Abstract
Objectives
The objective of this study was to identify the determinants of exclusive breastfeeding (EBF) practice in Sheka zone, Ethiopia. In addition, the study aims to assess the prevalence of EBF practice in the study area.
Study design
A community-based cross-sectional study design was used.
Methods
A random sample of 630 mothers was selected by stratified cluster sampling using Kebele (an administrative unit) as a cluster. Data were collected using interviewer-administered questionnaires between June and July 2017. Descriptive statistics were used to assess the prevalence of EBF. A multivariable logistic regression model was used to identify determinants of EBF practice.
Results
The prevalence of EBF was 76%. The prevalence of EBF decreases as the age of the infant increases: 95.3% of infants aged 1 month were exclusively breastfed, but only 45.5% of infants aged 6 months were exclusively breastfed. The determinants of EBF practice were age of the child, mother’s educational level, marital status, household income, place of delivery, receiving postnatal care and place of residence. Mothers with a child aged <1 month were 34.9 times more likely to be practicing EBF than mothers with a child aged 5–6 months.
Conclusions
Although the prevalence of EBF was below the World Health Organisation recommended level, the practice of EBF in the study area was good. The prevalence of EBF was shown to decrease as infant age increased. Therefore, we recommend that health workers in health centres and hospitals provide advice about EBF and the duration of EBF during postnatal care visits and infant vaccination appointments.
Keywords: Exclusive breastfeeding, Under six months, Cross-sectional study
Highlights
-
•
Community-based cross-sectional study.
-
•
The prevalence of exclusive breastfeeding (EBF) in Sheka zone in 2017 was 76%.
-
•
The determinants of EBF included mother’s education, marital status, income, place of residence, age of child, PNC and place of delivery.
1. Introduction
Breastfeeding, and exclusive breastfeeding (EBF) in particular, is one of the major strategies that helps to improve the nutritional status and survival of infants worldwide. Malnutrition is responsible, directly or indirectly, for 60% of the 10.9 million annual deaths among children under 5 years of age. Feeding practices in infants and young children have a significant impact on their nutritional status. Approximately 40% of deaths in children under 2 years of age are associated with inappropriate feeding practices [1].
The World Health Organisation (WHO) and United Nations Children’s Fund (UNICEF) recommend that all mothers should breastfeed their children exclusively for the first 6 months and thereafter they should continue to breastfeed for as long as the mother and child wish. At the age of 6 months, in addition to breastfeeding, children should receive appropriate and sufficient complementary feeding [2,3].
Both UNICEF and the WHO emphasise that breastfeeding is critical to achieving many of the Sustainable Development Goals (SDGs), such as: SDG 2, ending hunger and improving nutrition; SDG 3, preventing child mortality and decreasing the risk of non-communicable diseases; and SDG 4, supporting cognitive development and education. Breastfeeding is also an enabler to ending poverty, promoting economic growth and reducing inequalities. Despite its demonstrated benefits, EBF prevalence and duration in many countries, including Ethiopia, are lower than the international recommendation of EBF for the first 6 months of life [3,4]. Previous studies in Ethiopia have shown that breastfeeding is nearly universal, but the proportion of children who are exclusively breastfed up to the age of 6 months is less than the recommended levels [5,6].
Breast milk helps prevent respiratory infections, diarrhoeal disease, urinary tract infections, obesity, asthma, diabetes and other life-threatening conditions in children. Furthermore, research suggests that breastfeeding protects mothers against breast and ovarian cancer, reduces bone density and possibly postpartum haemorrhage. Promoting EBF is particularly important in low-resource settings where maternal and infant mortality and morbidity rates are high [7].
In Ethiopia, national breastfeeding practices are poor for many reasons, including traditional and cultural beliefs, low educational levels, heavy workloads of mothers, poor sanitary conditions, type of assistance at delivery, duration of stay at home, ethnicity, poor maternal knowledge, age, parity, antenatal service utilisation and place of delivery [8,9].
According to the 2016 Ethiopian Demographic and Health Survey (EDHS), the proportion of infants aged <6 months old who received EBF was 58%, which was slightly improved compared to 2011 EDHS (52%), but remains far from the global recommendation of 90% [10].
Although many studies have been conducted in different parts of Ethiopia, the prevalence and determinants of EBF practice have not been determined in Sheka Zone; hence, the current investigation aims to fill this gap in the research.
