (2020)19 proposed a model to predict the evolution of the virus in Brazil, and Cotta and colleagues (2020)20 evaluated the impact of public health measures during the COVID-19 pandemic. The impact of the virus on the eating habits and physical activity of health care professionals are also explored,21 as well as symptoms of depression,22 child health vulnerabilities,23,24 and SARS-CoV-2 mutations in Brazil.25
Although many studies have explored the COVID-19 outbreak in the Brazilian context, most work has focused on analyzing specific issues related to the spread of SARS-CoV-2, drugs, and symptoms. Some studies have discussed political choices,26 moral dilemmas of public management,27 the transformation in the labor market,28 food insecurity,29 and some political and social problems30 in the face of the COVID-19 outbreak in Brazil. However, no study has presented a literature review focusing on the role of government, on the Brazilian health system, and on social and economic impacts caused by the current pandemic. It is against this background that this study precisely assesses this literature gap, by highlighting the government role, health system problems, and social and economic issues related to the COVID-19 outbreak in Brazil.
Material and Method
To achieve our goal, we perform a scoping review according to the Extended Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement for Scoping Reviews (PRISMA-ScR).31,32 A scoping review is a systematic process that allows the synthesis and analysis of both qualitative and quantitative studies. The execution of a scoping review consists of five steps: (1) information sources and literature search, (2) eligibility criteria, (3) screening process, (4) data abstraction process, and (5) synthesis.32
The ISI Web of Science Core Collection database was searched for eligible publications, as it has a large number of research documents from high-impact journals.33–38 The documents were exported on August 14, 2021. Quality assessment attributes are shown in Table 2.
Table 2.
Quality Assessment Criteria.
| Attributes | Description |
|---|---|
| Query | (“severe acute respiratory syndrome coronavirus 2” OR “SARS-CoV-2” OR “SARS-CoV-19” OR “SARS-CoV-2019” OR “2019-nCoV” OR “sars2” OR “Covid-19*” OR “Covid19*” OR “Covid-2019*” OR “coronavirus” OR “coronavirus disease 2019” OR “coronavirus disease-19” OR “2019 novel coronavirus” OR “2019 novel coronavirus infection” OR “novel coronavirus” OR “Wuhan seafood market pneumonia virus” OR “Wuhan coronavirus” AND “Brazil”)9,39 |
| Refined by | Document types: article and review Timespan: 2019 to August 14, 2021 Language: English Indexes: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, ESCI |
| Inclusion criteria | (1) articles concerning government role, (2) the Brazilian Unified Health System, (3) economic impacts, and (4) social impacts |
| Exclusion criteria | (1) studies not associated with COVID-19 and (2) case reports, books, editorials, letters to the editor, commentaries, and technical notes |
The associated documents were identified, and articles deemed potentially eligible were retrieved for full-text review. The data abstraction form was structured, and all included papers were abstracted by two reviewers working independently. Discrepancies were resolved through discussion with a third reviewer who is an expert in research methodology. Studies not related to social and economic aspects, the government's role, and the health system were removed. Ethics approval was not necessary.
Results
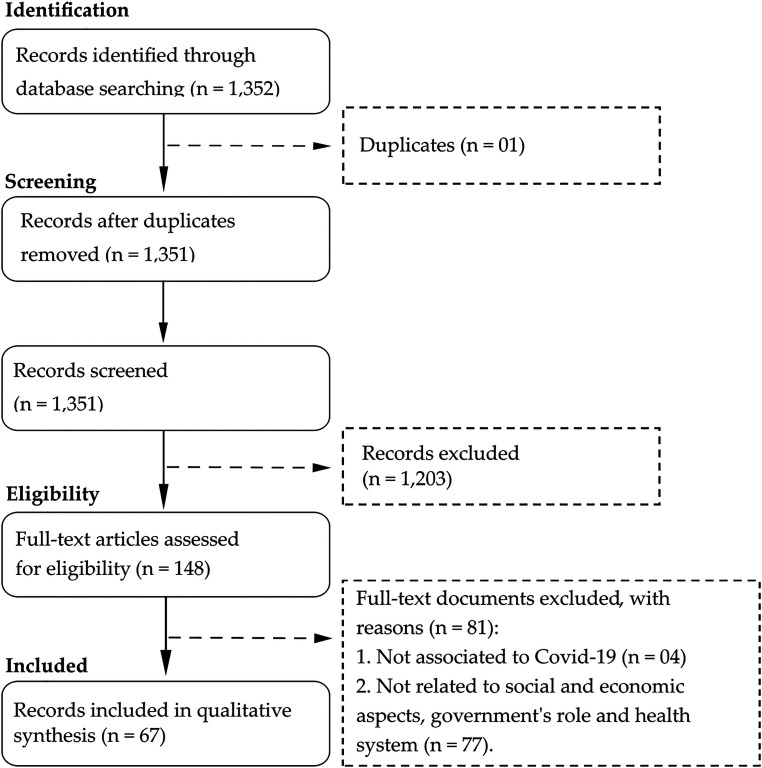
The original search identified 1352 documents from Web of Science. Among these articles, 1204 that were duplicates or not related were deleted. Finally, a total of 148 documents were fully read, and based on the previously mentioned eligibility criteria, 67 eligible studies were included in the qualitative analysis, as shown in Figure 1.
Figure 1.
PRISMA-ScR flow diagram.
Outbreak Numbers
Since the first case was reported in Brazil in February 2020, statistics predicted chaos in the Brazilian health system and economy. Even if the worst of the worst predictions were right, the world could not hide its concern about the number of confirmed cases and deaths.
Brazil is the fifth largest country in the world, the territorial extension direct influence on the spread of the disease. All 5570 municipalities across the country faced different challenges during the COVID-19 outbreak. The first case was confirmed in São Paulo, the most populous city in the Southern hemisphere, and spread from there to all 27 federal states of Brazil.40 Large cities such as Rio de Janeiro and São Paulo were the main hotspots, and the pandemic moved inland into smaller cities with inadequate or no medical equipment and supplies for intensive care.41 Small cities, with a lower number of hospital beds, were unable to attend to all patients, collapsing health and funeral systems.42 This was especially true because, historically, the Brazilian public health system operates with a shortage of—or outdated—equipment and medicines. The lack of resources forces the population to wait a long time to receive treatment.
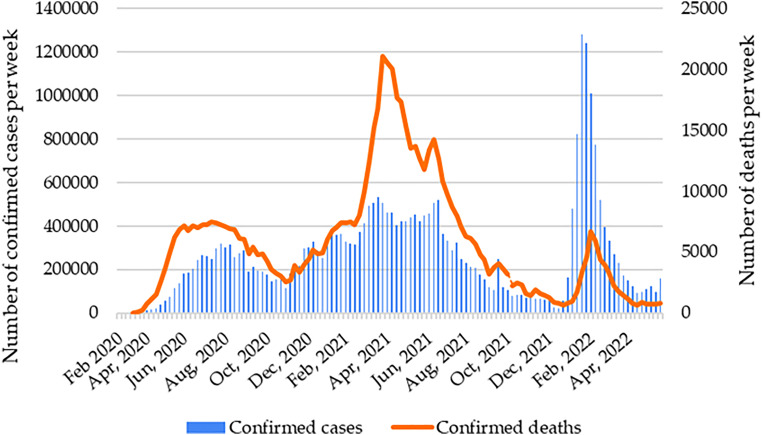
Although the virus spread rapidly across the country, large-scale tests were not applied to the population, and it is estimated that the number of people infected with SARS-CoV-2 was 15 times higher than official statistics.41Figure 2 shows the number of confirmed cases and the number of reported COVID-19-related deaths per epidemiological week of notification from the first confirmed case in February 2020.
