Figure 1.
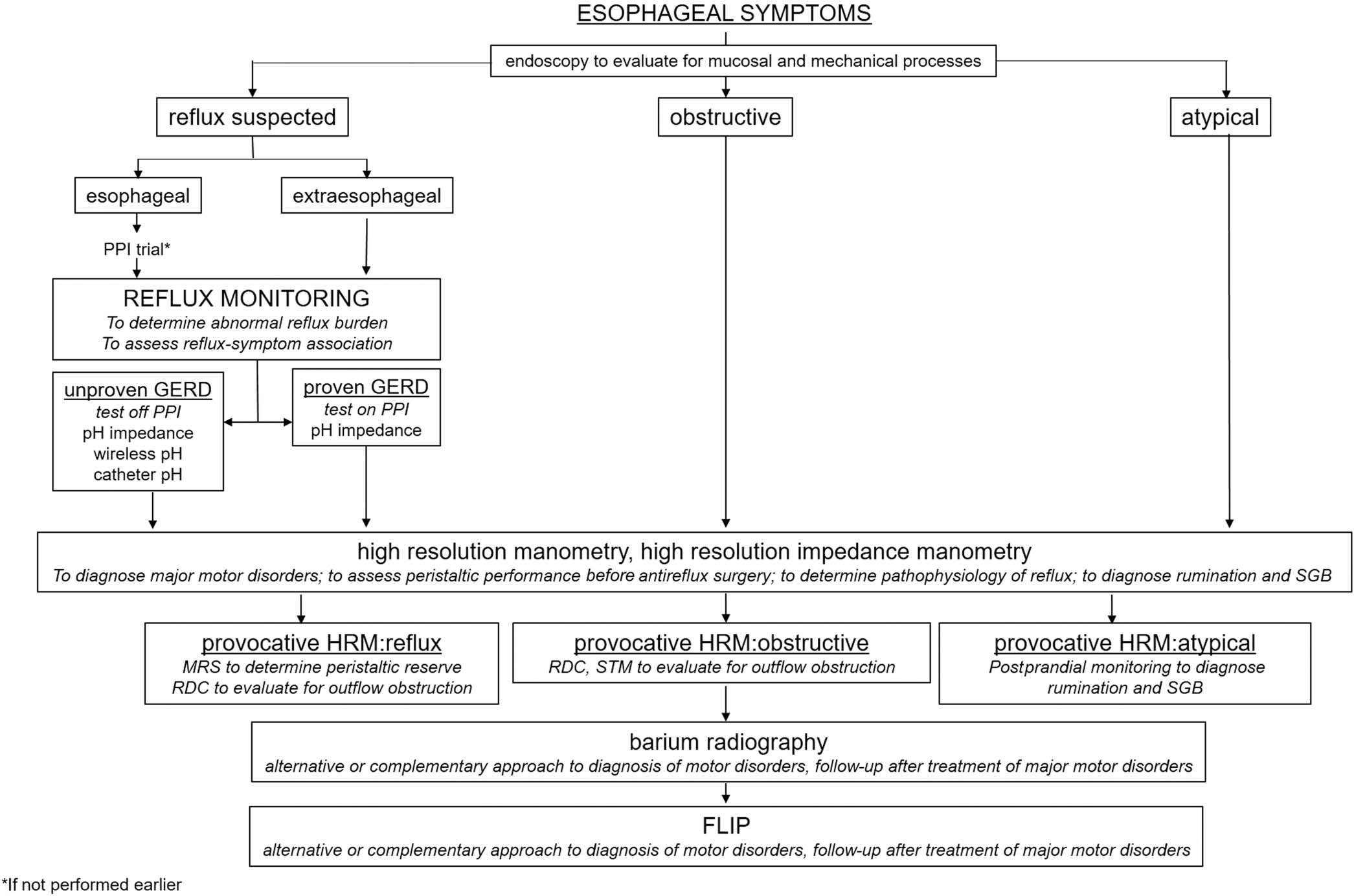
Clinical scheme for the evaluation of esophageal symptoms. Endoscopy is typically performed in the evaluation of persisting esophageal symptoms to look for a structural or mucosal mechanism of symptoms; if abnormal, management proceeds accordingly. Pathways for the evaluation of obstructive, typical, and extraesophageal symptoms suspicious for reflux and atypical symptoms (belching and rumination) differ. A PPI test may be an appropriate starting point for typical esophageal symptoms without alarm features; although this does not provide conclusive evidence of GERD, this is a pragmatic approach because most typical reflux patients do not need further invasive testing. However, objective evidence on esophageal reflux monitoring can predict the management outcome in both typical and extraesophageal reflux symptoms. Manometry helps identify major motor disorders as a mechanism for obstructive symptoms, may rule out confounding motor diagnoses in reflux presentations, and may assist with the diagnosis in atypical presentations. Provocative testing during manometry varies as goals of provocative testing also vary according to the symptom pathway. A timed upright barium swallow is a useful, safe, and inexpensive approach to evaluation of obstructive symptoms when appropriately performed. Barium studies and functional lumen imaging probe (FLIP) provide complementary value to evaluation of obstructive esophageal symptoms. GERD, gastroesophageal reflux disease; HRM, high-resolution manometry; MRS, multiple rapid swallows; PPI, proton pump inhibitor; RDC, rapid drink challenge; SGB, supragastric belching; STM, standardized test meal.
