Abstract
Purpose
To determine whether combinations of antifungal drugs are effective and safe for patients in intensive-care units.
Methods
This study compared the efficacy and safety of caspofungin (CAS), voriconazole (VOR), amphotericin B liposome (L-AmB), CAS+VOR, and CAS+L-AmB as empirical, preemptive, and targeted therapies for invasive fungal infection (IFI).
Results
Comparing the CAS, VOR, and CAS+VOR groups revealed that there were no differences in response rates between all therapy types, IFI-associated death within 90 days was less common in the CAS+VOR group (1.8%) than the VOR group (14.3%), and there were more adverse events in the VOR group than in the CAS group (P < 0.05). For empirical or preemptive therapy, the CAS group had a better response rate (80.0%) than the CAS+VOR group (47.1%), and there were more adverse events in the VOR group than in the CAS group (P < 0.05). For targeted therapy, no differences were found for efficacy and safety. There were no differences among the CAS, L-AmB, and CAS+L-AmB groups in efficacy and safety.
Conclusion
Patients who received CAS monotherapy as an empirical or preemptive therapy could achieve good outcomes. Patients who received CAS+VOR or CAS+L-AmB achieved almost the same outcomes when compared with those who received CAS, VOR, and L-AmB monotherapy as targeted therapies, but those who received CAS+VOR had a lower IFI mortality rate than did those who received VOR monotherapy.
Keywords: caspofungin, voriconazole, amphotericin B liposome, combination therapy, invasive fungal infection, intensive-care units
Introduction
The incidence of invasive fungal infection (IFI) has been increasing recently due to the increasing number of patients with transplantation, immunodeficiency, long-term application of broad-spectrum antibacterial drugs, and prolonged catheter indwelling. Patients in intensive-care units (ICUs) often suffer from various severe underlying diseases and varying degrees of organ failure, combined with the presence of various high-risk factors such as catheter indwelling and invasive operation after major surgery, leading to the increasing IFI incidence,1 which is currently 30–40%.2 IFI is currently most often caused in hospitals by invasive candidiasis (IC) and invasive aspergillosis (IA), and the proportion of infections caused by IC is as high as 70–90%, with IA accounting for 10–20%.3 Although various antifungal drugs such as triazoles, echinocandins, and polyenes have been clinically used to prevent and treat IFI, its mortality rate is still increasing. Studies found that the mortality rates of IC and IA were 10–49% and 60–90%,4 respectively, and the IFI infection rate may be higher in ICU patients. Meanwhile, there are difficulties in clinically diagnosing IFI in ICU patients, such as a low positivity rate for pathogen cultures and a high false-positive rate of serological examination, and there is currently restricted availability of new varieties of antifungal drugs used in China.1 The treatment efficacy of antifungal drug monotherapy is difficult to ensure, especially in ICU patients who experience complex changes in their physiological and pathological conditions.
Caspofungin (CAS), as a type of echinocandin drug, works by inhibiting the synthesis of β-(1,3)-D-glucan, an essential component of Candida and Aspergillus cell walls.5 Voriconazole (VOR), as a type of triazole drug, inhibits cytochrome P450-dependent 14α-lanosterol demethylation, which is a vital step in cell membrane ergosterol synthesis by fungi.6 Amphotericin B liposome (L-AmB), as a type of polyene drug, binds to the membrane sterols of fungal cells, causing barrier function impairment and loss of cell constituents.7 They operate via different mechanisms, so combining CAS and VOR (CAS+VOR) or CAS and L-AmB (CAS+L-AmB) may improve the efficacy and safety of treating IFI. In vitro studies indicated that CAS+VOR had a synergistic effect on clinical fungal isolates.8 This combination reduced the fungal burden of IFI in animal tissues compared with monotherapy using novel triazole or echinocandin drugs.9 Marr et al found that compared with VOR alone, CAS+VOR was associated with a lower mortality rate and its effects were not affected by other adverse prognostic variables in patients with hematopoietic stem-cell transplantation.10 In vitro studies and animal models have indicated that combining echinocandins and L-AmB may have a synergic or additive effect against Aspergillus spp.11,12 Clinical studies have suggested that this combination improves response to IFI.13,14 However, few studies have focused on the combined therapy of CAS+VOR or CAS+L-AmB in ICU patients.
The Infectious Diseases Society of America (IDSA) recommends CAS and VOR as initial therapies for IC15 and IA,16 respectively. L-AmB demonstrated efficacy for IFI in both animal models and human patients.13 For ICU patients, CAS was well tolerated and can be used to treat IFI.17,18 Meanwhile, the IDSA recommends echinocandins as an empirical therapy for suspected candidiasis in nonneutropenic patients in ICUs.15 VOR and L-AmB both play important roles in preventing and treating IFI in ICU patients.19 Despite its survival rate recently increasing due to advances in diagnosis and the availability of these antifungals, the outcome of IFI remains suboptimal, with an attributable mortality of up to 64%.20 Previous studies found that the outcome was successful in fewer than half of patients who received antifungal agents as salvage monotherapy (45%, 39%, and 42% for CAS,21 VOR,22 and L-AmB,23 respectively). Antifungal combined therapy has become an emerging strategy against IFI. Many experimental studies, randomized trials, and clinical series have attempted to evaluate the benefits of combination antifungal therapy.13,24–26 However, they had varying results, and the final results have not been made available in most cases. Furthermore, most of these investigations focused on patients with hematopoietic stem-cell transplantation and IA.13,24–28 Few studies have conducted in-depth analyses to evaluate the clinical efficacy and safety of treating IFI with combinations of CAS+VOR or CAS+L-AmB in ICU patients. The purpose of this retrospective analysis was therefore to assess the treatment effects, toxicity, and survival rate of combination antifungal regimens for IFI in ICU patients.
Materials and Methods
Study Design and Data Collection
This was a retrospective study and patients clinically diagnosed with IFI or diagnosed with suspected IFI who had received CAS, VOR, CAS+VOR, L-AmB, or CAS+L-AmB between January 1, 2015 and January 1, 2021 at the Second Affiliated Hospital of Xi’an Jiaotong University were collected. Proven, probable and possible IFI were defined according to the revised European Organization for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG) definitions.29 The criteria for proven IFI are as follows: for microscopic analysis of sterile material, proven IFI was characterised by histopathologic, cytopathologic, or direct microscopic examination of a specimen obtained by needle aspiration or biopsy in which hyphae or melanized yeast-like forms are seen accompanied by evidence of associated tissue damage (molds), or biopsy from a normally sterile site (other than mucous membranes) showing yeast cells (yeasts); for culture of sterile material, proven IFI was characterised by recovery of a mold or “black yeast” by culture of a specimen, or recovery of a yeast by culture of a sample obtained by a sterile procedure from a normally sterile and clinically or radiologically abnormal site consistent with an infectious disease process; for blood, proven IFI was characterised by blood culture that yields a mold, yeast or yeastlike fungi.29 Probable IFI required the presence of a host factor (recent history of neutropenia temporally related to the onset of fungal disease; receipt of an allogeneic stem cell transplant; prolonged use of corticosteroids; treatment with other recognized T cell immunosuppressants; inherited severe immunodeficiency), a clinical criterion (including criterion for lower respiratory tract fungal disease, tracheobronchitis, sinonasal infection, CNS infection and disseminated candidiasis), and a mycological criterion including direct test (cytology, direct microscopy, or culture) and indirect tests (detection of antigen or cell-wall constituents).29 Cases that meet the criteria for a host factor and a clinical criterion but for which mycological criteria are absent are considered possible IFI.29
Acute Physiology and Chronic Health Evaluation-II and Sequential Organ Failure Assessment scores were used to measure the severity of disease in the ICU patients. Their ages, sexes, and other basic information were recorded. Clinical data (imaging tests, demographic data, and underlying conditions) and laboratory data (liver and renal function) were recorded for each patient. The Ethics Committee of the hospital approved the study protocol.