Figure 2.
Number of confirmed cases and deaths.
On March 17, 2020, the first death from COVID-19 was reported.43 On May 23, 2020, Brazil ranked third worldwide in the number of cases and deaths from COVID-19. A few weeks later, the country ranked second worldwide in the number of infections and fatal victims of the virus.43 March and April 2021 were the most critical months, reaching 533,024 confirmed cases in the third week of March and 21,094 deaths in the fourth week of March.
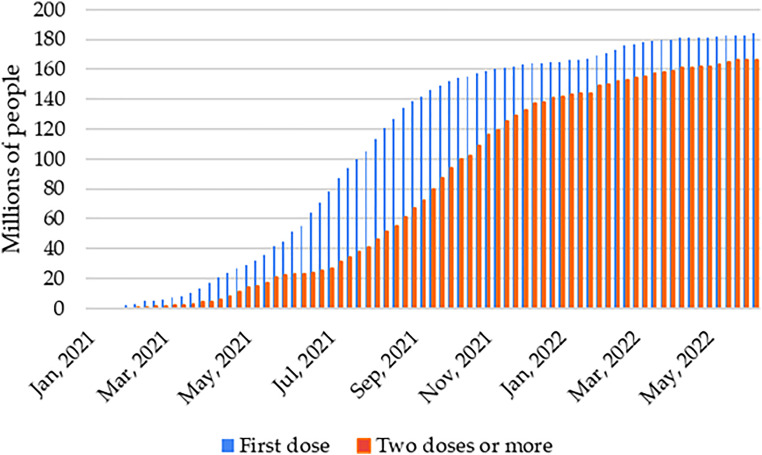
On January 17, 2021, Brazil started vaccinating the population. Vaccines began to be applied to priority groups, which include health professionals, institutionalized elderly people over 60 years of age, and the indigenous population living in villages.44 The initial expectation was that all 213 million Brazilians would receive two doses of the vaccine by the end of 2021. According to the Brazilian government, up until November 5, 2021, 161,945,574 (76.2%) Brazilians received the first dose of the vaccine, and 122,793,648 (57.8%) received two immunizing doses. In 2022, a third dose is being applied, and the fourth dose has started to be applied to elderly people and health care professionals. As of June 3, 2022, 184,018,923 (86.6%) of the population had received at least one dose, and 166,365,243 (78.3%) were fully vaccinated.45Figure 3 shows the number of vaccines applied.
Figure 3.
Number of vaccines applied.
Government Role
In Brazil, the economic and social problems aggravated by the COVID-19 outbreak cannot be understood separately from the country's political situation. On May 9, 2020, an editorial in The Lancet said: “COVID-19 in Brazil: “So what?”.” This criticism had two facets: On one hand, it was concerned with the social and health challenges in the emerging country. On the other hand, the concern was linked to political tensions that are carrying the country on a tightrope.46 “So what? I’m sorry. What do you want me to do about it?” were the words of the president of Brazil, Jair Bolsonaro, about the record of deaths from the COVID-19 outbreak.47 Thenceforth, the political stress collapsed the country, and the power struggle left more than 213 million Brazilians utterly confused. The Federal Government defended the economy while, conversely, the State Governors implemented restrictions that included social isolation and opening only essential services such as hospitals, pharmacies, and supermarkets.41 Public health policies, including isolation and lockdown, only began to be implemented when the Federal Government decided that State Governments had the autonomy to make decisions regarding the pandemic. Such disarray at the federal level is a deadly problem during a public health emergency.46
Going against WHO recommendations, Bolsonaro instigated economic activity, demonstrating “the contradictions of neoliberalism, which requires circulation even when it is proven to promote the illness and death of a significant percentage of the population”.48 The (un)wiseness used in country management directly impacts the results of a health crisis. In Brazil, the Federal Government had insufficiently mobilized to take mitigation initiatives,12 and COVID-19-related mortality and effects have placed the country in a critical situation that has economic and social effects on the entire society. The lack of quick responses to deal with the pandemic created an imbalance between the need to contain the virus and political interests,49 and the discourse of minimizing the severity of the disease and defending the use of drugs for early treatment without scientific evidence, such as hydroxychloroquine, evidence the political folly crisis.12,50
At the beginning of the pandemic, the Brazilian minister of health, Luiz Henrique Mandetta, adhered to the mitigation, social distancing, and quarantine measures proposed by the WHO. This decision caused conflicts with the president, and Mandetta was fired. The medical doctor Nelson Teich took over and was dismissed a month later for refusing to sign the authorization for the use of hydroxychloroquine. After that, army general Eduardo Pazuello held the position and authorized the prescription of hydroxychloroquine for mild cases of COVID-19 if the patient signed a consent form.50 Months later, the medical doctor Marcelo Queiroga assumed the position of Brazilian minister of health and continues to hold the position today.
It is important to keep in mind how the health of the Brazilian population was at the mercy of the president's political interests. Despite the country's historical social, health, economic and political problems, the games of power to the detriment of people's lives are evident. The population was left adrift, without leadership that would indicate a coherent path to face the pandemic. The president maintained the denial, saying that “there is no reason to panic” and “this is being propagated by the media”.13 To put the house in order, states and municipalities took on the responsibility for prevention, which fragmented policy when the country most needed a national pact to face the crisis.50
In order to meet the demands of the population and the pressure of the legislative opposition, the Brazilian Government and the Ministry of Economy approved law No. 13,982 in April 2020, granting emergency aid to the needy population.51 The aid—initially R$600 to R$1200 per month (around US$110-220) and later reduced to of R$150 to R$375—boosted the economy, but it is negligible if we consider the average cost of living in the country.50 In April 2021, the cheapest basic food basket in Brazil cost R$461.2852; in other words, the emergency assistance left little room for other monthly expenses, such as water, electricity, and rent bills, among others. In addition, the Federal Government did not present a national plan for the reorientation of the economy during the pandemic. An action plan could have stimulated all sectors to produce the necessary equipment and inputs, as well as create jobs at a time when economic activity was slowing down.13
As a consequence of ignoring science, the country had its public health, economic, and political problems aggravated.41 Pot-banging from balconies became a common form of protest against the country's government,46 and the expression “no oxygen, no vaccine, no government” was constantly appearing on the country's social media and walls. Bolsonaro's stance has been characterized as an antiscientific discourse that neglects everything that contradicts his ideology and political interests.53 These actions put at risk the lives of millions of people, as well as international cooperation partnerships and the nation's democracy.
The Unified Health System
The Unified Health System (abbreviation in Portuguese is Sistema Único de Saúde, or SUS) is one of the largest and most complex public health systems in the world. Through the system, throughout life, every Brazilian citizen has the right to full and free access to SUS. The actions of the public agency include urgent and emergency services; epidemiological, sanitary, and environmental surveillance; and pharmaceutical assistance.54 During the COVID-19 outbreak, the SUS has covered the health care of approximately 80% of the population, mainly people who cannot pay for private service.55 Despite its structure and large capacity, the Brazilian public health system can quickly collapse in the face of a pandemic.55 Historically, the SUS is neglected and receives insufficient public funds to cover all demands, and consequently, it cannot ensure the expected performance, causing delays in care or lack of equipment or medicines for the treatment of patients. Under these circumstances, the poor population is the most affected, as they depend exclusively on the SUS for any health care.