2. Methods
2.1. Study area
This study was conducted in Sheka Zone, Ethiopia. The capital of the Zone, Masha, is located 676 km southwest of Addis Ababa, the capital of Ethiopia. Administratively, the Zone is structured into three Woreda (an administrative unit within the Zone), with two town administrations comprised of 10 urban and 57 rural Kebeles (an administrative unit within a Woreda).
2.2. Study design
A community-based cross-sectional study was carried out to investigate the determinants of EBF practice. The study population consisted of mothers who had an infant aged <6 months old and who were living in Sheka Zone at the time of data collection.
2.3. Sampling procedure and sample size determination
In our study, a stratified cluster sampling method was applied, using Kebeles as clusters, and urban and rural as stratums. The sample size was calculated using a single population proportion formula using the following parameters: confidence level (95%), margin of error (5.5%), the Ethiopian national prevalence of EBF (58%) and default value of design effect (2).
After adjusting the sample size for an anticipated non-response of 5%, the total sample size was 650. However, data were collected from only 630 (96.9%) mothers due to non-response. Reasons for non-response included respondents being away/visiting family at the time of data collection and refusal to participate (for unknown reasons).
2.4. Data collection
A structured interviewer-administered questionnaire was prepared by reviewing relevant literatures. Pre-testing of the questionnaire was completed by interviewing 20 respondents from Tepi town (one of the two town administrations) and the questionnaire was improved as a result of the pre-test. The questionnaire contained a combination of open-ended and closed-ended questions.
Interviews were administered by 15 community health extension workers. The interviewers completed an intensive 3-day training course, delivered by the investigators, on interviewing techniques, meanings of each question, and how to collect and record data. The data were collected between June and July 2017. The supervision of the survey during data collection was also conducted by the authors.
2.5. Variables
Dependent variable. The dependent variable for the study was the practice of EBF using the ‘ever given the infant anything besides breast milk since birth’ definitions.
Independent variables. The independent variables included maternal sociodemographic and socio-economic characteristics. Contextual factors were determined by the delivery history of the mother (i.e. place of delivery and type of birth). Infant characteristics included infant age in days, infant sex and infant morbidity (assessed on a 2-week recall).
2.6. Statistical analyses
Quantitative data were entered, coded and analysed using IBM SPSS version 20. Descriptive statistics were computed to determine the prevalence of EBF. To identify associated factors, a bivariate logistic regression was performed for each independent variable with EBF. Finally, multivariable logistic regression was completed to elucidate the determinants of EBF.
3. Results
As shown in Table 1, from the 630 respondents, 50% of mothers were living in rural areas, 54.9% were from the Sheka ethnic group and 94.9% were married. In addition, the largest proportion of mothers (40.8%) were aged <25 years and the mean age of the mothers was 27.3 years.
Table 1.
Demographic and socio-economic characteristics of participants.
| Variable | n | % |
|---|---|---|
| Place of Residence | ||
| Rural | 315 | 50.0 |
| Urban | 315 | 50.0 |
| Ethnicity | ||
| Sheka | 346 | 54.9 |
| Kefa | 101 | 16.0 |
| Amhara | 84 | 13.3 |
| Oromia | 34 | 5.4 |
| Others | 65 | 10.3 |
| Marital Status | ||
| Currently not married | 32 | 5.1 |
| Married | 598 | 94.9 |
| Mother’s education level | ||
| No education | 161 | 25.6 |
| Primary | 318 | 50.5 |
| Secondary | 113 | 17.9 |
| Tertiary | 38 | 6.0 |
| Mother’s occupation | ||
| Housewife | 394 | 62.5 |
| Employed | 57 | 9.0 |
| Merchant | 52 | 8.3 |
| Farmer | 71 | 11.3 |
| Others | 56 | 8.9 |
| Husband’s education level | ||
| No education | 116 | 18.9 |
| Primary | 270 | 44.0 |
| Secondary | 135 | 22.0 |
| Tertiary | 92 | 15.0 |
| Husband’s occupation | ||
| Not Employed | 345 | 56.4 |
| Employed | 154 | 25.2 |
| Merchant | 113 | 18.5 |
| Gender of the child | ||
| Male | 281 | 44.6 |
| Female | 349 | 55.4 |
| Age of the child (days) | ||
| ≤30 | 39 | 6.2 |
| 31–60 | 72 | 11.4 |
| 61–90 | 94 | 14.9 |
| 91–120 | 131 | 20.8 |
| 121–150 | 139 | 22.1 |
| 151+ | 155 | 24.6 |
| Monthly household income (ETB) | ||
| ≤1000 | 357 | 56.7 |
| 1001–2000 | 148 | 23.5 |
| 2001–3000 | 65 | 10.3 |
| >3001 | 60 | 9.5 |
ETB, Ethiopian Birr.
