Abstract
Obstructive sleep apnoea (OSA) is a highly prevalent disorder associated with complications such as arterial hypertension, cardiovascular diseases and traffic accidents. The resources allocated for OSA are insufficient and OSA is a significant public health problem. Portable recording devices have been developed for the detection of OSA syndrome and have proved capable of providing an equivalent diagnosis to in-laboratory polysomnography (PSG), at least in patients with a high pre-test probability of OSA syndrome. PSG becomes important in patients who have symptoms and certain comorbidities such as chronic obstructive pulmonary disease or stroke, as well as in patients with a clinical history suggesting a different sleep disorder. Continuous positive airway pressure is the most effective treatment in OSA. Ambulatory monitoring of the therapeutic modalities has been evaluated to enhance the care process and reduce costs compared to the conventional approach, without sacrificing efficiency. This review evaluates the role of portable monitoring devices in the diagnostic process of OSA and the search for alternative strategies based on ambulatory management protocols.
Introduction
The International Classification of Sleep Disorders has grouped sleep disorders into eight categories [1], of which sleep-related breathing disorders and, more specifically, obstructive sleep apnoea syndrome (OSAS) are very common. OSAS is defined as a combination of symptoms such as excessive sleepiness, cognitive–behavioural or respiratory disorders, as well as others secondary to repeated episodes of upper airway obstruction during sleep. These episodes are quantified with the apnoea/hypopnoea index (AHI). Diagnosis is confirmed by an AHI of >5 events·h−1 measured by polysomnography (PSG) associated with symptoms that are related to the disease and unexplained by any other causes [2, 3]. This definition can be controversial. Considering an AHI of >5 events·h−1 as abnormal is arguable and it is probable that the threshold for abnormality differs in accordance with sex and age.
By consensus, the OSAS severity criteria are based on the AHI. Thus, a mild sleep apnoea is defined as an AHI of 5–15 events·h−1, a moderate one as an AHI of 15–30 events·h−1 and a severe one as >30 events·h−1 [4].
Many studies have shown significant associations between OSAS in adults and daytime hypersomnolence, hypertension, traffic accidents, cardiovascular and cerebrovascular diseases, diabetes and deterioration in quality of life, and it is also related to excess mortality [5–11]. Fortunately, effective treatment is available, most commonly in the form of continuous positive airway pressure (CPAP). Furthermore, OSAS in children is mainly associated with intermittent hypoxia, sleep fragmentation and alveolar hypoventilation, which can lead to delayed growth and development, pulmonary hypertension, systemic arterial hypertension and alterations in learning and behaviour [12]. The most common risk factor for childhood sleep apnoea is adenotonsillar hypertrophy and adenotonsillectomy is the usual first-line treatment [13].
OSAS is a very prevalent disease and is considered a public health problem of the first order. According to the Wisconsin sleep cohort study [14], 24% of males and 9% of females aged 30 to 60 years meet the diagnostic criteria. This prevalence is based on a cut-off of AHI ≥5 events·h−1. If symptoms are included, the prevalence of OSAS was 4% of males and 2% of females. Other authors have published similar results in other countries [15]. The prevalence of OSAS in adults increases with age and obesity, the latter being one of the most important risk factors for OSAS. The dramatic increase in obesity over the past 30 years, the increasing longevity of the population and the increasing awareness of OSAS as a risk factor have exponentially increased the number of patients for evaluation. This growth in demand has not been accompanied by any improvements in the approach to this problem.
We know from various studies [3, 14, 16] that >75% of patients with OSAS are either undiagnosed or untreated. Although PSG is considered the gold standard for the diagnosis, access to this procedure is limited because it requires special institutions and trained technicians and is relatively expensive. This problem of timely access is going to produce undiagnosed and undertreated sleep apnoea, as well as excessively long waiting lists [17, 18]. Accordingly, in the Wisconsin sleep cohort study [16], 93% of females and 82% of males with moderate-to-severe sleep apnoea did not receive diagnoses.
