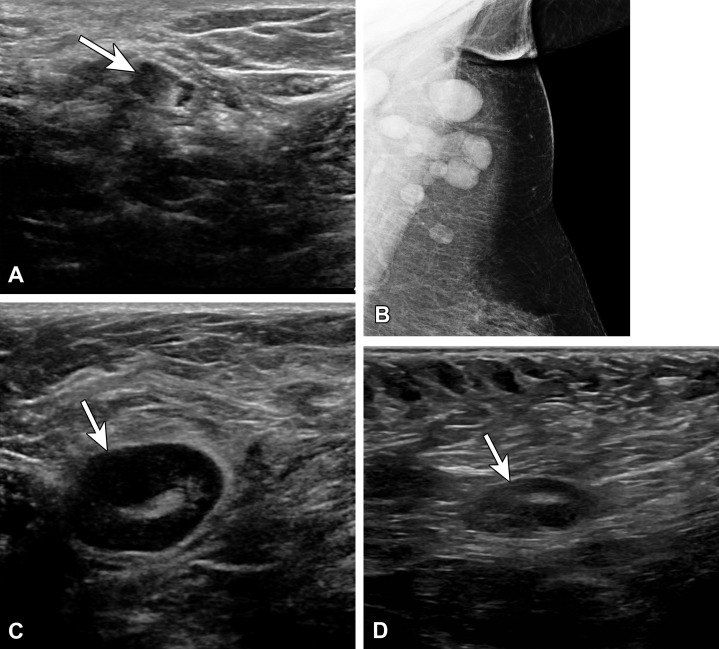
Figure 1.
(A) Vaccine-related lymphadenopathy in a 57-year-old man who presented for evaluation of the left axilla after surgical resection of melanoma along his back and positive axillary sentinel lymph node biopsy (SLNB). US image several weeks after an influenza vaccination shows a type 5 lymph node with asymmetric nodular cortical thickening (arrow). Results of core needle biopsy were benign, with no evidence of melanoma. (B–D) Vaccine-related lymphadenopathy in a 59-year-old woman who presented for evaluation of left axillary swelling after recently receiving a tetanus, diphtheria, and pertussis (Tdap) vaccination. Mammogram (B) shows multiple enlarged lymph nodes superiorly within the axilla. US images (C, D) show a type 5 lymph node with asymmetric nodular cortical thickening (arrow in C), which resolved at 3-month follow-up (arrow in D).