In total, 55.4% of the children were female. In terms of educational background, 50.5% of mothers attended primary level education and 44% of husbands of married women had primary level education. The majority of mothers (58.3%) were Protestant, followed by 32.7% Orthodox Christian. The average monthly family income was 1406.8 Ethiopian Birr (ETB), although 56.7% of households had a monthly income ≤1000 ETB.
3.1. Current practice of exclusive breastfeeding
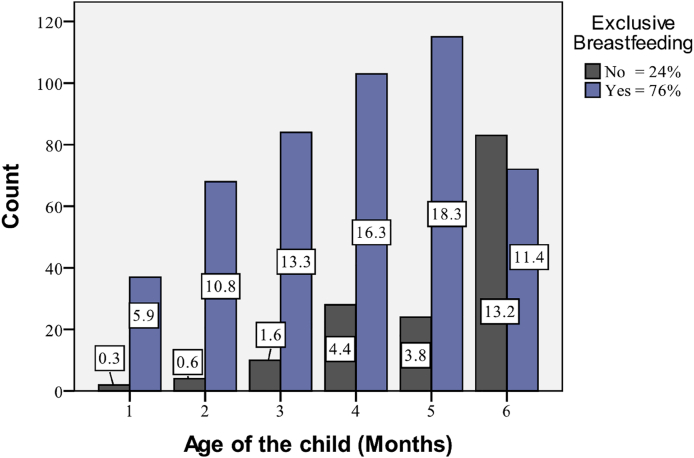
The current practice of EBF for children aged <6 months, as shown in Fig. 1, is 76% (479 mothers), with comparatively higher practice seen among mothers with a child aged <1 month old (92.3%).
Fig. 1.
Age of the child by exclusive breastfeeding status.
The detailed current practices of EBF are presented in Table 2. For mothers who were not practicing EBF, 84.1% gave clean water to their babies, 43.7% gave milk other than breast milk (e.g. fresh animal, powdered or tinned) and 5.3% gave porridge and/or gruel to their babies.
Table 2.
Mothers current exclusive breastfeeding (EBF) practice and knowledge.
| Variable | n | % |
|---|---|---|
| Knowledge of mothers on EBF duration | ||
| Yes | 605 | 96.0 |
| No | 25 | 4.0 |
| Knowledge of mothers on when the baby should start supplementary foods | ||
| Yes | 562 | 89.2 |
| No | 68 | 10.8 |
| How long the baby should be EBF (months [mean]) | 6.21 | |
| Foods in addition to breast milk | ||
| Ever had clean water | 127 | 84.1 |
| Ever had milk (powdered, tined or fresh animal) | 66 | 43.7 |
| Ever had porridge or gruel and others | 8 | 5.3 |
| Schedule of breastfeeding | ||
| Mother breastfed the baby when the baby wanted | 477 | 75.7 |
| Mother breastfed the baby when the baby cries | 402 | 63.8 |
| Mother breastfed the baby on schedule | 157 | 24.9 |
| Mother breastfed the baby when the mother wanted | 70 | 11.1 |
| Mother breastfed the baby whenever the breast engorged | 181 | 28.7 |
| Benefits of EBF for the baby | ||
| Breastfeeding is a good meal for the baby | 406 | 65.0 |
| Breastfeeding protects the baby from illnesses | 339 | 54.2 |
| Breastfeeding develops the relationship between mother and baby | 140 | 22.4 |
| Breastfeeding helps the growth of the baby | 402 | 64.3 |
| Benefits of EBF for the mother | ||
| After delivery breastfeeding helps the uterus to return to its position | 63 | 10.6 |
| Breastfeeding develops the relationship between mother and baby | 328 | 55.2 |
| Breastfeeding prevents pregnancy | 183 | 30.8 |
| Breastfeeding protects the mother from illnesses | 365 | 61.4 |
| Breastfeeding saves money | 158 | 26.6 |
| Knowledge of mother on when to give breast to the baby | ||
| The baby should be put to breast whenever the baby wants | 494 | 78.5 |
| The baby should be put to breast whenever the mother wants | 210 | 33.4 |
| The baby should be put to breast on schedule | 175 | 27.8 |
More than half of the mothers who participated in this study identified advantages of breastfeeding for the baby, including it providing a good meal for the baby (65.0%), protecting the baby from illnesses (54.2%), helping the growth of the baby (64.3%) and developing the relationship between mother and baby (22.4%). The recommended duration of EBF was correctly identified to be 6 months by 96% of the mothers who participated (mean = 6.21 months).