Exclusion Criteria and Drug Administration
The exclusion criteria were as follows: (1) <18 years old; (2) antifungal therapy for <7 days; (3) hypersusceptible or severe intolerance to CAS, VOR, or L-AmB; or (4) concomitant treatment with other antifungal agents. The treatments corresponding to possible, probable and proven IFI are empirical, preemptive and targeted therapies, respectively. In brief, empirical therapy was mainly given to the patients with neutropenia and fever of unknown origin who continue to have fever after 4 to 6 days of appropriate antimicrobial therapy. Preemptive therapy was given to the high-risk patients who already had signs of fungal infection. Targeted therapy was antifungal therapy targeting the pathogenic fungi in patients with confirmed IFI or confirmed fungal infection, and the determination of patients who were infected with IFI was according to EORTC/MSG definitions of proven IFI29 mentioned in 2.1. For patients with empirical, preemptive and targeted therapies of IFI, whatever for antifungal monotherapy or combination therapy, CAS was administered as a loading dose of 70 mg on the first day, followed by a maintenance dose of 50 mg daily; VOR was administered as an intravenous infusion at a loading dose of 6 mg/kg twice daily on the first day, followed by a maintenance dose of 4 mg/kg q12h on day 2 and thereafter; L-AmB was administered as a dose of 5 mg/kg each day. For the combination therapies, the two antifungal drugs were infused at different times each day.
Efficacy and Safety Assessments
To evaluate the efficacy, patients who received ≥7 days of antifungal therapy were included in the study since the response rate is difficult to determine if patients receive antifungal therapy for shorter periods. A complete remission was when there was the complete disappearance of symptoms and signs caused by IFI, and computed tomography indicating that the infected sites were completely or almost completely cleared, with fungal pathogens being eliminated. A partial remission was when there was significant improvement of clinical manifestations such as symptoms and signs caused by fungal infection, and a >50% reduction of imaging shadows. The disease was considered stable in the absence of significant improvement or aggravation of symptoms, signs, and imaging changes. Finally, when the clinical symptoms and imaging manifestations were aggravated, and the fungal pathogen microbiology examination continued to be positive without contamination being excluded were considered invalid outcomes.
We recorded all patient deaths and IFI-associated deaths within 90 days. IFI-associated deaths were defined as deaths within 90 days after an IFI diagnosis in patients with histological findings, or documented microbiological or radiographic information that suggested active IFI, and neither antemortem nor postmortem cases had favorable responses to treatment.
During the study period, the investigators monitored clinical adverse events daily and assessed whether any adverse events were related to the study outcomes after 14 days. Toxicity severity was assessed according to the Common Terminology Criteria for Adverse Events (version 4.0) from the National Cancer Institute.
Statistical Analysis
Statistical analysis was performed using SPSS (version 19.0). We presented continuous data (eg, age) as median±SD (range) values and categorical data (eg, response to therapy) as proportions. Data analyses involved comparisons between the CAS, VOR, and CAS+VOR groups, and between the CAS, L-AmB, and CAS+L-AmB groups. Kruskal–Wallis and chi-square (or Fisher’s exact) tests were used to compare continuous and categorical variables, respectively. Wilcoxon rank-sum and chi-square (or Fisher’s exact) tests were used to perform the pairwise comparisons of the continuous and categorical variables, respectively. We considered differences to be statistically significant at P < 0.05. All statistical analyses and graph drawings were performed using GraphPad Prism® (version 5.02).
Results
Basic Information of the Patients
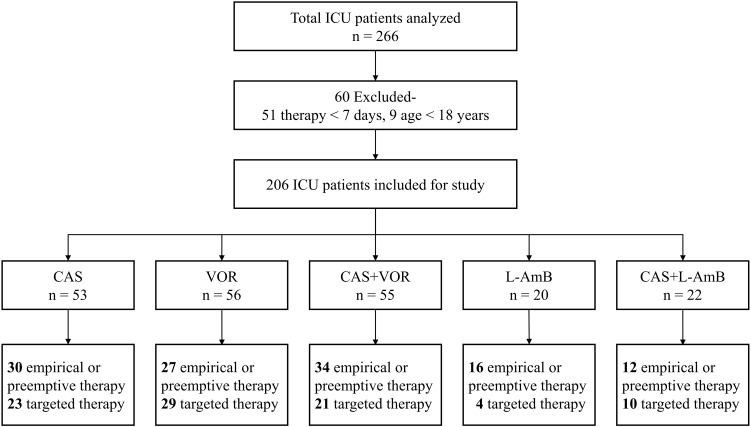
As shown in Figure 1, 266 ICU patients who were treated using empirical, preemptive, or targeted therapy for IFI were analyzed. The duration of antifungal agent therapy varied from 1 to 44 days, and their age varied from 6 to 97 years. We only assessed the treatment responses and IFI-associated mortality in patients who had received antifungal treatment for ≥7 days. Finally, 60 patients were excluded and 206 patients comprised the study population (Figure 1). CAS treatment was performed on 53 patients (empirical or preemptive therapy/targeted therapy: 30/23 patients), 56 (27/29) received VOR, 55 (34/21) received CAS+VOR (Figure 1, and Tables 1, 2, and 3), 20 (16/4) received L-AmB, and 22 (12/10) received CAS+L-AmB (Figure 1, and Tables 4, 5, and 6).
Figure 1.
Composition flowchart of ICUs. ICUs: intensive-care units; CAS, caspofungin; VOR, voriconazole; L-AmB, amphotericin B liposome. The bold texts represent the number of patients receiving empirical therapy, preemptive therapy and targeted therapy of CAS, VOR, CAS+VOR, L-AmB and CAS+L-AmB, respectively.
Table 1.
Demographics and Outcomes of All Intensive Care Unit Patients Receiving CAS, VOR or the Combination Therapy for Invasive Fungal Infectionsa
| Demographics and Outcomes | CAS (n = 53) | VOR (n = 56) | CAS+VOR (n = 55) | P-value |
|---|---|---|---|---|
| Sex (male/female) | 36/17 | 28/28 | 34/21 | 0.151 |
| Median age (range) (years) | 65 (28–97) | 65 (30–95) | 55 (19–92) | 0.011 |
| Median hospitalization days (range) | 18 (8–71) | 19 (7–58) | 21 (7–77) | 0.713 |
| Median duration of antifungal agents therapy (range) | 11 (7–32) | 11 (7–28) | 12 (8–27) | 0.283 |
| IFI diagnosis | ||||
| Definite (Candida.spp/Aspergillus.spp/others) | 23 (20/2/1) | 29 (20/9/0) | 21 (15/5/1) | 0.347 |
| Probable | 30 | 27 | 34 | 0.347 |
| Hypoproteinemia (%) | 45 (84.9) | 43 (76.8) | 41 (76.4) | 0.386 |
| Continuous renal replacement therapy (%) | 15 (28.3) | 17 (30.4) | 12 (21.8) | 0.572 |
| Liver function (Child-Pugh A/B/C) | 22/26/5 | 23/30/3 | 18/33/4 | > 0.05 |
| Median creatinine clearance rate (range) (mL/min) | 81.3 (7.7–592.0) | 106.5 (26.6–587.1) | 86.9 (10.0–478.7) | 0.136 |
| Median APACHE II score (range) | 25 (7–42) | 19 (6–34) | 21 (7–30) | 0.100 |
| Median SOFA score (range) | 12 (2–18) | 8 (1–19) | 11 (5–14) | 0.623 |
| Increase in neutrophils (On admission/ infection occurs/at the end of treatment) | 39/44/34 | 44/51/43 | 35/42/38 | > 0.05 |
| Steroid use before or during therapy (%) | 39 (73.6) | 40 (71.4) | 49 (89.1) | 0.051 |
| Mechanical ventilation during therapy (%) | 34 (64.2) | 48 (85.7) | 43 (78.2) | 0.028 |
| Prophylactic antifungal treatment prior to infection (%) | 14 (26.4) | 12 (21.4) | 22 (40.0) | 0.085 |
| Breakthrough infection (%) | 1 (1.9) | 0 (0) | 1 (1.8) | 0.548 |
| Response to therapy (%) | 37 (69.8) | 34 (60.7) | 31 (56.4) | 0.340 |
| IFI-associated death within 90 days (%) | 7 (13.2) | 8 (14.3) | 1 (1.8) | 0.035 |
| All deaths within 90 days (%) | 15 (28.3) | 14 (25.0) | 19 (34.5) | 0.547 |
| All adverse events (%) | 12 (22.6) | 30 (53.6) | 19 (34.5) | 0.003 |
| Liver (%) | 4 (7.5) | 11 (19.6) | 7 (12.7) | 0.187 |
| Renal (%) | 4 (7.5) | 15 (26.8) | 7 (12.7) | 0.021 |
Notes: aThe total number of all intensive care unit patients receiving CAS, VOR or the combination therapy was 164.
