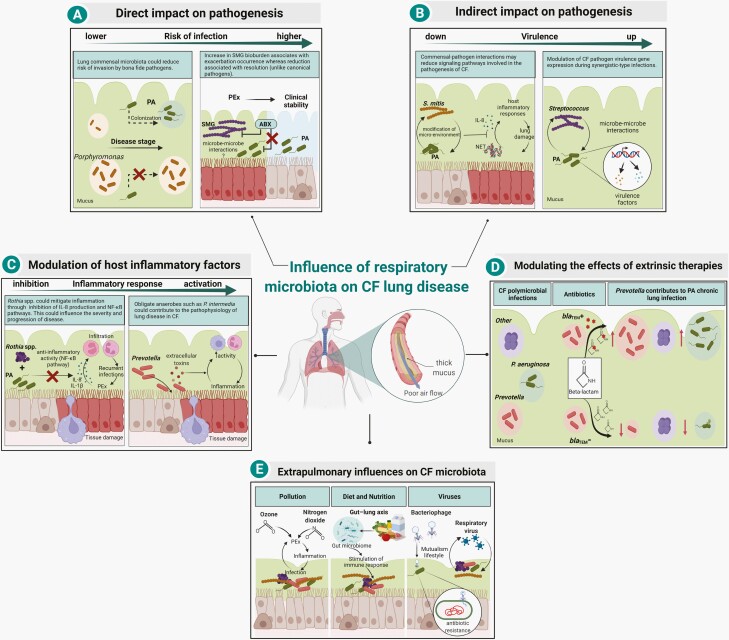
Figure 3.
Mechanisms by which respiratory microbiota influence CF lung disease. (A) Members of the CF microbiota have been associated with risk of infection in the airways. Colonization of commensal microbiota, such as Porphyromonas catoniae was found as a biomarker associated with a lower risk of P. aeruginosa (PA) early infection in CF [53]. In contrast, infection of Streptococcus milleri/anginosus group (SMG) at the onset of pulmonary exacerbations (PEx) is associated with symptomatic deterioration in clinical status, whereas its relative reduction is associated with symptom resolution (unlike canonical pathogens, such as P. aeruginosa) [3, 54]. (B) Commensal bacteria may negatively or positively influence the virulence of CF pathogens. Co-infection models in human epithelial cell lines with P. aeruginosa and commensal CF microbiota have shown that different strains of Streptococcus mitis reduce P. aeruginosa-induced inflammation through reduction of interleukin 8 (IL-8) production and neutrophil extracellular trap (NET) formation. The mechanism of action is still unknown but thought to be through modification of the micro-environment by metabolism adjustment by the commensal bacteria [55]. In contrast, some oral commensal streptococci enhance P. aeruginosa pathogenicity by increasing its virulence factor expression (eg, pyocyanin and elastase) [4, 56, 57]. (C) The CF microbiota contain bacteria with immunomodulatory activity that may alter host inflammatory response, which in turn could influence the progression of lung disease. Rothia mucilaginosa potentially mitigates host inflammation through the inhibition of the IL-8 production and NF-κB pathway activation in a human lung epithelial cell line [58]. Conversely, Prevotella intermedia was reported to be able to contribute to disease progression by secretion of cytotoxic extracellular toxins that induce the influx of macrophages and neutrophils in the airway lumen [59]. (D) CF microbiota influence disease through the modulation of extrinsic therapies. Extended-spectrum β-lactamases (ESBLs)-producing Prevotella isolates were reported to influence pathogenesis in vitro by shielding pathogens, such as P. aeruginosa from the action of β-lactam antibiotics [51]. (E) CF microbiota may be affected by a range of external factors, including pollution, diet, and viruses. Pollution may play a role in triggering PEx, leading to microbiota changes and further airway irritation and injury, which consequently could affect the extent of respiratory infections [60]. In the gut-lung axis, diet plays an important role in shaping the composition of the gut microbiota. Metabolites produced by the gut microbiota not only modulate gastrointestinal immunity but also impact immune responses in the lung [61, 62]. Bacteriophages may impact the fitness of members of the CF microbiota through horizontal gene transfer (HGT) of antimicrobial resistance genes [63]. Additionally, the progression of lung disease is influenced by infection with respiratory viruses which could indirectly promote community changes and host response [64]. Figure created with Biorender. Abbreviations: CF, cystic fibrosis; NF-κB, nuclear factor kappa B.