As the majority of the Brazilian population depends exclusively on SUS for any need related to treatment and health recovery, the pandemic and mass contamination collapsed many SUS services, especially hospitals, due to high demand. In this chaotic phase, when the country exceeded 1000 deaths a day, the Federal Government continued to defend early treatment.56 Several State Governors, through their own initiatives, sought ways to build and organize field hospitals, acquire equipment and supplies, and increase the number of intensive care units (ICU) beds available to the population.13 Despite the effort, many beds were only available for use after the reduction of cases, resulting in the expenditure of public money.50 In addition, the State's omission led society and private organizations to organize themselves in favor of the prevention of contamination. Companies reorganized production structures to provide protective equipment and alcohol gel, and communities organized the hiring of ambulances and health professionals.13
Many cities faced a lack of resources, supplies, and equipment for health care. In April 2021, the occupancy rate of ICU beds was over 90% in 21 states and the Federal District.57 The Manaus municipality, whose tragedy was presented by the national and international media, faced hospital overcrowding, and unattended people died in their own homes and were buried in mass graves due to overcrowding in cemeteries.13
To help identify suspected cases of COVID-19, the TeleSUS was developed, an integrated system that applies artificial intelligence to assist and guide people with suspected infection without requiring them to leave their homes.58 In a few days, TeleSUS served thousands of people, streamlining health care and dispatching requests for COVID-19 tests and medication.27 By directing part of the population with symptoms of COVID-19 to TeleSUS, it was possible to avoid the collapse of public health care in some Brazilian cities, guiding citizens with symptoms of the disease to remain in social isolation.59 The use of telemedicine during the pandemic characterized a great advance for Brazilian medicine, encouraging the use of information and communication technologies (ICTs) in the health context.60 Despite the apparent benefits, it is clear that there is still much to be done in terms of the population's access to ICTs. In addition, previous research has identified problems in TeleSUS apps; for a long time, the app recommended the use of masks only by people who were coughing or caring for infected people. Platforms also operated with missing or inconsistent information, which confused users.61 The actions of the Ministry of Health limited the population's access to concrete information about the pandemic, causing confusion, fear, and disbelief in the virus.
On the other hand, the centralization of resources for health in fighting the pandemic and the occupation of health professionals in caring for victims of COVID-19 left a gap in the care of people affected with other diseases, making them temporarily invisible to the health system.49 The situation was aggravated by the slow release of financial resources for the SUS, while the Federal Government prioritized economic issues: “This situation would be considered a scandal in any civilized country, because, during a pandemic, with cases and deaths growing exponentially for 16 weeks, the Ministry of Health keeps 67% of resources unused in the budget, without even being committed to something. It is not just about incompetence, it is a deliberate action not to spend, leaving the SUS and the Brazilian people to their own luck”,62 p. 295).
The challenges of the Brazilian health system and the number of deaths showed that the pandemic is much more than the “little flu,” the “cold,” or a “fantasy” promoted by the media, as President Bolsonaro said.63 Even with the challenges of each wave of COVID-19, the Brazilian health system and its professionals worked hard to serve the population and save lives. Despite the undeniable importance of the SUS for the country, a large part of the population fears the Federal Government's intention to privatize SUS services,64 which would leave most Brazilians without access to health care and treatment, due to the large regional disparity in access to services and the high costs of private services. However, discussions related to the privatization of the Brazilian public health service are not the result of the current pandemic.65,66 Over time, privatization occurs in different ways, and it is common to see private groups try to occupy the space of public services or private health services use subsidies from the public fund.67,68 Concerns about the privatization of health services motivated the creation of the National Front Against the Privatization of SUS, in 2018, formed by public health professionals, students, and SUS users. However, the lack of materials and professionals in the public service, added to the delay in care or poor care, discourages users from defending the SUS.68
Economic Impacts
The stoppage of several economic activities considered non-essential, the gradual resumption of these activities, and the investment in personal protective equipment negatively impacted the economies of several countries, causing the bankruptcy or closure of numerous businesses.69 When the pandemic escalated in Brazil in 2020, the country adopted measures of social isolation and closure of trade, causing significant impacts on supply and demand. These impacts contracted the economy due to three important reasons: reduced household consumption, reduced exports, and increased investment volatility. Added to the reduction in household consumption, the closing of commerce generated uncertainty in the population during the pandemic, causing a greater propensity to save money and, consequently, negatively affecting consumption of goods and services.70
As COVID-19 spread, the reduction of economic activities in many countries also decreased the volume and price of Brazilian exports. There was a reduction in investments due to the uncertainties generated by the government's denial and the absence of measures to mitigate the pandemic. The reduction in exports and the increase in the investment risk rate affected the Brazilian manufacturing industry, which is one of the most important sectors in the country because of its diverse production chains.51,71
In addition, the pandemic changed the production and consumption of goods and services, mainly due to the unemployment generated by the closure of establishments and the consequent loss of income and purchasing power of the workers.69 In 2020, the financial resources allocated by the Federal Government to deal with the COVID-19 outbreak reached R$604.75 billion, although R$81 billion remained uninvested.72 The government's primary deficit in 2020 was R$743.1 billion, compared to R$95 billion in 2019.73 The services sector, which represents 63% of the Brazilian Gross Domestic Product (GDP) and 68% of jobs, was one of the most affected, with an annual contraction of 7.8% in 2020.74 In trade, there was a reduction of 1.7 million jobs in 2020, out of 16 million people who worked in the sector before the pandemic. With the economic crisis, tax collection had a nominal drop of 4.1% in 2020.73 The shock between supply and demand and the reduction in income led to a strong contraction of the national GDP, which reached 4.3% in 2020, the worst result for the indicator since 1990 (−4.35).
