Figure 1. Main hallmarks of poststroke systemic inflammation over time.
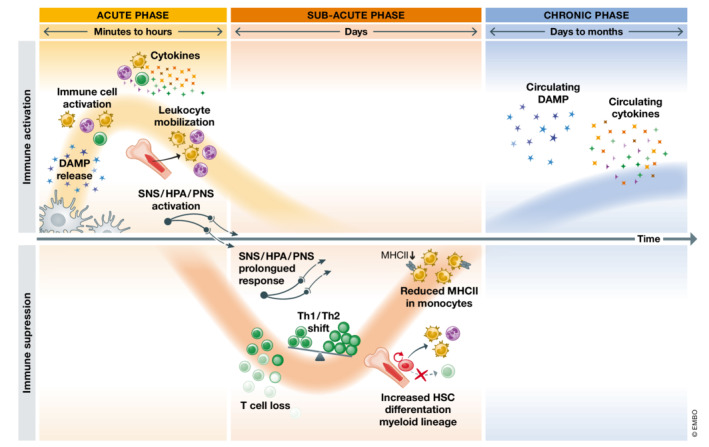
The peripheral immune response to stroke is initiated within minutes after stroke onset. DAMP are originated from dying or stressed cells within the ischemic brain or actively secreted by immune cells upon activation. Circulating DAMPs activate peripheral immune cells and provoke a massive expression and release of pro‐inflammatory cytokines into the bloodstream. Within the acute phase, stroke also induces the mobilization of more leukocytes from the spleen and the bone marrow as well as the activation of neurogenic pathways. In the subacute phase, within hours to days after stroke onset, a state of immunosuppression is triggered. The prolonged overactivation of neurogenic pathways as well as DAMP and other pro‐inflammatory mediators acutely released after stroke gradually induce lymphopenia due to massive cell death and the pronounced bias towards the monocyte differentiation pathway in bone marrow hematopoiesis. The is also a disbalance between Type 1 (Th1) and Type 2 (Th2) helper T cells and circulating monocytes are less capable of providing costimulatory signals. Later in time, a long‐term phase compromising peripheral immunity is characterized by chronic and sustained high levels of DAMP and pro‐inflammatory cytokines.