Table 2.
Demographics and Outcomes of Intensive Care Unit Patients Receiving Empirical or Preemptive Therapy of CAS, VOR or the Combination for Invasive Fungal Infectionsa
| Demographics and Outcomes | CAS (n = 30) | VOR (n = 27) | CAS+VOR (n = 34) | P-value |
|---|---|---|---|---|
| Sex (male/female) | 21/9 | 12/15 | 23/11 | 0.092 |
| Median age (range) (years) | 58.5 (28–97) | 60 (38–95) | 53 (19–85) | 0.061 |
| Median hospitalization days (range) | 19.5 (8–71) | 19 (8–41) | 18 (7–77) | 0.591 |
| Median duration of antifungal agents therapy (range) | 11 (7–32) | 11 (7–19) | 8.5 (7–27) | 0.087 |
| Hypoproteinemia (%) | 25 (83.3) | 19 (70.4) | 28 (82.4) | 0.445 |
| Continuous renal replacement therapy (%) | 6 (20.0) | 8 (29.6) | 6 (17.6) | 0.506 |
| Liver function (Child-Pugh A/B/C) | 14/14/2 | 15/10/2 | 12/21/1 | > 0.05 |
| Median creatinine clearance rate (range) (mL/min) | 81.0 (11.5–592.0) | 104.4 (26.6–556.4) | 84.9 (10.0–400.1) | 0.231 |
| Median APACHE II score (range) | 23 (7–39) | 18 (6–25) | 21 (7–25) | 0.232 |
| Median SOFA score (range) | 10 (2–16) | 7 (1–15) | 10 (5–12) | 0.503 |
| Increase in neutrophils (On admission/ infection occurs/at the end of treatment) | 20/24/18 | 21/24/23 | 20/23/23 | > 0.05 |
| Steroid use before or during therapy (%) | 20 (66.7) | 20 (74.1) | 32 (94.1) | 0.014 |
| Mechanical ventilation during therapy (%) | 15 (50.0) | 24 (88.9) | 25 (73.5) | 0.005 |
| Prophylactic antifungal treatment prior to infection (%) | 6 (20.0) | 5 (18.5) | 15 (44.1) | 0.052 |
| Breakthrough infection (%) | 0 (0) | 0 (0) | 0 (0) | — |
| Response to therapy (%) | 24 (80.0) | 16 (59.3) | 16 (47.1) | 0.025 |
| IFI-associated death within 90 days (%) | 0 (0) | 1 (3.7) | 0 (0) | 0.297 |
| All deaths within 90 days (%) | 8 (26.7) | 7 (25.9) | 16 (47.1) | 0.130 |
| All adverse events (%) | 6 (20.0) | 17 (63.0) | 11 (32.4) | 0.003 |
| Liver (%) | 2 (6.7) | 8 (29.6) | 4 (11.8) | 0.058 |
| Renal (%) | 2 (6.7) | 7 (25.9) | 4 (11.8) | 0.115 |
Note: aThe total number of intensive care unit patients receiving empirical or preemptive therapy of CAS, VOR or the combination was 91.
Table 3.
Demographics and Outcomes of Intensive Care Unit Patients Receiving Targeted Therapy of CAS, VOR or the Combination for Invasive Fungal Infectionsa
| Demographics and Outcomes | CAS (n = 23) | VOR (n = 29) | CAS+VOR (n = 21) | P-value |
|---|---|---|---|---|
| Sex (male/female) | 15/8 | 16/13 | 11/10 | 0.654 |
| Median age (range) (years) | 69 (28–87) | 67 (30–86) | 66 (25–92) | 0.208 |
| Median hospitalization days (range) | 18 (8–70) | 19 (7–58) | 28 (7–58) | 0.097 |
| Median duration of antifungal agents therapy (range) | 11 (7–27) | 11 (7–28) | 12 (7–26) | 0.969 |
| Infection type (Candida.spp/Aspergillus.spp/others) | 23 (20/2/1) | 29 (20/9/0) | 21 (15/5/1) | > 0.05 |
| Hypoproteinemia (%) | 20 (87.0) | 24 (82.8) | 13 (61.9) | 0.097 |
| Continuous renal replacement therapy (%) | 9 (39.1) | 9 (31.0) | 6 (28.6) | 0.730 |
| Liver function (Child-Pugh A/B/C) | 8/12/3 | 8/20/1 | 6/12/3 | > 0.05 |
| Median creatinine clearance rate (range) (mL/min) | 81.5 (7.7–428.7) | 108.6 (36.5–271.1) | 106.5 (15.1–478.7) | 0.473 |
| Median APACHE II score (range) | 37 (9–42) | 21 (10–34) | 25 (12–30) | 0.201 |
| Median SOFA score (range) | 15 (6–18) | 11 (7–19) | 12 (9–14) | 0.753 |
| Increase in neutrophils (On admission/ infection occurs/at the end of treatment) | 19/23/15 | 20/27/19 | 16/20/15 | > 0.05 |
| Steroid use before or during therapy (%) | 19 (82.6) | 20 (69.0) | 17 (81.0) | 0.504 |
| Mechanical ventilation during therapy (%) | 19 (82.6) | 24 (82.8) | 18 (85.7) | 1.000 |
| Prophylactic antifungal treatment prior to infection (%) | 8 (34.8) | 7 (24.1) | 7 (33.3) | 0.689 |
| Breakthrough infection (%) | 1 (4.3) | 0 (0) | 1 (4.8) | 0.514 |
| Response to therapy (%) | 13 (56.5) | 18 (62.1) | 15 (71.4) | 0.587 |
| IFI-associated death within 90 days (%) | 7 (30.4) | 7 (24.1) | 1 (4.8) | 0.084 |
| All deaths within 90 days (%) | 7 (30.4) | 7 (24.1) | 3 (14.3) | 0.504 |
| All adverse events (%) | 6 (26.1) | 13 (44.8) | 8 (38.1) | 0.377 |
| Liver (%) | 2 (8.7) | 3 (10.3) | 3 (14.3) | 0.805 |
| Renal (%) | 2 (8.7) | 8 (27.6) | 3 (14.3) | 0.212 |
Note: aThe total number of intensive care unit patients receiving targeted therapy of CAS, VOR or the combination was 73.
Table 4.