The high prevalence of OSAS and the great demand for examinations mean that PSG cannot be used in all patients. In order to deal with these difficulties, portable recording devices have been developed for the detection of OSAS [2, 19–22], and have proved capable of providing an equivalent diagnosis to in-laboratory PSG, at least in patients with a high pre-test probability of moderate-to-severe OSAS [23–25]. Moreover, screening questionnaires have been used to identify patients with a high risk of OSAS who may benefit from receiving diagnosis and management as quickly as possible [26–34].
Types of sleep studies
In 1994, the American Academy of Sleep Medicine (AASM) [35] classified sleep studies into four types, based on the number and types of physiological variables recorded (table 1).
Table 1. Types of sleep studies (6-h overnight recording minimum).
| Type 1 | Type 2 | Type 3 | Type 4 | |
| Number of leads | ≥7 | ≥ 7 | ≥ 4 | 1–2# |
| Types of leads | EEG, EOG, EMG, ECG, airflow, effort, oximetry | EEG, EOG, EMG, ECG, airflow, effort, oximetry | ECG, airflow, effort, oximetry (at least two channels are respiratory movements or respiratory movement and airflow) | Oximetry and other (usually airflow) |
| Body position | Objectively measured | Optional | Optional | Not measured |
| Setting | Attended (usually in a sleep centre) | Unattended | Attended or unattended |
Attended or unattended |
| Description | Standard PSG performed in a sleep laboratory (reference standard to which the other monitors are compared) | Comprehensive portable PSG | Portable testing limited to sleep apnoea | Continuous recording of 1–2 signals |
EEG: electroencephalogram; EOG: electrooculogram; EMG: electromyogram; PSG: polysomnography. #: sometimes type 4 may measure ≥3 parameters, but does not meet all the criteria of a higher category. Modified from [35].
Type 2, 3 and 4 monitors can be applied with portable monitoring at home (ambulatory monitoring). Nevertheless, these devices can vary as regards the signals recorded and the sensors. Moreover, the methods of scoring, the criteria used to define respiratory events, particularly hypopnoeas, and the cut-off of the AHI used to establish severity of OSAS can give rise to further variability [36, 37].
In this respect, the AASM recommends that portable monitors use the same sensors normally used for in-laboratory PSG. However, many studies have compared type 3 monitor recordings with PSG using older model monitors that only had the oro-nasal thermistor signal (a less sensitive indicator of airflow reduction than nasal pressure signal) and this difference may be another reason for the discrepancy between the AHI in PSG and in home respiratory polygraphy (RP) [38].
One important factor in the comparison of PSG and RP recording can be differences between the manual scoring of recording, the manual editing of automatic scoring (“sequential RP scoring”) and the totally automated process. Manual scoring is superior to automated scoring [39]. The sequential RP scoring protocol had a similar cost to manual scoring and both were a cheaper alternative to PSG [36, 37, 39]. Finally, another aspect that must be considered with unattended portable monitors is the data loss, as there are reports of a data loss of 3–18% for type 3 monitors and of 7–10% for oxygen saturation measurements in type 4 monitors [36]. For all these reasons, studies using a specific portable monitor cannot be generalised to other devices, thus reducing our capacity to perform meta-analyses and evidence-based reviews. Despite these circumstances, a systematic review conducted in 2003 [36] did evaluate portable sleep study systems in OSAS diagnosis. The authors observed that portable monitoring devices had variable sensitivities (31–100%) and variable specificities (48–100%). This variability of the devices and the limited evidence available until this review [36] were the principal causes for not conclusively recommending all the portable devices in the OSAS diagnosis [36].
However, many subsequent studies have confirmed the overall usefulness of these portable monitoring devices [2, 23, 37, 40, 41]. In fact, one study found that it was better to use home testing sooner, rather than waiting for in-laboratory PSG, in severe OSAS patients, resulting in a significant improvement in daytime sleepiness and quality of life and demonstrating a significantly lower incremental cost–effectiveness ratio and a rapid application of treatment in these patients [37].
In 2007, the AASM [23] concluded, after an exhaustive review of the literature, that the use of home portable monitoring had finally been approved. The authors recommended that unobserved registers with type 2–3 monitors can be used as an alternative to PSG diagnosis in patients with a high probability of moderate-to-severe OSAS and no significant medical comorbidities. Unattended portable monitoring can be as accurate as PSG for diagnosis in selected populations [26, 27, 32–34]. The AASM also issued other recommendations for the use of unattended portable monitors (table 2). In contrast, the evidence regarding type 4 monitors was weaker.
