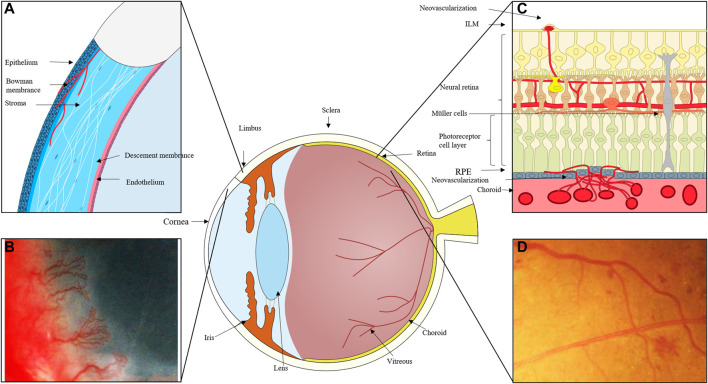
FIGURE 1.
(A) The cornea can become damaged by inflammation, trauma, and other factors, and the process of corneal repair is accompanied by the development of neovascularization. New blood vessels emerge from the corneal limbal vessels, and the corneal endothelium proliferates and migrates, growing into the corneal stroma to create corneal neovascularization, which ultimately affects vision. (B) Massive corneal revascularisation, affecting the patient’s vision. (C) In cases of retinal inflammation, ischemia, and damage to retinal homeostasis, retinal microvascular endothelial cells migrate to the damaged area and, with the help of pro-angiogenic cells like Müller and microglia, secrete pro-angiogenic factors, eventually forming new neovascular cavities. In extreme cases, these neovascular cavities can even break through the inner boundary membrane and grow into the vitreous cavity. When the choroid is exposed to stimulating circumstances like hypoxia and ischemia, choroidal microvessels expand in the direction of these locations, occasionally piercing the RPE layer. (D) Fundus photography of neovascularisation in the eye.