3.2. Reproductive health history
The reproductive health histories of the study participants are presented in Table 3. The average number of children born alive was 2.4. For 31.6% of participants, the infant referred to in this study was their first child. The majority of mothers (97.6%) had received antenatal care (ANC) for the most recent pregnancy. In total, 34.1% of mothers gave birth in government hospitals and 53.2% in government health centres; 87.6% of mothers were advised about EBF during delivery. Postnatal care (PNC) for the most recent birth was reported by 81.3% of mothers.
Table 3.
Reproductive health history of mothers.
| Variable | n | % |
|---|---|---|
| Received ANC | ||
| Yes | 615 | 97.6 |
| No | 15 | 2.4 |
| Get advice about breastfeeding at ANC | ||
| Yes | 362 | 58.9 |
| No | 253 | 41.1 |
| Place of delivery | ||
| Home or private health center | 80 | 12.7 |
| Government hospital | 215 | 34.1 |
| Government health center | 335 | 53.2 |
| Type of delivery | ||
| Normal | 587 | 93.2 |
| Caesarian | 43 | 6.8 |
| Get advice about breastfeeding on delivery | ||
| Yes | 552 | 87.6 |
| No | 78 | 12.4 |
| Received PNC | ||
| Yes | 512 | 81.3 |
| No | 118 | 18.7 |
| Get advice about breastfeeding on PNC | ||
| Yes | 501 | 98.0 |
| No | 10 | 2.0 |
| Birth order of child | ||
| First | 199 | 31.6 |
| Second | 171 | 27.1 |
| Third and above | 260 | 41.3 |
| Child morbidity for last 2 weeks | ||
| Yes | 125 | 19.8 |
| No | 505 | 80.2 |
| Birth interval between the last two children (years [mean]) | 2.64 | |
| Number of children born alive [mean] | 2.37 | |
ANC- antenatal care; PNC- postnatal care.
3.3. Factors associated with exclusive breastfeeding practice
Multiple logistic regression analysis was performed by considering variables that were significant up to the 20% significant level in the bivariate analysis. A forward stepwise method was used.
The multiple logistic regression (see Table 4) identified age of child, mother’s educational level, marital status, household income, place of delivery, receiving PNC and place of residence to be the determinants of EBF practice.
Table 4.
Logistic regression result on determinants of EBF.