Demographics and Outcomes of All Intensive Care Unit Patients Receiving CAS, L-AmB or the Combination Therapy for Invasive Fungal Infectionsa
| Demographics and Outcomes | CAS (n = 53) | L-AmB (n = 20) | CAS+L-AmB (n = 22) | P-value |
|---|---|---|---|---|
| Sex (male/female) | 36/17 | 9/11 | 13/9 | 0.196 |
| Median age (range) (years) | 65 (28–97) | 51 (25–79) | 54 (21–87) | 0.004 |
| Median hospitalization days (range) | 18 (8–71) | 23 (8–92) | 23 (7–59) | 0.514 |
| Median duration of antifungal agents therapy (range) | 11 (7–32) | 10 (7–30) | 9 (7–44) | 0.179 |
| IFI diagnosis | ||||
| Definite (Candida.spp/Aspergillus.spp/others) | 23 (20/2/1) | 4 (3/1/0) | 10 (6/3/1) | 0.149 |
| Probable | 30 | 16 | 12 | 0.149 |
| Hypoproteinemia (%) | 45 (84.9) | 15 (75.0) | 14 (63.6) | 0.128 |
| Continuous renal replacement therapy (%) | 15 (28.3) | 4 (20.0) | 7 (31.8) | 0.707 |
| Liver function (Child-Pugh A/B/C) | 22/26/5 | 9/11/0 | 5/16/1 | > 0.05 |
| Median creatinine clearance rate (range) (mL/min) | 81.3 (7.7–592.0) | 122.8 (12.2–210.7) | 89.4 (16.5–482.2) | 0.095 |
| Median APACHE II score (range) | 25 (7–42) | 16 (4–28) | 27 (6–38) | 0.200 |
| Median SOFA score (range) | 12 (2–18) | 7 (1–14) | 15 (5 −20) | 0.722 |
| Increase in neutrophils (On admission/ infection occurs/at the end of treatment) | 39/44/34 | 13/13/9 | 15/19/14 | > 0.05 |
| Steroid use before or during therapy (%) | 39 (73.6) | 14 (70.0) | 22 (100.0) | 0.008 |
| Mechanical ventilation during therapy (%) | 34 (64.2) | 6 (30.0) | 12 (54.5) | 0.033 |
| Prophylactic antifungal treatment prior to infection (%) | 14 (26.4) | 10 (50.0) | 9 (40.9) | 0.132 |
| Breakthrough infection (%) | 1 (1.9) | 0 (0) | 0 (0) | 1.000 |
| Response to therapy (%) | 37 (69.8) | 16 (80.0) | 15 (68.2) | 0.679 |
| IFI-associated death within 90 days (%) | 7 (13.2) | 2 (10.0) | 3 (13.6) | 1.000 |
| All deaths within 90 days (%) | 15 (28.3) | 4 (20.0) | 4 (18.2) | 0.721 |
| All adverse events (%) | 12 (22.6) | 9 (45.0) | 8 (36.4) | 0.144 |
| Liver (%) | 4 (7.5) | 4 (20.0) | 1 (4.5) | 0.229 |
| Renal (%) | 4 (7.5) | 3 (15.0) | 4 (18.2) | 0.309 |
Note: aThe total number of all intensive care unit patients receiving CAS, L-AmB or the combination therapy was 95.
Table 5.
Demographics and Outcomes of Intensive Care Unit Patients Receiving Empirical and Preemptive Therapy of CAS, L-AmB or the Combination for Invasive Fungal Infectionsa
| Demographics and Outcomes | CAS (n = 30) | L-AmB (n = 16) | CAS+L-AmB (n = 12) | P-value |
|---|---|---|---|---|
| Sex (male/female) | 21/9 | 8/8 | 9/3 | 0.316 |
| Median age (range) (years) | 58.5 (28–97) | 50.5 (25–68) | 59.5 (27–74) | 0.178 |
| Median hospitalization days (range) | 19.5 (8–71) | 20.5 (8–92) | 21.5 (7–48) | 0.981 |
| Median duration of antifungal agents therapy (range) | 11 (7–32) | 8.5 (7–30) | 12.5 (7–44) | 0.195 |
| Hypoproteinemia (%) | 25 (83.3) | 12 (75.0) | 7 (58.3) | 0.237 |
| Continuous renal replacement therapy (%) | 6 (20.0) | 1 (6.3) | 3 (25.0) | 0.376 |
| Liver function (Child-Pugh A/B/C) | 14/14/2 | 8/8/0 | 5/7/0 | > 0.05 |
| Median creatinine clearance rate (range) (mL/min) | 81.0 (11.5–592.0) | 130.8 (12.2–210.7) | 89.4 (61.7–324.1) | 0.124 |
| Median APACHE II score (range) | 23 (7–39) | 14 (4–21) | 22 (6–27) | 0.256 |
| Median SOFA score (range) | 10 (2–16) | 6 (1–12) | 13 (5 −18) | 0.223 |
| Increase in neutrophils (On admission/ infection occurs/at the end of treatment) | 20/24/18 | 9/9/5 | 6/10/9 | > 0.05 |
| Steroid use before or during therapy (%) | 20 (66.7) | 11 (68.8) | 12 (100) | 0.058 |
| Mechanical ventilation during therapy (%) | 15 (50.0) | 3 (18.8) | 5 (41.7) | 0.139 |
| Prophylactic antifungal treatment prior to infection (%) | 6 (20.0) | 9 (56.3) | 6 (50.0) | 0.028 |
| Breakthrough infection (%) | 0 (0) | 0 (0) | 0 (0) | — |
| Response to therapy (%) | 24 (80.0) | 14 (87.5) | 9 (75.0) | 0.681 |
| IFI-associated death within 90 days (%) | 0 (0) | 0 (0) | 0 (0) | — |
| All deaths within 90 days (%) | 8 (26.7) | 2 (12.5) | 1 (8.3) | 0.409 |
| All adverse events (%) | 6 (20.0) | 6 (37.5) | 5 (41.7) | 0.297 |
| Liver (%) | 2 (6.75) | 4 (25.0) | 1 (8.3) | 0.237 |
| Renal (%) | 2 (6.7) | 1 (6.3) | 2 (16.7) | 0.587 |
Note: aThe total number of intensive care unit patients receiving empirical and preemptive therapy of CAS, L-AmB or the combination was 58.
Table 6.
