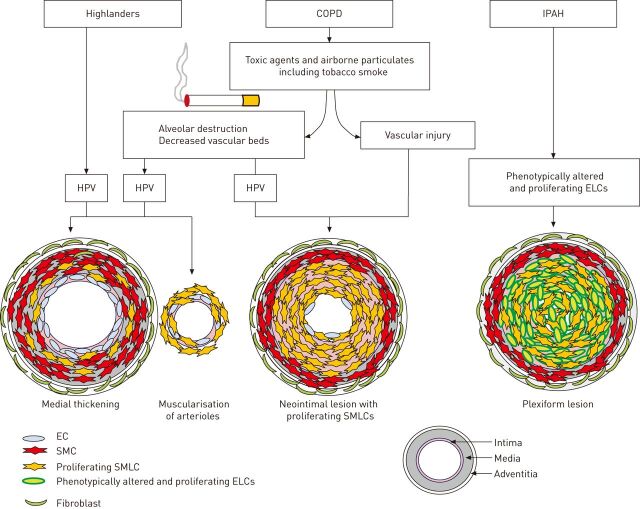
Figure 1.
A hypothetical mechanism underlying the pulmonary vascular remodelling in highlanders, chronic obstructive pulmonary disease (COPD) patients and idiopathic pulmonary arterial hypertension (IPAH) patients. In healthy highlanders, long-term alveolar hypoxia can cause pulmonary vascular alterations, including medial wall thickening and muscularisation of nonmuscularised arterioles with proliferative smooth muscle-like cells (SMLCs). These are caused by the high fluid shear stress owing to hypoxic pulmonary vasoconstriction (HPV), resulting in an elevated pulmonary arterial pressure. In the patients with COPD, both vascular injuries caused by toxic agents and airborne particulates, including tobacco smoke, and the haemodynamic changes induced by the hypoxic condition resulting from the parenchymal destruction and the decreased vascular bed, may have a role in inducing the neointimal lesions consisting of proliferative SMLCs in the pulmonary muscular arteries. These lesions are different from the pulmonary vascular alterations seen in highlanders and in the pulmonary hypertension models induced by chronic hypoxic exposure alone. In the patients with IPAH, the defining pulmonary vascular alterations are complex vascular lesions consisting of phenotypically altered and proliferating endothelial-like cells (ELCs). The distinction between the pathological features in IPAH and COPD seems to largely be the presence or absence of complex vascular lesions with phenotypically altered and proliferating ELCs. EC: endothelial cell; SMC: smooth muscle cell.