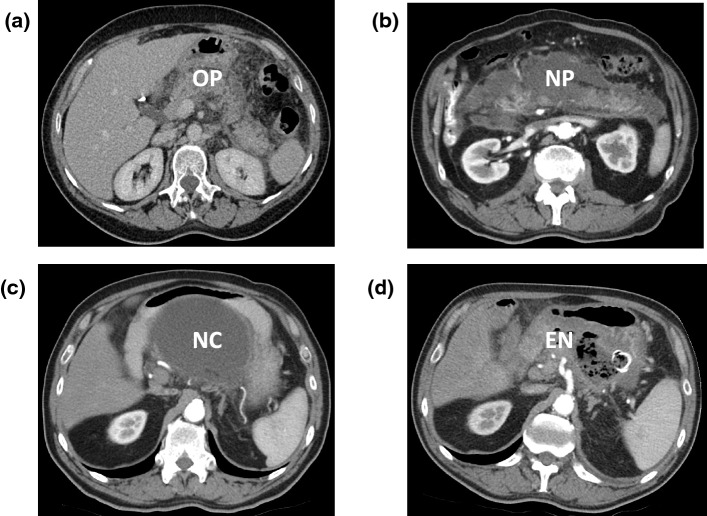
Fig. 5.
Contrast-enhanced computerised tomography scans of patients with acute pancreatitis, with application of specialist interventions for pancreatic necrosis. a Uncomplicated acute oedematous pancreatitis (OP) is seen with perfusion of the pancreatic parenchyma, surrounded by inflammation. b Acute necrotising pancreatitis (NP) with loss of most of the parenchyma, excepting a small portion in the head and separate small portion of the tail of the gland. This scan was taken 2 weeks into the attack and the necrosis with associated inflammation is diffuse and poorly localised. c More than 4 weeks after the onset of acute pancreatitis in the same patient as in b, the necrotic collection (NC) has become localised and walled off close to the posterior wall of the stomach, making it suitable for endoscopic drainage. (d) In the same patient as in b, infection has supervened, identified by the presence of radiolucent black gas bubbles within the collection, which was treated by endoscopic necrosectomy (EN). The endoscopically inserted self-expanding metal stent between the stomach and necrotic cavity is visible as a radiopaque white ring; flushing the cavity endoscopically every 7–10 days was necessary to empty and allow collapse of the cavity, following which the stent was removed