Demographics and Outcomes of Intensive Care Unit Patients Receiving Targeted Therapy of CAS, L-AmB or the Combination for Invasive Fungal Infectionsa
| Demographics and Outcomes | CAS (n = 23) | L-AmB (n = 4) | CAS+L-AmB (n = 10) | P-value |
|---|---|---|---|---|
| Sex (male/female) | 15/8 | 1/3 | 4/6 | 0.253 |
| Median age (range) (years) | 69 (28–87) | 54.5 (41–79) | 43 (21–87) | 0.031 |
| Median hospitalization days (range) | 18 (8–70) | 39.5 (27–57) | 25 (8–59) | 0.037 |
| Median duration of antifungal agents therapy (range) | 11 (7–27) | 12.5 (10–25) | 7.5 (7–27) | 0.119 |
| Infection type (Candida.spp/Aspergillus.spp/others) | 23 (20/2/1) | 4 (3/1/0) | 10 (6/3/1) | > 0.05 |
| Hypoproteinemia (%) | 20 (87.0) | 3 (75.0) | 7 (70.0) | 0.366 |
| Continuous renal replacement therapy (%) | 9 (39.1) | 4 (100.0) | 4 (40.0) | 0.730 |
| Liver function (Child-Pugh A/B/C) | 8/12/3 | 1/3/0 | 0/9/1 | > 0.05 |
| Median creatinine clearance rate (range) (mL/min) | 81.5 (7.7–428.7) | 107.8 (62.0–144.8) | 122.3 (16.5–478.7) | 0.545 |
| Median APACHE II score (range) | 37 (9–42) | 21 (7–28) | 29 (10–38) | 0.512 |
| Median SOFA score (range) | 15 (6–18) | 9 (3–14) | 17 (7 −20) | 0.198 |
| Increase in neutrophils (On admission/ infection occurs/at the end of treatment) | 19/23/15 | 4/4/4 | 9/9/5 | > 0.05 |
| Steroid use before or during therapy (%) | 19 (82.6) | 3 (75.0) | 10 (100.0) | 0.347 |
| Mechanical ventilation during therapy (%) | 19 (82.6) | 3 (75.0) | 7 (70.0) | 0.138 |
| Prophylactic antifungal treatment prior to infection (%) | 8 (34.8) | 1 (25.0) | 7 (70.0) | 0.689 |
| Breakthrough infection (%) | 1 (4.3) | 0 (0) | 0 (0) | 1.000 |
| Response to therapy (%) | 13 (56.5) | 2 (50.0) | 6 (60.0) | 1.000 |
| IFI-associated death within 90 days (%) | 7 (30.4) | 2 (50.0) | 3 (30.0) | 0.762 |
| All deaths within 90 days (%) | 7 (30.4) | 2 (50.0) | 3 (30.0) | 0.762 |
| All adverse events (%) | 6 (26.1) | 3 (75.0) | 3 (30.0) | 0.168 |
| Liver (%) | 2 (8.7) | 0 (0) | 0 (0) | 1.000 |
| Renal (%) | 2 (8.7) | 2 (50.0) | 2 (20.0) | 0.104 |
Note: aThe total number of intensive care unit patients receiving targeted therapy of CAS, L-AmB or the combination was 37.
Demographics and Outcomes of Patients Who Received CAS, VOR, or Their Combination
Table 1 lists the demographic and clinical characteristics of all ICU patients who received CAS, VOR, or their combination, and the comparisons among them. There were demographic differences in the median age and mechanical ventilation during therapy (P < 0.05). Patients who received CAS or VOR therapy were much older than were those who received a combination (median age 65 years vs 55 years, P < 0.05). Patients who received VOR were more likely to receive mechanical ventilation during therapy than were those who received CAS (85.7% vs 64.2%, P < 0.05).
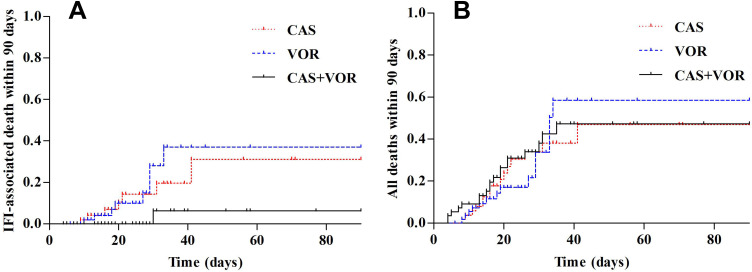
This study compared efficacy and safety in the three therapy groups. The response rates of the CAS, VOR, and combination therapy groups were 69.8%, 60.7%, and 56.4% (P > 0.05), respectively. Patients who received VOR had a higher IFI-associated mortality rate within 90 days than did those who received combination therapy (14.3% vs 1.8%, P < 0.05; Table 1 and Figure 2A), but there were no differences between the three groups in all-cause mortality rate within 90 days (P > 0.05; Table 1 and Figure 2B). Patients who received VOR had higher rates of adverse events than did those who received CAS (53.6% vs 22.6%, P < 0.05).
Figure 2.
Estimated cumulative incidence curves of invasive fungal infection (IFI) associated death within 90 days (A), and all deaths within 90 days (B) for ICU patients receiving CAS, VOR or the combination therapy (For all patients, n = 164).
Empirical or Preemptive Therapy
Table 2 lists the demographic and clinical characteristics of ICU patients who received CAS, VOR, or their combination as an empirical or preemptive therapy, and the comparisons among them. The only demographic or clinical characteristic differences were between steroid use before or during therapy and mechanical ventilation during therapy among the three patient groups (P < 0.05). Patients who received CAS+VOR used steroids before or during therapy more than did those who received CAS (94.1% vs 66.7%, P < 0.05). More patients who received VOR underwent mechanical ventilation during therapy than did those who received CAS (88.9% vs 50.0%, P < 0.05).
The response rates for empirical or preemptive therapy in the CAS, VOR, and combination groups were 80.0%, 59.3%, and 47.1% (P < 0.05), respectively. Patients who received CAS had higher response rates than did those who received the CAS+VOR combination (P < 0.05). There were no differences in breakthrough infections, IFI-associated deaths within 90 days, or all deaths within 90 days among the three groups (P > 0.05). Adverse events were more common in patients who received VOR than in those who received CAS (63.0% vs 20.0%, P < 0.05). There was no difference in liver or renal adverse events among the three groups (P > 0.05).
Targeted Therapy
Table 3 lists the demographic and clinical characteristics of ICU patients who received CAS, VOR, or their combination as targeted therapy, and the comparisons among them. There were no differences in any of the demographic or clinical characteristics among the three groups (P > 0.05).
The response rates for targeted therapy in the CAS, VOR, and combination groups were 56.5%, 62.1%, and 71.4% (P > 0.05), respectively. There were no differences in breakthrough infections, all deaths within 90 days, or all adverse events among the three groups (P > 0.05). The rate of IFI-associated deaths within 90 days was higher in patients who received CAS than in those who received CAS+VOR (30.4% vs 4.8%, P < 0.05).
Demographics and Outcomes of Patients Who Received CAS, L-AmB, or Their Combination
Table 4 lists the demographic and clinical characteristics of all ICU patients who received CAS, L-AmB, or their combination, and the comparisons among them. The only differences in demographic or clinical characteristics among the three groups were in median age, steroid use before or during therapy, and mechanical ventilation during therapy (P < 0.05). Patients who received CAS were older than were those who received L-AmB (65 vs 51, P < 0.05). More patients who received CAS+L-AmB used steroids before or during therapy than did those who received L-AmB (100.0% vs 70.0%, P < 0.05). More patients who received CAS underwent mechanical ventilation during therapy than did those who received L-AmB (64.2% vs 30.0%, P < 0.05).
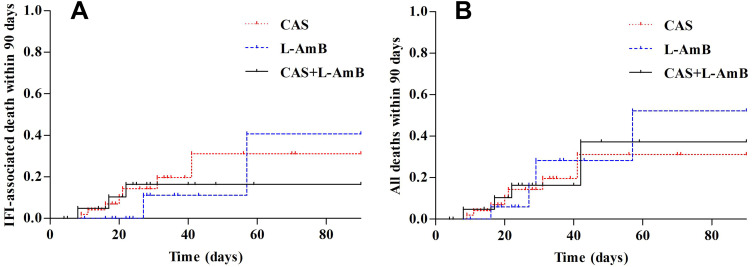
The response rates in the CAS, L-AmB, and their combination therapy groups were 69.8%, 80.0%, and 68.2% (P > 0.05), respectively. There were no differences among the three groups in responses to therapy, breakthrough infections, IFI-associated deaths within 90 days (Table 4 and Figure 3A), all deaths within 90 days (Table 4 and Figure 3B), or all adverse events (P > 0.05).
Figure 3.
Estimated cumulative incidence curves of invasive fungal infection (IFI) associated death within 90 days (A), and all deaths within 90 days (B) for ICU patients receiving CAS, L-AmB or the combination therapy (For all patients, n = 95).