The economic virus spread as fast as SARS-CoV-2, disrupting production chains around the world.75 The pandemic has brought frightening GDP projections and major concerns for small companies operating with limited capital and low financial reserves.76 This is especially worrying because three-quarters of Brazilian workers work in small formal or informal businesses, causing the economic recession and unemployment crisis to have profound impacts on Brazilian society.75
In this context, it is necessary to consider issues such as gender, social class, ethnicity, and sexuality, among others, which place some groups in a situation of greater vulnerability to pandemic impacts. The situation becomes more complex when thinking about groups that already faced disparities in the labor market, such as women. The implications for gender equality are substantial and are expected to persist beyond the duration of the pandemic.77 In Brazil, work resumed at a different pace than daycare centers and schools, leaving many women at the mercy of the need to care for their children, a role historically attributed to them.69
Another serious consequence of business closures and social isolation was the sharp drop in jobs. According to the National Survey of Continuous Household Samples,78 in 2020, the employment level of the Brazilian population dropped dramatically, reaching a total of 49.4% of the working-age population, as a result of economic and political crises fueled by the pandemic. The lowest level of employment was identified in the state of Alagoas, where only 35.9% of people able to work were employed, followed by Rio de Janeiro, where the index of employees reached 45.4%. In the first quarter of the pandemic, Brazil reached the largest contingent since 2002, with 14.805 million unemployed, a significant increase in the informality and precariousness of the workforce.78 Furthermore, informal workers also had difficulties to staying employed, as household consumption remained low. The level of informality decreased, not because of the achievement of formal employment, but because the crisis fueled by the pandemic first affected informal workers. The high unemployment rate caused a large reduction in the wage bill in the labor market, whose total value in the first quarter of 2020 was R$236 billion reais, falling to R$188 billion at the end of the second quarter of 2020.79
Considering gender differences, women were the most affected by unemployment (16.4%), against 11.9% of men. In terms of ethnicity, 17.2% of blacks were unemployed, 15.8% of browns, and 11.5% of white people. These data are directly linked to the level of education and the historical exclusion to which the black and brown population was subjected in the country, as this places them in a position of less education, and the highest rate of unemployment occurs precisely among people with incomplete secondary education (23.7%), whereas among people who have completed higher education the rate is 6.9 percent.78
As a measure to mitigate the impacts of the pandemic, the Proposal for Amendment to the Constitution (PEC 10/2020), also called the “War Budget,” was sanctioned. This is an extraordinary fiscal measure aimed at simplifying government spending to fight the coronavirus pandemic. Part of this budget was earmarked for emergency aid that began to be dispersed in April 2020 (600 reais per month) for low-income people. The aid was an important measure taken by the government, as it injected money into the economy and partly helped the resumption of household consumption. Then, the economy showed some signs of recovery in the third quarter of 2020. Although the current government of the country has an austere posture in relation to the pandemic, this measure generates protection for the most vulnerable populations.71 However, as a consequence of the reduction in emergency aid, the country's economic recovery was brief, and the injection of money was insufficient to repair the damage suffered by formal workers and the poorest layers of the population.80,81
Given this scenario, Brazil's historical social inequalities were deepened. According to the Cadastro Único (CadÚnico), in the first quarter of 2020, there were 13.5 million people in extreme poverty (with monthly income per person of up to R$89, or approximately US$16).52,81 A year later, in March 2021, this number rose 5.8%, adding 784,000 people in this condition. In 2019, the country already had alarming numbers; between 2019 and 2021, there was an increase of 9% of people in extreme poverty, which was aggravated by the effects of the pandemic.82
In the murky waters of the pandemic, the worsening of the outbreak, the risk of stagflation, mobility restrictions, and the slow pace of population immunization increase uncertainties regarding the recovery of the Brazilian economy.72 The chaos of the pandemic has only one certainty: The economic shock will have lasting and significant effects, and the country's recovery will require joint actions to reorganize the labor market and production chains.
Social Impacts
“How can a virus be “democratic” […] in such an unequal country?”.83 This is undoubtedly an important issue to bear in mind when analyzing the COVID-19 outbreak in Brazil, a country permeated by inequalities. In addition to economic inequalities, Brazil faces a series of inequalities related to social class, ethnicity/race, gender, and other structural problems.84 The pandemic shed light on the social disparities and inequalities that exist in Brazil and, in many contexts, aggravated them. Social distancing strategies have been and continue to be seriously affected in the country because low-income families and self-employed people need to work to ensure daily food. Moreover, the COVID-19 outbreak opened inequalities and prejudices much more in the peripheral Brazilian population, which suffers the most significant consequences14 —mainly, the 6% of the population living in slums (favelas), with little or no access to basic sanitation, waste management, potable water, and hygienic conditions.85
For people living in areas with greater vulnerability, hygiene and physical distance recommendations are almost impossible to follow, increasing the number of cases of infection and death. In addition, black and brown patients represent two-thirds of the COVID-19 cases in the North, Northeast, and Midwest regions of the country.86 This shows that historically marginalized and vulnerable people suffer the main damages of the pandemic: “In Brazil, the supposed democratic character of the virus is questioned when one observes the data that the black and peripheral population has higher lethality rates than the rest of the population. In Rio de Janeiro, at the beginning of May, the data reveal that the lethality rate in the Complexo de Favelas da Maré is 30.8%, while in the Leblon neighborhood it reaches 2.4%. Nevertheless, […] data […] indicate that the number of hospitalizations and deaths of black and brown people has a higher rate of increase than that of white people” (,87 p. 2).
In addition, indigenous peoples and women are particularly affected. The indigenous population suffers constant attacks in the country and has been ignored by the government that encourages illegal extraction from the Amazon rainforest. The war for territory leaves these people at a crossroads: They are exterminated in conflicts for their rights, or they are killed by the virus.88 Social isolation and access to hygiene items are privileges for few indigenous people in the country, and possibly, many died due to COVID-19 and were not statistically accounted for due to the impossibility of diagnosis or lack of medical support.89
Concerning women, social isolation has increased domestic violence and the number of femicides in the country.14 In addition, in the second quarter of 2020, the employment rate of women (39.7%) was significantly lower than that of men (58.1%), showing that the pandemic intensified the longstanding gender inequality in the Brazilian labor market.90
Nevertheless, the inequalities and the social and health precariousness in Brazil during the pandemic caused Brazilians to experience a unique tragedy.14 In addition to aggravating the country's economic and political challenges, the pandemic unleashed a wave of social despair, increasing the population's vulnerability, depression, and anxiety symptoms, especially in the most vulnerable subpopulations.91
Discussion
Historically, Brazil is affected by serious health issues as a result of neglecting emerging diseases, such as malaria, yellow fever, Chikungunya, Zika virus, and others that rapidly spread their symptoms and lethality across the country.11 The COVID-19 outbreak has dramatically worsened existing public health problems in Brazil. Unfortunately, thousands of people have lost their lives, others are suffering the consequences of a slow recovery, and millions have been left unemployed, food-insecure, or emotionally shaken.
As it spread to several countries, the COVID-19 pandemic was influenced by the particularities of each region according to their environmental, cultural, and economic conditions; available health services; and existing public policies (Jewett et al, 2021). These variables interfered with the spread of the disease, the prevention measures adopted, the guarantee of access to health services, and much more.13 In Brazil, it was no different: The economic, political, and health challenges placed the country at the top of the ranking of deaths and infections, along with the United States and India.
The COVID-19 outbreak has led to a global race that mobilized several countries and institutions across the world for the development of vaccines and treatments in record time. Brazilian initiatives for a vaccine were led by research groups with vast experience, such as the FioCruz Foundation and the Instituto Butantan.92 Despite this, the country has provided little financial support and incentives to exploit the potential of its scientific and internationalized community for solutions to the pandemic, ignoring its scientists and expertise.50 The SUS, the main system to fight the pandemic, has become the driving force for fighting the outbreak, as it includes a network of primary care, emergency services, hospitals, specialized services, and laboratories, together with a health, sanitary, and epidemiological surveillance system. In addition, the National Immunization Program was the basis for mass vaccination against COVID-19.
Despite the crucial role of the health system in guaranteeing universal and free access to thousands of Brazilians, it continues to operate in historically precarious conditions, with little investment and recognition by the government and by part of the population. The role of the government and the educational levels of the population can influence the way the Brazilian people dealt with the pandemic; after all “strangely, part of Brazilian society expresses itself eloquently to criticize the implementation of the lockdown, but it is extremely silent concerning lives reaped”.72
Despite the efforts of researchers and health professionals, the country remains influenced by political disputes, mainly between political authorities and the scientific community, as the State, which should make decisions in situations of catastrophes and emergencies based on the evidence provided by the national and global scientific communities, presented a denial of the severity of the pandemic. Thus, the country's politics and science walked in opposite directions, creating a scenario of insecurity and uncertainty for the population.13
Our findings are in line with the existing literature, showing that the COVID-19 outbreak negatively impacted the already fragile Brazilian economy and was stimulated by the political conflicts that drive the country. The sum of these factors further exacerbated some social inequalities and shook the Brazilian health system. Socioeconomic variables had a great influence on the spread of the disease93 and were aggravated by unemployment and overcrowding of the public health service.