| Factors | COR [95% CI] | p-Value | AOR [95% CI] | p-Value |
|---|---|---|---|---|
| Age of the child (months) | ||||
| <1 | 24.60[5.75, 105.33] | .000 | 34.90 [7.35, 165.65] | .000 |
| 1–2 | 20.40 [7.09, 58.71] | .000 | 34.60 [10.88, 109.99] | .000 |
| 2–3 | 9.60 [4.63, 19.92] | .000 | 11.93 [5.47, 26.05] | .000 |
| 3–4 | 4.49 [2.64, 7.63] | .000 | 6.77 [3.68, 12.45] | .000 |
| 4–5 | 5.95 [3.46, 10.22] | .000 | 6.67 [3.63, 12.20] | .000 |
| 5–6 | 1 | 1 | ||
| Mother’s education level | ||||
| No education | 1 | 1 | ||
| Primary | 1.86 [1.21, 2.87] | .005 | 2.51 [1.44, 4.37] | .001 |
| Secondary | 1.59 [0.91, 2.76] | .104 | 3.86 [1.78, 8.35] | .001 |
| Tertiary | 0.77 [0.37, 1.62] | .493 | 1.66 [0.60, 4.64] | .332 |
| Monthly household income (ETB) | ||||
| ≤1000 | 4.25 [2.40, 7.52] | .000 | 5.60 [2.55, 12.26] | .000 |
| 1001–2000 | 3.35 [1.77, 6.32] | .000 | 5.38 [2.41, 12.03] | .000 |
| 2001–3000 | 2.42 [1.16, 5.05] | .019 | 3.70 [1.54, 8.89] | .003 |
| 3001+ | 1 | 1 | ||
| Place of delivery | ||||
| Home and private health center | 0.68 [0.40, 1.16] | .160 | 0.50 [0.25, 1.01] | .054 |
| Government hospital | 1.36 [0.89, 2.06] | .153 | 1.89 [1.13, 3.15] | .015 |
| Government health center | 1 | 1 | ||
| Receiving PNC | ||||
| Yes | 1.95 1.26, 3.00] | .003 | 2.60 [1.47, 4.59] | .001 |
| No | 1 | 1 | ||
| Place of residence | ||||
| Rural | 1.79 [1.23, 2.60] | .002 | 2.22 [1.23, 4.02] | .008 |
| Urban | 1 | 1 | ||
| Marital status | ||||
| Currently not married | 3.18 [0.96, 10.59] | .060 | 4.00 [0.99, 16.28] | .052 |
| Married | 1 | 1 | ||
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; EBF, exclusive breastfeeding; ETB, Ethiopian Birr.
4. Discussion
This study aimed to identify the prevalence and determinants of EBF practice in Sheka Zone. Despite the benefits of EBF, there are a number of barriers which hinder the current practice.
In this study, the prevalence of EBF was 76%, which is comparable with studies from Hossana town (74%) and Enderta Woreda (70.2%) [11,12]. The prevalence of EBF in this study was higher than the 2016 EDHS report (58%) and villages of kangemi, Kenya (45.5%) [10,13], but lower than studies conducted in Egypt (93%) [14].
Mothers with a child aged <1 month were 34.9 times more likely to be practicing EBF than mothers with a child aged 5–6 months. As the age of the infant increased towards 6 months, EBF was less likely to be practiced. This finding is comparable with results from Jimma, Goba and Enderta Woreda [12,15,16]. Decreased EBF with increased child age is common in many developing countries as the majority of mothers believe that breast milk alone is not sufficient as the infant gets older. Mothers in developing countries have many responsibilities within the household and also in income generation activities. This leads to mothers spending increased time away from their child, especially as the child grows, and this may be another reason for the large decline in the prevalence of EBF practice in children aged 5–6 months.
Infants of mothers who delivered at home or in private health centres were 50% less likely to exclusively breastfed than mothers who delivered at government health centres (at the 10% significance level). This finding was consistent with studies performed in Debre Berhan, Ghana, and Kingoma region of west Tanzania [[17], [18], [19]]. This could be explained by the fact that mothers who delivered at health facilities received breastfeeding advice. In contrast to this finding, a study conducted in Nepal found that mothers choosing to deliver at home were more likely to remain exclusively breastfeeding for 6 months [20].
Infants of mothers with an average monthly income of ≤1000 ETB were 5.6 times more likely to exclusively breastfed than mothers with average monthly income of ≥3000 ETB. This study indicates that when the mother earned a high income, the rate of EBF decreased. This finding was consistent with studies conducted in Ethiopia and Bangladesh [21,22]. A possible explanation for this finding is that women with higher incomes are less likely to stay at home during the daytime, which may compromise the practice of EBF.
Mothers with secondary education were 3.86 times more likely to be practicing EBF than mothers with no education. This finding is consistent with previous studies [23,24] and shows that improved maternal education increases mother’s knowledge, attitudes and practices towards EBF practice, and enables them to be involved in better economic statues than their counterparts, which subsequently empowers them to resist external interferences and pressures from traditional beliefs and misconceptions.
Mothers who received PNC were 2.6 times more likely to be practicing EBF than mothers who had no PNC. This might be the result of good counselling about breastfeeding after delivery by health workers. This result was consistent with other study findings from Addis Ababa, Enderta Woreda, Egypt and Nigeria [12,14,25,26].