Empirical or Preemptive Therapy
Table 5 lists the demographic and clinical characteristics of ICU patients who received CAS, L-AmB, or their combination as an empirical or preemptive therapy, and the comparisons between them. The only difference among the three groups in demographic or clinical characteristics was in antifungal prophylaxis prior to infection (P < 0.05). More patients who received L-AmB had antifungal prophylaxis prior to infection than did those who received CAS (56.3% vs 20.0%, P < 0.05).
The response rates for an empirical or preemptive therapy in the CAS, L-AmB, and their combination groups were 80.0%, 87.5%, and 75.0% (P > 0.05), respectively. There were no differences among the three groups in responses to therapy, breakthrough infections, IFI-associated deaths within 90 days, all deaths within 90 days, or all adverse events (P > 0.05).
Targeted Therapy
Table 6 lists the demographic and clinical characteristics of ICU patients who received targeted therapy of CAS, L-AmB, or their combination, and the comparisons between them. The only differences in demographic or clinical characteristics among the three groups were in median age and median hospitalization days (P < 0.05). Patients who received CAS were older than those who received CAS+L-AmB (69 vs 43, P < 0.05), and had fewer hospitalization days than those who received L-AmB (18 vs 39.5, P < 0.05).
The response rates of targeted therapy in the CAS, L-AmB, and their combination groups were 56.5%, 50.0%, and 60.0%, respectively. There were no differences among the three groups in responses to therapy, breakthrough infections, IFI-associated deaths within 90 days, all deaths within 90 days, or all adverse events (P > 0.05).
Discussion
IFI is a common cause of morbidity and mortality in ICU patients. Despite the use of echinocandin, triazole, and polyene drugs, the outcomes remain suboptimal and mortality attributable to IFI remains high. Clinicians have resorted to using combination antifungal therapies, but few investigative studies have involved ICU patients, and results in those involving other patients have varied. The present study aimed to determine if antifungal agents can achieve potential synergies in ICU patients in vivo, and whether combination therapy provides additional benefits such as improving response rates and reducing mortality when used as empirical, preemptive, or targeted therapy for IFI. The study also evaluated whether the toxicity of antifungal drugs increases when they are used in combination.
CAS plays a huge role in the primary and salvage treatment of patients with IFI in ICUs.30 VOR is often recommended as antifungal prophylaxis and the main treatment for IFI for patients with immunodeficiency.31 L-AmB has been administered as the gold-standard therapy for adult patients with IFI,32 which also plays an important role in preventing IFI in ICU patients.19 In clinical practice, the combined use of antifungal drugs is important for severely infected ICU patients who had failed to respond to antifungal monotherapy. In this study, we found that the response rates did not differ significantly among CAS, VOR, and their combination (P > 0.05) in ICU patients. This is consistent with Issam finding that in patients with hematological malignancy, the combination of VOR and CAS did not result in better outcomes compared with VOR alone as primary or salvage therapies.33 In the absence of prospective and well-controlled clinical trials, IDSA generally does not recommend combination antifungal agents as the primary treatment option for IA (class B, level II evidence), but they can be considered for salvage therapy.16 However, the small amount of available data from in vitro, in vivo, and nonrandomized clinical trials suggest that some forms of combination therapy have benefits in IA.34 In the present study, we found that patients who received combination therapy had a lower rate of IFI-associated deaths within 90 days than did those who received VOR (P < 0.05), and the combination group did not have more adverse events. Meanwhile, we found that the incidence of adverse events was higher in patients who received VOR than in those who received CAS (P < 0.05). However, we did not find any difference in responses to therapy, breakthrough infections, IFI-associated deaths within 90 days, all deaths within 90 days, or all adverse events among the CAS, L-AmB, and their combination groups (P > 0.05).
The clinical manifestations of IFI lack specificity, and early diagnosis is difficult. Therefore, for patients with elevated body temperature, poor response to broad-spectrum antibacterial drugs, or highly suspected fungal infection, it is recommended to apply empirical therapy as early as possible to avoid aggravation and even death caused by delayed treatment. In clinical practice, IC is the third most common bloodstream infection in ICU patients, and it is associated with high morbidity and mortality. Prophylaxis and preemptive therapy are important for ICU patients.35 For suspected IC in ICU patients, the guidelines from both the IDSA and the European Society of Clinical Microbiology and Infectious Diseases recommend using an echinocandin as the primary therapy.15,36 In this study, we found that patients who received CAS as empirical or preemptive therapy were more likely to respond than were those who received CAS+VOR (P < 0.05), and they had fewer adverse events than did those who received VOR (P < 0.05). However, there were no differences in IFI-associated deaths within 90 days and all deaths within 90 days among the three groups (P > 0.05). When compared with using azoles as empirical therapy, Cui et al found that an echinocandin as an empirical therapy can improve clinical outcomes and reduce in-hospital mortality.37 For patients who received CAS, L-AmB, or their combination as an empirical or preemptive therapy, we found that there were no differences in responses to therapy, IFI-associated deaths within 90 days, all deaths within 90 days, and all adverse events among the three groups (P > 0.05). Kontoyiannis et al found that CAS+L-AmB was well tolerated and was a good choice as a preemptive therapy for IA.26 León-Gil et al found that 84% and 81.8%38 of patients with probable IC and IA had a satisfactory clinical response, respectively. Those authors therefore considered CAS to be effective and safe in treating IFI. Appropriate empirical therapy is critical in improving outcomes.39 For ICU patients, echinocandins were recommended as the first-line empiric treatment according to recent guidelines15 because of their less-severe side effects; the present results are therefore consistent with the guideline recommendations.
Preemptive and targeted therapies are very important for ICU patients with complex physiological and pathological conditions. The IDSA suggested that echinocandins could be used as an initial therapy for managing IC.15 While the IDSA recommended VOR as a first-line therapy for IA,16 simultaneous concomitant use of two agents has not been well supported, and there the clinical data to support combination antifungal therapy over monotherapy for IC or IA are inadequate.34 In the present study, we found that for patients who received targeted therapy, there were no differences in response rates, all deaths within 90 days, or all adverse events (P > 0.05). However, we found that the CAS+VOR group had fewer IFI-associated deaths within 90 days than did the CAS group (4.8% vs 30.4%, P < 0.05). Raad et al found that in adult patients with hematopoietic malignancy, there was no significant difference in the therapeutic effect between CAS alone and CAS+VOR,40 which was consistent with our study. However, some previous studies found that combination antifungal therapy had benefits for patients with IA. Marr et al found that combination therapy could provide meaningful survival benefits when compared with VOR monotherapy in hematological malignancies infected with IA.10 Panackal et al suggested that clinicians should consider combination antifungal therapy for IA in certain situations as it had a better effect than monotherapy in salvage treatment.41 A study of lung transplant patients with Aspergillus infection found that CAS combined with VOR was safe and achieved a good treatment effect in almost all patients.42 Another study of patients with solid-organ transplantation found that CAS combined with VOR had a good effect on patients with Aspergillus infection.43
Most previous studies focused on transplant patients infected with IA, while the present study focused on ICU patients infected with IFI, and the results indicated that most patients in ICUs were infected with IC. Our results support the recommendations of the IDSA guidelines. However, for ICU patients with severe infection, combination therapy with CAS and VOR may have some advantages in reducing IFI-associated mortality. Among the three groups of patients who received CAS, L-AmB, or their combination as targeted therapy, we found no differences in responses to therapy, IFI-associated deaths within 90 days, all deaths within 90 days, or all adverse events (P > 0.05). Kontoyiannis found that the CAS+L-AmB combination might have had inadequate benefits as salvage therapy for patients infected with IA.26 Mihu et al found that the combination of echinocandins and L-AmB had no advantage in improving the therapeutic effect or reducing the mortality rate compared with either drug alone, and it would only increase the cost and not improve the outcome of patients with hematological malignancies.28 The results of some retrospective studies have also suggested that combination therapy should be further evaluated as a salvage treatment for IFI when patients receive CAS in combination with polyene or triazole drugs.44,45
Some limitations of this study should be noted. Firstly, although the total number of ICU patients was relatively large, the number of patients in each group was small, especially in the L-AmB monotherapy and CAS+L-AmB combination therapy groups. Secondly, this was a single-center study, and hence the results may not reflect the outcome of antifungal agent combination therapy in ICU patients at different institutions. Thirdly, the retrospective design may skew the results; well-designed randomized controlled trials are needed to adequately address this issue.