In short, we can only imagine that if the country had invested in the health system and in research and education, in addition to heeding WHO guidelines, the pandemic would have taken a very different course. Faced with the global pandemic, whose proportions were even greater in Brazil, we can ask ourselves how the country will deal with another health crisis in the future, what lessons the population and its governments have learned after the giant challenges that have arisen or increased from the COVID-19 pandemic, and whether the lessons from this pandemic can be used to deal with future crises. We are hopeful that everyone has learned about solidarity and believes in science in these dark times.
Conclusion
In conclusion, the COVID-19 outbreak created chaos in Brazil, collapsing the health system, economy, and society. Every day, new studies pave the way for new medical solutions and vaccine approaches to SARS-CoV-2. The reality of the pandemic took a high toll on Brazilian society, on companies and their workers, on the health system, and on the health of millions of people. Hopefully, the COVID-19 pandemic in Brazil will be an example and, above all, prepare the country and the world to deal with similar situations in the future.
Our results show how the health of Brazilians was neglected during the COVID-19 outbreak and how the decisions of the country's managers affected the economy, especially the employment and livelihood of thousands of people. In addition, we highlight the impact of the pandemic on historically disadvantaged groups, such as indigenous people, black and brown people, and low-income people, especially those who live in Brazilian slums. The impact of the pandemic on minority groups needs to be studied in future research because government attitudes left these populations at the mercy of the virus through genocidal decisions. The low investment in research and in the public health service were also factors responsible for the worsening of the pandemic.
Finally, this work has limitations as it only contemplates documents from the Web of Science with discussions focused only on political, economic, social, and Brazilian health system issues. Although the literature published during the COVID-19 pandemic covered important topics, we hope that future research will focus on creating contingency plans to deal with future crises. Thus, future studies can explore in greater depth each of the topics presented in this scoping review and propose empirical approaches to deal with the pandemic. In addition, other topics—such as the impact of the COVID-19 outbreak on Brazilian education, the telemedicine, the world of work, the mental health of individuals, and each sector of the Brazilian economy—can be explored individually and more deeply in future research.
Author Biographies
Michele Kremer Sott holds a bachelor's degree in business and a master's degree in industrial systems and processes from the University of Santa Cruz do Sul, Brazil, and a master's degree in software engineering from the University of Quindío, Colombia. Sott is currently a PhD candidate and research fellow in business administration at Unisinos University. Her current research interests include the current COVID-19 outbreak, health care, and complex network analysis.
Mariluza Sott Bender holds a bachelor's degree in psychology and a master's degree in regional development from the University of Santa Cruz do Sul. She is a specialist in urgency, emergency, and intensive care and is currently pursuing a master's degree in psychology. Her current research interests include the current pandemic, mental health, gender, and sexuality.
Kamila da Silva Baum holds a bachelor's degree in economics from the Pontifical Catholic University of Rio Grande do Sul, Brazil. She has experience in spatial analysis and development economics. Her current research interests include poverty and regional economics.
Footnotes
CRediT Authorship Contribution Statement: Michele Kremer Sott: Conceptualization, Methodology, Validation, Formal analysis and investigation, Data curation, Writing—original draft preparation, Writing—review and editing, Visualization, Supervision. Mariluza Sott Bender: Conceptualization, Methodology, Validation, Formal analysis and investigation, Data curation, Writing—original draft preparation, Writing—review and editing, Visualization. Kamila da Silva Baum: Conceptualization, Methodology, Validation, Formal analysis and investigation, Data curation, Writing—original draft preparation, Writing—review and editing, Visualization.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is partially supported by the Coordination for the Improvement of Higher Education Personnel (CAPES), Brazil.
ORCID iD: Michele Kremer Sott https://orcid.org/0000-0002-7428-3993
References
- 1.Li P, Xie M, Zhang W. Clinical characteristics and intrauterine vertical transmission potential of coronavirus disease 2019 infection in 9 pregnant women: a retrospective review of medical records. Am J Obstet Gynecol. 2020;223(6):955-956. doi: 10.1016/j.ajog.2020.08.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khamisy-Farah R, Gilbey P, Furstenau LBet al. Big data for biomedical education with a focus on the COVID-19 era: an integrative review of the literature. Int. J. Environ. Res. Public Health. 2021;18(17):8989. doi: 10.3390/ijerph18178989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navarro V. The consequences of neoliberalism in the current pandemic. Int J Heal Serv. 2020;50(3):271-275. doi: 10.1177/0020731420925449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Ceukelaire W, Bodini C. We need strong public health care to contain the global Corona pandemic. Int J Heal Serv. 2020;50(3):276-277. doi: 10.1177/0020731420916725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu S, Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395(10233):1321-1322. doi: 10.1016/S0140-6736(20)30845-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Zhou Y. (2020). Prevalence of comorbidity and its effects in patients infected with SARS-CoV-2: a systematic review and metaanalysis. Int J Infect Dis, 94(1), 91‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57(1):279‐283. doi: 10.1016/j.jcrc.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coronavirus disease (COVID-19) outbreak. World Health Organization (WHO). https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Published June 10, 2021. Accessed June 13, 2022.