Table 2. Recommendations for unattended portable monitoring.
| 1. PM is performed with a comprehensive sleep evaluation with different screening questionnaires and clinical scores |
| 2. Supervised by a practitioner with sleep medicine certification and performed under the auspices of an AASM-accredited sleep medicine centre |
| 3. Record airflow, respiratory effort and blood oxygenation channels and use the same biosensors as laboratory PSG |
| 4. Display of raw data for manual scoring or editing of automated scoring (sequential scoring) |
| 5. Alternative to PSG for OSAS diagnosis in patients with high pre-test probability of moderate-to-severe OSAS |
| 6. It is not appropriate for OSAS diagnosis if patient presents significant comorbidities |
| 7. It is not appropriate for screening of asymptomatic populations |
| 8. Alternative for OSAS diagnosis in patients for whom in-laboratory PSG is not possible (immobility, critical illness, etc.) |
| 9. If PM is negative in patients with a high pre-test probability of moderate-to-severe OSAS, in-laboratory PSG should be performed to rule out any false-negative study |
| 10. Monitor the response to non-CPAP treatments for sleep apnoea (i.e. weight loss or intra-oral device) |
PM: unattended portable monitoring; AASM: American Academy of Sleep Medicine; PSG: polysomnography; OSAS: obstructive sleep apnoea syndrome; CPAP: continuous positive airway pressure. Information from [23].
Other official documents by Medicare and Medicaid Services [42, 43] have recognised that attended or unattended type 2 and 3, and even type 4 monitors (with at least three channels), were acceptable as diagnostic methods for prescribing CPAP in patients who had symptoms of OSAS, regardless of whether they were followed inside or outside a sleep unit. This strategy is then mainly validated and accepted in patients with high pre-test probability.
Traditionally, the approach used to validate portable monitoring has been to compare it with a reference standard PSG. The limitation of this approach is that it assumes that in-laboratory PSG is the gold standard test for diagnosing sleep apnoea. We know that patients frequently do not sleep as well in a sleep laboratory as they do at home (“first night effect”). Furthermore, the instrumentation is more extensive than that of most home tests and may induce changes in sleep, for example, patients in a laboratory usually spend more time sleeping supine, thereby increasing the AHI in some patients. These factors can affect the real quality of sleep.
Because of this variability in sleep studies, Collop et al. [44] have recently reviewed the classification of types of sleep studies published in 1994. A new classification system, based on measurements of Sleep, Cardiovascular, Oximetry, Position, Effort and Respiratory parameters (SCOPER categorisation), details the type of signals measured by these devices (table 3).
Table 3. SCOPER categorisation.
| Sleep | Cardiovascular | Oximetry | Position | Effort | Respiratory |
| S1 | C1 | O1 | P1 | E1 | R1 |
| Three EEG channels# with EOG and chin EMG | >1 ECG lead | Oximetry (finger or ear) with recommended sampling¶ | Video or visual position measurement | Two RIP belts | Nasal pressure and thermal device |
| S2 | C2 | O1x | P2 | E2 | R2 |
| <3 EEGs with or without EOG or chin EMG | Peripheral arterial tonometry | Oximetry (finger or ear) without recommended sampling (per scoring manual) or not described | Nonvisual position measurement | One RIP belt | Nasal pressure |
| S3 | C3 | O2 | E3 | R3 | |
| Sleep surrogate: e.g. actigraphy | Standard ECG measure (one lead) | Oximetry with alternative site (e.g. forehead) | Derived effort | Thermal device | |
| S4 | C4 | O3 | E4 | R4 | |
| Other sleep meaures | Derived pulse (typically from oximetry) | Other oximetry | Other effort measures (including piezo belts) | End-tidal CO2 | |
| C5 | R5 | ||||
| Other cardiac measures | Other respiratory measures |
EEG: electroencephalogram; EOG: electrooculogram; EMG: electromyogram; RIP: respiratory inductance plethysmography. #: frontal, central and occipital; ¶: proper oximetry sampling is defined as 3-s averaging and a mínimum of 10-Hz sampling rate (25 Hz is desirable). Modified from [44].