4.1. Limitations
This cross-sectional study was conducted in the months of June and July, which is the principal time for agricultural work in the study area and in many parts of Ethiopia. It should be noted that there may be a difference in the practice of EBF during different seasons, but it was not considered in the current study.
5. Conclusions
The prevalence of EBF in Sheka Zone in 2017 was 76%, which was higher than the national prevalence of 58% in 2016. Although the prevalence was below the WHO recommended level of 90%, the practice of EBF in the area was good.
The practice of EBF in the study area depends on age of the child, mother’s education, marital status, place of residence, income, receiving PNC and place of delivery.
The prevalence of EBF decreases as the age of the infant increases. In total, 95.3% of infants aged <1 month were exclusively breastfed, but only 45.5% of infants aged 6 months were exclusively breastfed. We recommend that health workers in health centres and hospitals provide advice about EBF and the optimal duration of EBF at PNC visits and infant vaccination appointments.
Ethical approval
Permission to undertake this research was obtained from the Sheka Zone health bureau. Informed verbal consent was also obtained from study participants in their local language after explaining the purpose of the study, benefits of partaking in the study and the right to withdraw from the study at any time during data collection. The participants were also assured the confidentiality of their responses since their names were not included in the questionnaire.
Funding
Mizan-Tepi University.
Availability of data
The datasets analysed in the current study are available from the corresponding author on reasonable request.
Author contributions
Both authors were responsible for the design of the research, supervision of the data collection, ensuring the quality of collected data, analysis of data, interpretations of the findings and drafting the manuscript. Both authors reviewed the manuscript and approved the final version.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to give our heartfelt gratitude and appreciations to Mizan-Tepi University Research Directorate Office and Tepi Campus Research Coordinator Office and Department of Statistics for granting financial and logistical support to this study. Very special thanks are extended to all health extension workers who were involved in the data collection.
References
- 1.World Health Organization . 2003. Global Strategy for Infant and Young Child Feeding. Geneva. [Google Scholar]
- 2.Peters E., Wehkamp K.-H., Felberbaum R.E., ger D.K., Linder R. Breastfeeding duration is determined by only a few factors. Eur. J. Publ. Health. 2005;16(2):162–167. doi: 10.1093/eurpub/cki199. [DOI] [PubMed] [Google Scholar]
- 3.Foo L.L., Quek S.J.S., Ng S.A., Lim M.T., Deurenbergyap M. Breastfeeding prevalence and practices among Singaporean Chinese, Malay and Indian mothers. Health Promot. Int. 2005;20(3):229–237. doi: 10.1093/heapro/dai002. [DOI] [PubMed] [Google Scholar]
- 4.Haider J., Kloos H., Haile Mariam D., Demissie T. In: The Epidemiology and Ecology of Health and Diseases in Ethiopia. Berhane Y., H/Mariam D., Kloos H., editors. Shama Books; Addis Ababa, Ethiopia: 2006. Food and nutrition. [Google Scholar]
- 5.Girma W., Genebo T. ORC Macro; Maryland, USA: 2002. Determinants of Nutritional Status of Women and Children in Ethiopia. Calverton. [Google Scholar]
- 6.Central Statistical Agency (CSA)[Ethiopia], ORC Macro . central statistics agency and ORC Macro; Maryland. USA: 2006. Ethiopia Demographic and Health Survey 2005. Addis Ababa, Ethiopia and Calverton. [Google Scholar]
- 7.UNICEF & WHO. GLOBAL BREASTFEEDING SCORECARD . 2017. Tracking Progress for Breastfeeding Policies and Programmes. [Google Scholar]
- 8.Ethiopian Federal Ministry of Health and UNICEF . Addis Ababa: Federal Ministry of Health; 2004. Forces to Promote Safe Breastfeeding. [Google Scholar]
- 9.Ministry of Finance and Economic Development, Population Department Ethiopia . Addis Ababa: Ministry of Finance and Economic Development, Population Department Ethiopia; 2008. An Annotated Bibliography of Population and Reproductive Health Researches in Ethiopia. [Google Scholar]
- 10.Central Statistical Agency (CSA) [Ethiopia] and ICF . CSA and ICF; Maryland, USA: 2016. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville. [Google Scholar]