- 9.Furstenau LB, Rabaioli B, Sott MKet al. A bibliometric network analysis of coronavirus during the first eight months of COVID-19 in 2020. Int J Environ Res Public Health. 2021;18(3):1-24. doi: 10.3390/ijerph18030952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Artur APS, Abreu BMPN, Oliveira LdL, et al. Use of fuzzy logic to demonstrate possibility of health system collapse due to coronavirus pandemic / Uso Da Lógica Fuzzy Para Demonstrar a Possibilidade De Colapso Do Sistema De Saúde Devido À Pandemia De Coronavírus. Brazilian J Dev. 2021;7(1):1455-1466. doi: 10.34117/bjdv7n1-100 [DOI] [Google Scholar]
- 11.Homma A, Da Silva Freire M, Possas C. Vaccines for neglected and emerging diseases in Brazil by 2030: the “valley of death” and opportunities for RD&I in vaccinology 4.0. Cad Saude Publica. 2020;36(2):1‐18. doi: 10.1590/0102-311X00128819 [DOI] [PubMed] [Google Scholar]
- 12.Soares A,de Menezes RF. Coronavirus in Brazil: the march of folly. Saude e Soc. 2021;30(2):1‐17. doi: 10.1590/S0104-12902021200653 [DOI] [Google Scholar]
- 13.Henriques CMP, Vasconcelos W. Crises dentro da crise: Respostas, incertezas e desencontros no combate a pandemia da COVID-19 no Brasil. Estud Avancados. 2020;34(99):25-44. doi: 10.1590/S0103-4014.2020.3499.003 [DOI] [Google Scholar]
- 14.Cortese Coelho M. A Brazilian pandemia/monium: a researcher’s search for a ‘new normal’. Gender, Work Organ. 2021;28(S1):80-88. doi: 10.1111/gwao.12504 [DOI] [Google Scholar]
- 15.Gomes DS, Andrade LA, Ribeiro CJN, et al. Risk clusters of COVID-19 transmission in northeastern Brazil: prospective space-t-me modeling. Epidemiol Infect. Vol 148 (1), p. 08‐242020. doi: 10.1017/S0950268820001843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bivar GCC, De Aguiar MESC, Santos RVC, Cardoso PRG. COVID-19, the anti-vaccine movement and immunization challenges in Brazil: a review. Sci Med (Porto Alegre). 2021;31(1):1-8. doi: 10.15448/1980-6108.2021.1.39425 [DOI] [Google Scholar]
- 17.Laureano AFS, Riboldi M. The different tests for the diagnosis of COVID-19-a review in Brazil so far. J Bras Reprod Assist. 2020;24(3):340-346. doi: 10.5935/1518-0557.20200046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vicente VA, Lustosa BPR, Grisolia ME, et al. Environmental detection of sars-cov-2 virus rna in health facilities in Brazil and a systematic review on contamination sources. Int J Environ Res Public Health. 2021;18(7) 3824. doi: 10.3390/ijerph18073824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neves AG, Guerrero G. (2020). Predicting the evolution of the COVID-19 epidemic with the A-SIR model: Lombardy, Italy and Sao Paulo state, Brazil. Physica D: Nonlinear Phenomena, Volume 413, page 1-12, December 2020 Article number 132693. 10.1016/j.physd.2020.132693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cotta RM, Naveira-cotta CP, Magal P. Mathematical parameters of the COVID-19 epidemic in Brazil and evaluation of the impact of different public health measures. Biology (Basel). 2020;9(8):1-26. doi: 10.3390/biology9080220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mota IA, De Oliveira Sobrinho GD, Morais LPS, Dantas TF. Impact of COVID-19 on eating habits, physical activity and sleep in Brazilian healthcare professionals. Arq Neuropsiquiatr. 2021;79(5):429-436. doi: 10.1590/0004-282X-ANP-2020-0482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barros MdA, Lima MG, Malta DC, et al. Report on sadness/depression, nervousness/anxiety and sleep problems in the Brazilian adult population during the COVID-19 pandemic. Epidemiol e Serv Saude Rev do Sist Unico Saude do Bras. 2020;29(4):e2020427. doi: 10.1590/s1679-49742020000400018 [DOI] [PubMed] [Google Scholar]
- 23.Malta Campos M, Vieira LF. COVID-19 and early childhood in Brazil: impacts on children’s well-being, education and care. Eur Early Child Educ Res J. 2021;29(1):125-140. doi: 10.1080/1350293X.2021.1872671 [DOI] [Google Scholar]
- 24.Cabral IE, Pestana-Santos M, Ciuffo LL, Nunes YR, Lomba MLLF. Child health vulnerabilities during the COVID-19 pandemic in Brazil and Portugal. Rev. Latino-Am. Enfermagem. 2021;vol 29:e3422. doi: 10.1590/1518-8345.4805.3422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Timmers L, Peixoto J, Ducati R, Reports JB-S, 2021 U. SARS-CoV-2 mutations in Brazil: from genomics to putative clinical conditions. nature.com. Published online 2021.https://www.nature.com/articles/s41598-021-91585-6. Accessed August 22, 2021. [DOI] [PMC free article] [PubMed]
- 26.Domingues JM. Brazil In the face of COVID-19: tragedy and political choices. Environment. 2020;63(1):4-14. doi: 10.1080/00139157.2021.1842710 [DOI] [Google Scholar]
- 27.Santos LS. Moral dilemmas of the Brazilian public management in the face of the COVID-19 pandemic. Rev Adm Publica. 2020;54(4):909-922. doi: 10.1590/0034-761220200219x [DOI] [Google Scholar]
- 28.Costa SdS. The pandemic and the labor market in Brazil. Rev Adm Publica. 2020;54(4):969-978. doi: 10.1590/0034-761220200170x [DOI] [Google Scholar]
- 29.Manfrinato C V, Marino A, Condé VF, Franco MDCP, Stedefeldt E, Tomita LY. High prevalence of food insecurity, the adverse impact of COVID-19 in Brazilian favela. Public Health Nutr. 2021;24(6):1210-1215. doi: 10.1017/S1368980020005261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boschiero MN, Capasso Palamim CV, Ortega MM, Mauch RM, Lima Marson FA. One year of coronavirus disease 2019 (COVID-19) in Brazil: a political and social overview. Ann Glob Heal. 2021;vol 87, art. no. 44. doi: 10.5334/AOGH.3182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borges do Nascimento IJ, Cacic N, Abdulazeem HM, et al. Novel coronavirus infection (COVID-19) in humans: a scoping review and meta-analysis.J Clinical Med.2020; 9(4):941. https://www.mdpi.com/677406. Published online 2020. Accessed August 14, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tricco AC, Antony J, Zarin W, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1) art. no. 224, page 1-15. doi: 10.1186/s12916-015-0465-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dias JL, Sott MK, Ferrão CC, et al.. Data mining and knowledge discovery in databases for urban solid waste management: A scientific literature review. Waste Manage Res. 2021;39(11):1331-1340. doi: 10.1177/0734242X211042276. [DOI] [PubMed] [Google Scholar]
- 34.Furstenau L, Sott M, Homrich AJ, et al. An overview of 42 years of lean production: applying bibliometric analysis to investigate strategic themes and scientific evolution structure. Taylor Fr. 2021;33(9):1068-1087. doi: 10.1080/09537325.2020.1865530 [DOI] [Google Scholar]
- 35.Furstenau LB, Sott MK, Kipper LM, et al. Link between sustainability and industry 4.0: trends, challenges and new perspectives. IEEE Access. 2020;8:140079-140096, art. no. 9151934. doi: 10.1109/ACCESS.2020.3012812 [DOI]
- 36.Sott MK, Furstenau LB, Kipper LM, et al. Process modeling for smart factories: using science mapping to understand the strategic themes, main challenges and future trends. Bus Process Manag J. 2020;27(5):1391-1417. doi: 10.1108/BPMJ-05-2020-0181 [DOI] [Google Scholar]
- 37.Sott MK, Furstenau LB, Kipper LM, et al. Precision techniques and agriculture 4.0 technologies to promote sustainability in the coffee sector: state of the art, challenges and future trends . IEEE Access. 2020;8 (1):149854‐149867. doi: 10.1109/ACCESS.2020.3016325 [DOI] [Google Scholar]
- 38.Sott MK, Bender MS, Furstenau LB, Machado LM, Cobo MJ, Bragazzi NL. 100 Years of scientific evolution of work and organizational psychology: a bibliometric network analysis from 1919 to 2019. Front. Psychol. 2020;11:598676. 10.3389/fpsyg.2020.598676. Accessed November 6, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Herrera-Viedma E, López-Robles JR, Guallar J, Cobo MJ. Global trends in coronavirus research at the time of COVID-19: a general bibliometric approach and content analysis using SciMAT. Prof la Inf. 2020;29(3):1-20. doi: 10.3145/epi.2020.may.22 [DOI] [Google Scholar]
- 40.Candido DS, Watts A, Abade L, et al. Routes for COVID-19 importation in Brazil. J Travel Med. 2020;27(3), art. no taaa042, pages 1- 7. doi: 10.1093/jtm/taaa042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dantas E. Brazilian Report on the coronavirus crisis: a clash of pandemics. Med Law. 2020;39(2):153-160. 10.1590/0103-1104202012500I. Accessed August 21, 2021. [DOI] [Google Scholar]
- 42.Cavalcante JR, Cardoso-Dos-Santos AC, Bremm JM, et al. COVID-19 in Brazil: evolution of the epidemic up until epidemiological week 20 of 2020. Epidemiol e Serv Saude Rev do Sist Unico Saude do Bras. 2020;29(4):e2020376. doi: 10.5123/S1679-49742020000400010 [DOI] [PubMed] [Google Scholar]
- 43.Nascimento MLF. A multivariate analysis on spatiotemporal evolution of COVID-19 in Brazil. Infect Dis Model. 2020; vol 5: 670‐680. doi: 10.1016/j.idm.2020.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.COVID-19: Vacinação contra a covid-19 já teve início em quase todo o país. Ministério da Saúde distribuiu 6 milhões de doses do imunizante. SUS website. Available onhttps://www.unasus.gov.br/noticia/vacinacao-contra-a-covid-19-ja-teve-inicio-em-quase-todo-. Published March 2021, Acessed nov 14, 2021.