We shall now review the evidence on ambulatory OSAS monitoring in terms of diagnosis, management and cost-effectiveness, based on unattended type 2, 3 and 4 sleep studies. We have ruled out papers limited to attended monitoring devices and comparisons between sleep laboratory-based techniques, we have also discarded papers that do not clearly state the type of equipment used.
Type 2 sleep study (unattended portable PSG)
Diagnostic accuracy
The AASM approved the usefulness of unattended portable monitors (type 2–3 devices) to diagnose OSAS in patients with a high pre-test probability without comorbidities [23]. The advances in portable monitoring devices have made it possible to record complex signals in an unattended setting, such as home portable PSG. They are more expensive than other portable devices, however, and need much more time from the expert technicians and physicians who read the registers and report the results. The standards for obtaining and analysing this unattended PSG were published by the Sleep Heart Health Study (SHHS) [45]. The comparison of in-laboratory PSG with home monitoring showed no significant difference in the mean AHI, and the portable device obtained a reasonably low failure rate in one large study (SHHS) [46].
Another study [47] reported an acceptable sensitivity and specificity with few false-positive results (3%); however, a high rate of data loss (20%) and false-negative results (15%) were reported, and this study [47] did not have a good evidence level. In a randomised study, Campbell and Neill [48] proved that unattended home PSG is a valid alternative to in-laboratory PSG. Sleep quality was similar in both arms and the AHI was significantly different, with an average underestimate of 5.1 events·h−1 in home PSG. This difference only affected the diagnosis in three patients, but treatment advice did not change. With regard to preference, 50% patients preferred home PSG.
Interest in the clinical pathway for OSAS diagnosis and treatment
Although these devices have demonstrated a performance similar to that of in-laboratory PSG, patient's problems with the application of the bipolar electrodes require the presence of a technician to set up the test at home, so they are perhaps not practical for clinical purposes. Type 2 monitors may be useful in a hospital setting (obviating the need to go to a sleep centre), but more studies are needed to ascertain their role in the management of OSAS patients.
Costs
Three studies [47–49] have shown reduced costs with this device versus attended PSG, based on the assumption that overnight staff and laboratory expenses could be eliminated with a portable monitor. However, the 20% failure rate with this ambulatory device was not accounted for. Campbell and Neill [48] estimated that out of every 100 in-laboratory PSGs performed, 6.7 studies would require a repeated night. Bearing in mind that the cost of home-based PSG is 70% that of an attended in-laboratory PSG, home PSG would therefore save 25%.
However, the lack of studies in this area makes it difficult to draw any conclusions about possible savings with this type of portable monitoring.
Type 3 sleep study (unattended RP)
Diagnostic accuracy
Diagnostic accuracy at home in the situation of high pre-test probability
The most commonly used ambulatory monitoring devices are type 3 monitors. Traditionally, noninferiority studies have tried to compare them with in-laboratory PSG for the diagnosis of OSAS. They have shown positive results, at least in patients with a high pre-test probability of moderate-to-severe OSAS, suggesting that unattended RP is a feasible option with an equivalent diagnosis to in-laboratory PSG and good concordance (>80% agreement) [23, 50–53].
Unfortunately, unattended RP underestimates the AHI, given that it records the number of apnoeas/hypopnoeas per hour of recording instead of per hour of sleep and, moreover, RP cannot identify arousal and, consequently, cannot incorporate this criterion into the definition of hypopnoea. The AASM recommends two alternative definitions of hypopnoea, one including arousal and the other excluding it [23]. In this respect, Masa et al. [54] concluded that although adding surrogate arousal (defined as a hyperventilation following flow reduction) to home respiratory polygraphy (HRP) can produce a modest improvement in the AHI, this alteration is not clinically important. Furthermore, wrist actigraphy was used to calculate the total sleep time in HRP and improve the agreement between HRP and PSG, although this action only slightly improved the HRP results [50].