Conclusion
ICU patients who received CAS as an empirical or preemptive therapy were more likely to respond than were those who received CAS+VOR, and for the other therapy methods, the combinations of CAS+VOR or CAS+L-AmB did not result in better outcomes compared with CAS, VOR, or L-AmB alone. The data analyzed in this study support the recommendations of the IDSA that echinocandins should be a first-line empirical treatment and primary therapy for suspected IC, echinocandins should be an initial therapy for managing IC, and VOR should be a first-line therapy for IA in ICU patients. However, the IFI mortality rate was lower for CAS+VOR than for VOR monotherapy, and VOR monotherapy was associated with more adverse events compared with CAS monotherapy. Clinicians should therefore consider these situations when selecting antifungal agents for ICU patients. Treatment decisions should consider the response rates, IFI mortality rate, and the often severe adverse effects of antifungals (including hepatic and/or renal function impairment) when they are used in combination.
Acknowledgments
The authors sincerely acknowledge the doctors in the ICUs who helped us in this study.
Funding Statement
This work is supported by The National Natural Science Foundation of China (grant number 82003871), The General Project of the Key Research and Development Program of Shaanxi Province (grant number 2022SF-187) and The Specialized Research Fund for Faculty Training of The Second Affiliated Hospital of Xi’an Jiaotong University (grant number RC(XM)202008).
Abbreviations
IFI, invasive fungal infection; ICUs, intensive-care units; IC, invasive candidiasis; IA, invasive aspergillosis; CAS, Caspofungin; VOR, Voriconazole; L-AmB, Amphotericin B liposome; CAS+VOR, CAS and VOR; CAS+L-AmB, CAS and L-AmB; IDSA, Infectious Diseases Society of America.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The Second Affiliated Hospital of Xi’an Jiaotong University Research Ethics Committee approved the study protocol. The consent was waived due to the retrospective nature of the review. We keep the privacy of the participants confidential. We confirm that the data was anonymized and maintained with confidentiality, and the study compliance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Authors declare no conflicts of interest.
References
- 1.Lilienfeld-Toal MV, Wagener J, Einsele H, et al. Invasive fungal infection. Dtsch Arztebl Int. 2019;116(16):271–278. doi: 10.3238/arztebl.2019.0271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delaloye J, Calandra T. Invasive candidiasis as a cause of sepsis in the critically ill patient. Virulence. 2014;5(1):161–169. doi: 10.4161/viru.26187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmiedel Y, Zimmerli S. Common invasive fungal diseases: an overview of invasive candidiasis, aspergillosis, cryptococcosis, and Pneumocystis pneumonia. Swiss Med Wkly. 2016;146. doi: 10.4414/smw.2016.14281 [DOI] [PubMed] [Google Scholar]
- 4.Ibrahim-Granet OG, Rekiki A, Savers A, et al. New insights into the pathogenesis of invasive pulmonary aspergillosis: real time imaging of hypoxia and inflammation. Mycoses. 2013;56:145–146. doi: 10.1111/j.1439-0507.2012.02224.x [DOI] [PubMed] [Google Scholar]
- 5.Cortes LJ, Russi NJ. Equinocandinas. Rev Chilena Infectol. 2011;28(6):529–536. Spanish. [PubMed] [Google Scholar]
- 6.Hargrove TY, Wawrzak Z, Lamb DC, et al. Structure-functional characterization of cytochrome P450 sterol 14alpha-demethylase (CYP51B) from aspergillus fumigatus and molecular basis for the development of antifungal drugs. J Biol Chem. 2015;290(39):23916–23934. doi: 10.1074/jbc.M115.677310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fukasawa M. リソーマルアムホテリシンB. Nihon Ishinkin Gakkai Zasshi. 2005;46(4):229–231. Japanese. doi: 10.3314/jjmm.46.229 [DOI] [PubMed] [Google Scholar]
- 8.Perea S, Gonzalez G, Fothergill AW, et al. In vitro interaction of caspofungin acetate with voriconazole against clinical isolates of aspergillus spp. Antimicrob Agents Chemother. 2002;46(9):3039–3041. doi: 10.1128/aac.46.9.3039-3041.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirkpatrick WR, Perea S, Coco BJ, et al. Efficacy of caspofungin alone and in combination with voriconazole in a Guinea pig model of invasive aspergillosis. Antimicrob Agents Chemother. 2002;46(8):2564–2568. doi: 10.1128/AAC.46.8.2564-2568.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marr KA, Schlamm HT, Herbrecht R, et al. Combination antifungal therapy for invasive aspergillosis: a randomized trial. Ann Intern Med. 2015;162(2):81–89. doi: 10.7326/M13-2508 [DOI] [PubMed] [Google Scholar]
- 11.Arikan S, Lozano-Chiu M, Paetznick V, et al. In vitro synergy of caspofungin and amphotericin B against Aspergillus and Fusarium spp. Antimicrob Agents Chemother. 2002;46(1):245–247. doi: 10.1128/AAC.46.1.245-247.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clemons KV, Espiritu M, Parmar R, et al. Comparative efficacies of conventional amphotericin b, liposomal amphotericin B (AmBisome), caspofungin, micafungin, and voriconazole alone and in combination against experimental murine central nervous system aspergillosis. Antimicrob Agents Chemother. 2005;49(12):4867–4875. doi: 10.1128/AAC.49.12.4867-4875.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maertens J, Glasmacher A, Herbrecht R, et al. Multicenter, noncomparative study of caspofungin in combination with other antifungals as salvage therapy in adults with invasive aspergillosis. Cancer. 2006;107(12):2888–2897. doi: 10.1002/cncr.22348 [DOI] [PubMed] [Google Scholar]
- 14.Caillot D, Thiebaut A, Herbrecht R, et al. Liposomal amphotericin B in combination with caspofungin for invasive aspergillosis in patients with hematologic malignancies: a randomized pilot study (Combistrat trial). Cancer. 2007;110(12):2740–2746. doi: 10.1002/cncr.23109 [DOI] [PubMed] [Google Scholar]
- 15.Pappas PG, Kauffman CA, Andes DR, et al. clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62(4):e1–50. doi: 10.1093/cid/civ933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patterson TF, Thompson GR 3rd, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;63(4):e1–e60. doi: 10.1093/cid/ciw326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muilwijk EW, Schouten JA, Van Leeuwen HJ, et al. Pharmacokinetics of caspofungin in ICU patients. J Antimicrob Chemother. 2014;69(12):3294–3299. doi: 10.1093/jac/dku313 [DOI] [PubMed] [Google Scholar]
- 18.Denning DW. Echinocandin antifungal drugs. Lancet. 2003;362(9390):1142–1151. doi: 10.1016/S0140-6736(03)14472-8 [DOI] [PubMed] [Google Scholar]