- 45.Terceira dose da vacina COVID-19, para reforço da imunização, começa em setembro. Federal government websiteAvailable onhttps://www.gov.br/casacivil/pt-br/assuntos/noticias/2021/agosto/ministerio-da-saude-anuncia-dose-de-reforco-para-vacinacao-contra-a-c. Published 2021.
- 46.The Lancet. COVID-19 in Brazil: “so what?”. The Lancet. 2020;395(10235):1461. doi: 10.1016/s0140-6736(20)31095-3. COVID-19 in Brazil:“So what?” ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7251993/. Accessed August 14, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Conde M. Brazil In the time of coronavirus. Geopolitica(s). 2020; vol 11 (especial): pages 239- 249. doi: 10.5209/GEOP.69349 [DOI] [Google Scholar]
- 48.Nunes J. (2020). A pandemia de COVID-19: securitização, crise neoliberal e a vulnerabilização global. Cadernos de Saúde Pública, 36(4), e00063120. doi: 10.1590/0102-311X00063120 [DOI] [PubMed] [Google Scholar]
- 49.Mendes EV. O Lado Oculto De Uma Pandemia: a Terceira Onda Da COVID-19. COLEÇÃO COVID-19 - Profissionais Saúde e Cuid Primários | Vol 4. Published online 2021:329-346.https://www.conass.org.br/biblioteca/volume-4-profissionais-de-saude-e-cuidados-primarios/. Accessed August 24, 2021.
- 50.Bueno F, Souto E, Matta G C, Notas sobre a Trajetória da Covid-19 no Brasil. In Book: Os impactos sociais da COVID-19 no Brasil: populações vulnerabilizadas e respostas à pandemia. Organizer: Matta GC, Rego S, Souto E, Segata J. Publisher: FioCruz, 2021, Vol 1, Pages: 27‐40, eISBN:9786557080320, doi: 10.7476/9786557080320 [DOI] [Google Scholar]
- 51.Brasil. Lei no 13.982, de 2 de abril de 2020. Altera a Lei no 8.742, de 7 de dezembro de 1993. Diário Oficial da União website, published 2020, Edição: 64-A, 1. Accessed August 24, 2021.
- 52.https://www.dieese.org.br/analisecestabasica/2021/202103cestabasica.pdf Pesquisa Nacional da Cesta Básica de Alimentos Março de 2021. Nota à imprensa, São Paulo: DIEESE, 2021.
- 53.Idrovo AJ, Manrique-Hernández EF, Fernández Niño JA. Report from Bolsonaro’s Brazil: the consequences of ignoring science. Int J Heal Serv. 2021;51(1):31-36. doi: 10.1177/0020731420968446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sistema Único de Saúde (SUS): estrutura, princípios e como funciona. 2021. Ministério da Saúde website. Available on: https://antigo.saude.gov.br/sistema-unico-de-saude. Accessed 24 August 2021.
- 55.Ribeiro F, Ribeiro F, Leist A. Who is going to pay the price of COVID-19? Reflections about an unequal Brazil. Int J Equity Health. 2020;19(1), art. no 91. doi: 10.1186/s12939-020-01207-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Melo K. Pazuello lamenta mortes por COVID- 19 e destaca tratamento precoce. Agência Brasil, Brasília, 8 ago. 2020. Available on: https://agenciabrasil.ebc.com.br/saude/noticia/2020-08/pazuello-lamenta-mortes-por-covid-19-e-destaca-tratamento-precoce Acce
- 57.Boletim Observatório COVID-19 após 6 meses de pandemia no Brasil. Edição especial, p.2. Fiocruz website. Available onhttps://portal.fiocruz.br/sites/portal.fiocruz.br/files/documentos/boletim_covid_6meses.pdfp. 13 Accessed 25 August 2021.
- 58.Marinho PRD, Cordeiro GM, Coelho HFC, Brandão SCS. COVID-19 in Brazil: a sad scenario. Cytokine Growth Factor Rev. 2021;58(1):51‐54. doi: 10.1016/j.cytogfr.2020.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mélo CB, Farias GD, Tavares Da Rocha T, Bezerra Barbosa De Moura R. Teleconsulta no SUS durante a pandemia da COVID-19 no Brasil. rsdjournal.org. doi:10.33448/rsd-v10i8.17675.
- 60.Alves de Veiga RS, Vinícius Rodrigues MP, Rodrigues dos Santos A, Carolina Silva Guimarães A, Cristina Santos Dutra S. Telemedicina e COVID-19: uma revisão de literatura. rbc.emnuvens.com.br. 2021;(1):3.https://rbc.emnuvens.com.br/cremego/article/view/53. Accessed July 4, 2022.
- 61.Motta I, Lopes J, Research MQ-SD, 2020 undefined. Interactive Voice Response systems for informing citizens about the COVID-19 pandemic: A study on Brazil’s Disque Saúde. revistas.unisinos.br. doi:10.4013/sdrj.2020.133.20
- 62.Costa AM, Rizzotto MLF, Lobato LdV. In the COVID-19 pandemic, Brazil sees the SUS. Saúde em Debate. 2020;44(125):289-296. doi:10.1590/0103-1104202012500i [Google Scholar]
- 63.da Luz Scherf E, Viana da Silva MV, Fachini JS. The management (or lack thereof) of COVID-19 in Brazil: implications for human rights and public health. Int J Hum Rights Healthc. 2020;14(2):158-174. doi: 10.1108/IJHRH-09-2020-0085 [DOI] [Google Scholar]
- 64.O que dizia a polêmica proposta sobre Unidades Básicas de Saúde, que acabou revogada por Bolsonaro. 2021. BBC News Brasil website. Available onhttps://www.bbc.com/portuguese/brasil-54727328. Accessed 05 Sept 2021.