- 11.Alemu Earsido, Abebe Wondwosen, Dereje Nebiyu. Prevalence and determinants of exclusive breastfeeding practices among infants in Hossana Town, southern Ethiopia: a community based cross-sectional study. EC Gynaecology. 2017;4(3):69–79. [Google Scholar]
- 12.Teka Bahre, Assefa Huruy, Haileslassie Kiday. Prevalence and determinant factors of exclusive breastfeeding practices among mothers in Enderta woreda, Tigray, North Ethiopia: a cross-sectional study. Int. Breastfeed. J. 2015;10:2. doi: 10.1186/s13006-014-0028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayisis M.K., Wakoli A.B. Exclusive breastfeeding practice: its implication on Nutrition status, growth and morbidity pattern among infants aged 0-6 months. Global J. Biol. Agricult. Health Sci. 2014;3(1):254–258. [Google Scholar]
- 14.Mahmoud N.A., Megahed N.M., Essam M.M., Ibraheem M.M., BelalMarrouf O., El din Hussein E.K., et al. Assessment of knowledge and practice of proper breastfeeding among mothers attending- El-Shohada primary health care units, Ismailia City. Int. J. Health Sci. 2014;2(1):70–78. [Google Scholar]
- 15.Seifu W., Assefa G., Egata G. Prevalence of Exclusive breastfeeding and its predictors among infants aged six months in Jimma Town, Southwest Ethiopia. J. Pediatr. Neonatal Care. 2013;1(3) [Google Scholar]
- 16.Setegn T., Belachew T., Gerbaba M., Deribe K., Deribew A., Biadgilign S. Factors associated with exclusive breastfeeding practices among mothers in Goba district, south east Ethiopia: a cross-sectional study. Int. Breastfeed. J. 2012;7(1):17. doi: 10.1186/1746-4358-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitiku Asfaw Maeza, Damte Argaw Mesele, Kebede Kefene Zelalem. Factors associated with exclusive breastfeeding practices in Debre Berhan District, Central Ethiopia: a cross sectional community based study. Int. Breastfeed. J. 2015;10:23. doi: 10.1186/s13006-015-0049-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tampah-Naah, Kumi-Kyereme Determinants of exclusive breastfeeding among mothers in Ghana. Int. Breastfeed. J. 2013;8(13) doi: 10.1186/1746-4358-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nkala T.E., Msuya S.E. Prevalence and predictors of exclusive breastfeeding among women in Kigoma region, Western Tanzania: a community based cross-sectional study. Int. Breastfeed. J. 2011;6(17) doi: 10.1186/1746-4358-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khanal V., Sauer K., Zhao Y. Exclusive breastfeeding practices in relation to social and health determinants: a comparison of the 2006 and 2011 Nepal Demographic and Health Surveys. BMC Publ. Health. 2013;13:958. doi: 10.1186/1471-2458-13-958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tigest S., Amare W., Yemane B. Factors associated exclusive breastfeeding practices of urban women in Addis Ababa public health centers, Ethiopia: a cross sectional study. Int. Breastfeed. J. 2015;10:22. doi: 10.1186/s13006-015-0047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joshi P.C., Angdembe M.R., Das S.K., Ahmed S., Faruque A.S.G., Ahmed T. Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: a cross-sectional study. Int. Breastfeed. J. 2014;9(7) doi: 10.1186/1746-4358-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eskezyiaw A.G., Desta H.H., Genet G.K. Exclusive breast feeding practice and associated factors in Kemba Woreda, southern Ethiopia, a community based cross-sectional study. Int. J. Sci. Technol. Soc. 2017;5(4):55–61. [Google Scholar]
- 24.Shumey A., Meaza Demissie M., Berhane Y. Timely initiation of complementary feeding and associated factors among children aged 6 to 12 months in Northern Ethiopia: an institution-based cross-sectional study. BMC Publ. Health. 2013;13:1050. doi: 10.1186/1471-2458-13-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghwass A., Ahmed D. Prevalence and predictors of 6-month exclusive breastfeeding in a rural area in Egypt. Breastfeed. Med. 2011;6(4):191–196. doi: 10.1089/bfm.2011.0035. [DOI] [PubMed] [Google Scholar]
- 26.Agho Kingsley E., Michael J Dibley, Justice I Odiase, Sunday M Ogbonmwan. Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy Childbirth. 2011;11(2) doi: 10.1186/1471-2393-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analysed in the current study are available from the corresponding author on reasonable request.