- 19.De Pascale G, Tumbarello M. Fungal infections in the ICU: advances in treatment and diagnosis. Curr Opin Crit Care. 2015;21(5):421–429. doi: 10.1097/MCC.0000000000000230 [DOI] [PubMed] [Google Scholar]
- 20.Martin-Pena A, Aguilar-Guisado M, Espigado I, et al. Antifungal combination therapy for invasive aspergillosis. Clin Infect Dis. 2014;59(10):1437–1445. doi: 10.1093/cid/ciu581 [DOI] [PubMed] [Google Scholar]
- 21.Maertens J, Raad I, Petrikkos G, et al. Efficacy and safety of caspofungin for treatment of invasive aspergillosis in patients refractory to or intolerant of conventional antifungal therapy. Clin Infect Dis. 2004;39(11):1563–1571. doi: 10.1086/423381 [DOI] [PubMed] [Google Scholar]
- 22.Denning DW, Ribaud P, Milpied N, et al. Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin Infect Dis. 2002;34(5):563–571. doi: 10.1086/324620 [DOI] [PubMed] [Google Scholar]
- 23.Walsh TJ, Hiemenz JW, Seibel NL, et al. Amphotericin B lipid complex for invasive fungal infections: analysis of safety and efficacy in 556 cases. Clin Infect Dis. 1998;26(6):1383–1396. doi: 10.1086/516353 [DOI] [PubMed] [Google Scholar]
- 24.Lee DG, Lee HJ, Yan JL, et al. Efficacy and safety of combination antifungal therapy in Korean haematological patients with invasive aspergillosis. Mycoses. 2019;62(10):969–978. doi: 10.1111/myc.12972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiu KY, Liao XY, Fang JP, et al. Combination antifungal treatment for invasive fungal disease after hematopoietic stem cell transplantation in children with hematological disorders. Transpl Infect Dis. 2019;21(3):e13066. doi: 10.1111/tid.13066 [DOI] [PubMed] [Google Scholar]
- 26.Kontoyiannis DP, Hachem R, Lewis RE, et al. Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer. 2003;98(2):292–299. doi: 10.1002/cncr.11479 [DOI] [PubMed] [Google Scholar]
- 27.Haidar G, Singh N. How we approach combination antifungal therapy for invasive aspergillosis and mucormycosis in transplant recipients. Transplantation. 2018;102(11):1815–1823. doi: 10.1097/TP.0000000000002353 [DOI] [PubMed] [Google Scholar]
- 28.Mihu CN, Kassis C, Ramos ER, et al. Does combination of lipid formulation of amphotericin B and echinocandins improve outcome of invasive aspergillosis in hematological malignancy patients? Cancer. 2010;116(22):5290–5296. doi: 10.1002/cncr.25312 [DOI] [PubMed] [Google Scholar]
- 29.De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–1821. doi: 10.1086/588660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Freemantle N, Tharmanathan P, Herbrecht R. Systematic review and mixed treatment comparison of randomized evidence for empirical, pre-emptive and directed treatment strategies for invasive mould disease. J Antimicrob Chemother. 2011;66(Suppl 1):i25–35. doi: 10.1093/jac/dkq439 [DOI] [PubMed] [Google Scholar]
- 31.Jin H, Wang T, Falcione BA, et al. Trough concentration of voriconazole and its relationship with efficacy and safety: a systematic review and meta-analysis. J Antimicrob Chemother. 2016;71(7):1772–1785. doi: 10.1093/jac/dkw045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sideri G, Falagas ME, Grigoriou M, et al. Liposomal amphotericin B in critically ill paediatric patients. J Clin Pharm Ther. 2012;37(3):291–295. doi: 10.1111/j.1365-2710.2011.01288.x [DOI] [PubMed] [Google Scholar]
- 33.Silva S, Negri M, Henriques M, et al. Candida glabrata, Candida parapsilosis and Candida tropicalis: biology, epidemiology, pathogenicity and antifungal resistance. FEMS Microbiol Rev. 2012;36(2):288–305. doi: 10.1111/j.1574-6976.2011.00278.x [DOI] [PubMed] [Google Scholar]
- 34.Garbati MA, Alasmari FA, Al-Tannir MA, et al. The role of combination antifungal therapy in the treatment of invasive aspergillosis: a systematic review. Int J Infect Dis. 2012;16(2):e76–81. doi: 10.1016/j.ijid.2011.10.004 [DOI] [PubMed] [Google Scholar]
- 35.Ostrosky-Zeichner L, Shoham S, Vazquez J, et al. MSG-01: a randomized, double-blind, placebo-controlled trial of caspofungin prophylaxis followed by preemptive therapy for invasive candidiasis in high-risk adults in the critical care setting. Clin Infect Dis. 2014;58(9):1219–1226. doi: 10.1093/cid/ciu074 [DOI] [PubMed] [Google Scholar]
- 36.Cornely OA, Bassetti M, Calandra T, et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect. 2012;18(Suppl 7):19–37. doi: 10.1111/1469-0691.12039 [DOI] [PubMed] [Google Scholar]
- 37.Cui N, Wang H, Qiu H, et al. Impact of initial empirical antifungal agents on the outcome of critically ill patients with invasive candidiasis: analysis of the China-SCAN study. Int J Antimicrob Agents. 2017;50(1):74–80. doi: 10.1016/j.ijantimicag.2017.02.019 [DOI] [PubMed] [Google Scholar]
- 38.Leon-Gil C, Ubeda-Iglesias A, Loza-Vazquez A, et al. Efficacy and safety of caspofungin in critically ill patients. ProCAS study. Rev Esp Quimioter. 2012;25(4):274–282. [PubMed] [Google Scholar]
- 39.Dupont H, Mahjoub Y, Chouaki T, et al. Antifungal prevention of systemic candidiasis in immunocompetent ICU adults: systematic review and meta-analysis of clinical trials. Crit Care Med. 2017;45(11):1937–1945. doi: 10.1097/CCM.0000000000002698 [DOI] [PubMed] [Google Scholar]
- 40.Raad II, Zakhem AE, Helou GE, et al. Clinical experience of the use of voriconazole, caspofungin or the combination in primary and salvage therapy of invasive aspergillosis in haematological malignancies. Int J Antimicrob Agents. 2015;45(3):283–288. doi: 10.1016/j.ijantimicag.2014.08.012 [DOI] [PubMed] [Google Scholar]
- 41.Panackal AA, Parisini E, Proschan M. Salvage combination antifungal therapy for acute invasive aspergillosis may improve outcomes: a systematic review and meta-analysis. Int J Infect Dis. 2014;28:80–94. doi: 10.1016/j.ijid.2014.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomas A, Korb V, Guillemain R, et al. Clinical outcomes of lung-transplant recipients treated by voriconazole and caspofungin combination in aspergillosis. J Clin Pharm Ther. 2010;35(1):49–53. doi: 10.1111/j.1365-2710.2009.01061.x [DOI] [PubMed] [Google Scholar]
- 43.O’Shaughnessy EM, Meletiadis J, Stergiopoulou T, et al. Antifungal interactions within the triple combination of amphotericin B, caspofungin and voriconazole against Aspergillus species. J Antimicrob Chemother. 2006;58(6):1168–1176. doi: 10.1093/jac/dkl392 [DOI] [PubMed] [Google Scholar]
- 44.Aliff TB, Maslak PG, Jurcic JG, et al. Refractory Aspergillus pneumonia in patients with acute leukemia: successful therapy with combination caspofungin and liposomal amphotericin. Cancer. 2003;97(4):1025–1032. doi: 10.1002/cncr.11115 [DOI] [PubMed] [Google Scholar]
- 45.Marr KA, Boeckh M, Carter RA, et al. Combination antifungal therapy for invasive aspergillosis. Clin Infect Dis. 2004;39(6):797–802. doi: 10.1086/423380 [DOI] [PubMed] [Google Scholar]