- 65.Morosini MVGC, Fonseca AF, Baptista TW de Faria. Previne Brasil, the agency for the development of primary healthcare, and the services portfolio: radicalization of privatization policy in basic healthcare? Cad Saude Publica . 2020;36(8), pages 1‐20. doi: 10.1590/0102-311X00040220 [DOI] [PubMed]
- 66.Socal MP, Amon JJ, Biehl J. Right-to-medicines litigation and universal health coverage: institutional determinants of the judicialization of health in Brazil. Health Hum Rights. 2020;22(1):221-235. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7348422/. Accessed July 4, 2022. [PMC free article] [PubMed] [Google Scholar]
- 67.Straub M, Gomes R, Debate GA-S em, 2021 undefined. The public-private conflict in SUS: specialized outpatient care in Paraná. SciELO Bras. Accessed July 4, 2022. https://www.scielo.br/j/sdeb/a/gXWSySSV58WjvssRFwxbMMB/abstract/?lang=en
- 68.Cislaghi JF. Privatization of healthcarein Brazil: from big capital dictatorship to the PT dministrations. Rev Em Pauta. 2019;17(43), pages 60‐73. doi: 10.12957/rep.2019.42502 [DOI] [Google Scholar]
- 69.https://demografiaufrn.net/2020/06/29/impacto-mulheres/ O que já sabemos sobre os impactos socioeconômicos da pandemia da COVID-19 para as mulheres? ONAS - COVID19 – Observatório do Nordeste para Análise Sociodemográfica da COVID-19. ONAS website. Published 2020. Available on.
- 70.Nota Informativa: uma Análise da Crise gerada pela COVID-19 e a Reação de Política Econômica. MINISTÉRIO DA ECONOMIA website. Nota Técnica, published 13 de maio de 2020a. Available onhttps://www.gov.br/economia/pt-br/centrais-de-conteudo/publicacoes/. Accessed 06 Nov 2021.
- 71.Couto L. A Crise do COVID-19, regras orçamentárias e suas interpretações: mudanças necessárias? Published online 2020.http://repositorio.ipea.gov.br/handle/11058/9835. Accessed November 6, 2021.
- 72.https://jornal.unesp.br/2021/07/0 No Brasil, impacto econômico da pandemia será forte e duradouro Para re-tornar à normalidade, será preciso reorganizar a cadeia produtiva e o mercado de trabalho, especialmente para as mulheres. UNESP website, published on may 2021. Available on.
- 73.Impactos da pandemia sobre os resultados recentes das contas públicas. Ipea - Instituto de Pesquisa Economica Aplicada website. Published on oct 2021. Available onhttps://www.ipea.gov.br/cartadeconjuntura/index.php/2021/02/impac-tos-da-pandemia-sobre-os-resultados-recentes-das-c.
- 74.Marcas da pandemia. Valor magazine website. Published on 2021. Available onhttps://valor.globo.com/coronavirus/a-economia-na-pandemia/. Accessed 05 Sept 2021.
- 75.Nogueira MO, Silva SP, de Carvalho SS. From biological viruses to economic viruses: a vaccine for microenterprises in Brazil. Rev Adm Publica. 2020;54(4):1010-1021. doi: 10.1590/0034-761220200312x [DOI] [Google Scholar]
- 76.Alexander W. Bartik, Marianne Bertrand, Zoe Cullen, Edward L. Glaeser, Michael Luca, Christopher Stanton. The impact of COVID-19 on small business outcomes and expectations Proceedings of the National Academy of Sciences, 117 (30) (2020), pp. 17656‐17666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Alon T, Doepke M, Olmstead-Rumsey J, Tertilt M. The impact of COVID-19 on gender equality. Published online 2020.https://www.nber.org/papers/w26947. Accessed September 5, 2021.
- 78.Com pandemia, 20 estados têm taxa média de desemprego recorde em 2020. IBGE - Instituto Brasileiro de Geografia e Estatística, Agência IBGE Notícias website. Rio de Janeiro: IBGE, 2021. Available onhttps://agenciadenoticias.ibge.gov.br/agencia-notici.
- 79.Ministério da Economia avalia impacto econômico do coronavírus. MINISTÉRIO DA ECONOMIA website. Published online 2020.
- 80.Trovão C. A pandemia de COVID-19 e a desigualdade de renda no Brasil: um olhar macrorregional para a proteção social e os auxílios emergenciais. Ufrn Depec. 2020;4(1):1‐38. https://ccsa.ufrn.br/portal/wp-ontent/uploads/2020/05/TROVÃO-2020-PANDEMIA-E-DESIGUALDADE.pdf. Accessed November 6, 2021. [Google Scholar]
- 81.Secretaria Especial do Desenvolvimento Social. Ministério da Cidadania website. Published oin 2021. Available onhttp://mds.gov.br/acesso-a-informacao/perguntas-frequentes/bolsa-familia/beneficios/beneficiario. Published online 2021.
- 82.Insegurança alimentar e COVID 19 no Brasil. Rede Penssan website, [Brasília, DF], 2021. Available onhttp://olheparaafome.com.br/. Published online 2021.
- 83.Fernandes LAC, Silva CAF, Dameda C, Bicalho PPG. Covid-19 and the Brazilian reality: the role of favelas in combating the pandemic. Front. Sociol .2020;5:611990. doi: 10.3389/fsoc.2020.611990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Carnut L, Mendes Á, Guerra L. Coronavirus, capitalism in crisis and the perversity of public health in Bolsonaro’s Brazil. Int J Heal Serv. 2021;51(1):18-30. doi: 10.1177/0020731420965137 [DOI] [PubMed] [Google Scholar]
- 85.Almeida GB, Vilches TN, Ferreira CP, Fortaleza CMCB. Addressing the COVID-19 transmission in inner Brazil by a mathematical model. Sci Rep .2021;11(1): 1‐14. doi: 10.1038/s41598-021-90118-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ranzani OT, Bastos LSL, Gelli JGM, et al. Characterisation of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407-418. doi: 10.1016/S2213-2600(20)30560-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Costa Jd, Silva Jd, Brandão ESC, Bicalho PPG. COVID-19 No Sistema Prisional Brasileiro: Da Indiferença Como Política À Política De Morte. Psicol Soc. 2020;32(1):1‐19. doi: 10.1590/1807-0310/2020v32240218 [DOI] [Google Scholar]
- 88.Menton M., Milanez F., de Andrade Souza J. M., Cruz F. S. M. (2021). The COVID-19 pandemic intensified resource conflicts and indigenous resistance in Brazil. World Development, 138 (1), art no. 105222. [Google Scholar]
- 89.Palamim CVC, Ortega MM, Marson FAL. COVID-19 in the indigenous population of Brazil. J Racial Ethn Heal Disparities. 2020;7(6):1053-1058. doi: 10.1007/s40615-020-00885-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pandemia afetou mais o trabalho de mulheres, jovens e negros. Ipea – Instituto de Pesquisa Economica Aplicada website. Published on 2021. Available onhttps://www.ipea.gov.br/portal/index.php?option=com_content&view=article&id=37963&Itemid=9. Accessed 06 Sept 2021.
- 91.Zhang SX, Huang H, Li J, Antonelli-Ponti M, de Paiva SF, da Silva JA. Predictors of depression and anxiety symptoms in Brazil during COVID-19. Int J Environ Res Public Health. 2021;18(13):7026. doi: 10.3390/ijerph18137026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kanno AI, Barbosa MMF, Moraes L, Leite LCC. Sars-cov-2 vaccine development and how Brazil is contributing. Genet Mol Biol. 2021;44(1):20200320. doi: 10.1590/1678-4685-GMB-2020-0320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Martins LD, da Silva I, Batista WV, MdF Andrade, Ed Freitas, Martins JA. How socio-economic and atmospheric variables impact COVID-19 and influenza outbreaks in tropical and subtropical regions of Brazil. Environ Res. 2020;191 (1) art no. 110184. doi: 10.1016/j.envres.2020.110184 [DOI] [PMC free article] [PubMed] [Google Scholar]