Various studies have validated the diagnosis of OSAS with unattended RP compared with in-laboratory PSG. Ballester et al. [20] validated a home portable respiratory recording device in a general population with a high level of agreement between both methods, despite using a thermistor for oronasal airflow. For a PSG cut-off point of 10 events per hour of sleep, a portable respiratory recording device of 6 events per hour showed a sensitivity and specificity of 95% and 92%, respectively. Moreover, other authors obtained similar results [55–58]. When the diagnostic accuracy of a type 3 monitor was analysed [59], the authors found no differences in the AHI per hour in bed between PSG and home RP (2±5 events·h-1 in bed), although there were differences per hour of sleep. Most patients were successfully classified by these portable monitoring studies, but 47% of patients would have required further study if we had used home portable monitoring. With a similar study design, Reichert et al. [60] validated a different home portable device. They obtained a sensitivity and specificity of 91% and 83%, respectively, using a cut-off AHI of 15 events·h−1 for home studies. Following the validation studies, other authors [61–64] compared various portable monitoring devices with PSG, obtaining good agreement with corrected AHIs (apnoea/hypopnoeas/total time in bed). Su et al. [61] also found no differences in the AHI obtained by the two methods (portable monitoring device versus PSG) in a laboratory setting. No conclusions could be drawn, however, with regard to the reliability of this device in the home setting.
A large randomised study was performed to determine the diagnostic efficacy of HRP compared with in-laboratory PSG and the cost of telematic services for data transmission [52]. With a sensitive AHI cut-off point of ≤5 events·h−1, HRP effectively excluded OSAS, while with a specific cut-off of ≥10 events·h−1, HRP confirmed OSAS. Therefore, HRP is a significantly cheaper alternative to PSG in these patients.
From the prevalence point of view, OSAS is so frequent that the use of unattended RP has greatly increased in recent years, particularly in sleep nonreference centres. A randomised study [65] reported a good concordance (86.9%) between nonreference centres and sleep reference centres (with PSG) in therapeutic decisions. Therefore, RP evaluated by a respiratory physician in a nonreference centre is capable of managing and treating a large number of patients.
Diagnostic accuracy in special populations
Although many studies have validated portable monitoring devices in adults with a high clinical probability of OSAS (mainly males), only a few have evaluated their feasibility in other populations.
Curiously, there are very few studies in the female population. Gjevre et al. [66] evaluated the usefulness of these devices in females with a suspicion of a high risk of OSAS. They found the highest level of agreement with an AHI of ≥10 events·h−1. They could thus diagnose with reasonable certainty and start CPAP therapy in females with a high clinical suspicion of OSAS and an AHI ≥10 events·h−1.
Other authors have found a good correlation and diagnostic accuracy between home portable monitoring (Stardust II; Philips Healthcare, Best, The Netherlands) and PSG in the elderly population (≥65 years) with a high clinical probability of OSAS [67]. Moreover, the authors observed that >70% of these patients had severe OSAS.
Another problem that has been observed is the underdiagnosis of OSAS in children, where an early diagnosis could have important consequences for prevention. Although PSG is the gold standard diagnostic method in children, its standardisation is still inadequate. Meanwhile, Alonso Alvarez et al. [53] have reported the reliability of RP for the diagnosis of OSAS in children. There was a high rate of diagnostic agreement between RP and PSG (84.9%) and a high correlation (89.4%) for an AHI ≥3 events·h−1 in PSG and an respiratory disturbance index (RDI) ≥3 events·h−1 in RP.
In another area, Quintana-Gallego et al. [68] validated a type 3 monitor (Apnoescreen II; Erich Jaeger GMBH & CoKg, Würzburg, Germany) for diagnosis of sleep disordered breathing in stable heart failure patients. Using AHI cut-off points of ≥5, ≥10 and ≥15 events·h−1, the diagnostic accuracy of HRP versus PSG was 78–84%, 68–82% and 88–97%, respectively. HRP showed good diagnostic accuracy for OSAS, as well as distinguishing between central and obstructive events. Furthermore, Sériès et al. [69] demonstrated that overnight home oximetry is a sensitive and specific tool for identifying sleep apnoea in patients with chronic heart failure, but not for distinguishing between obstructive and central events.
In patients with OSAS and chronic obstructive pulmonary disease (COPD) (overlap syndrome), there is no evidence to support the use of portable devices to diagnose OSAS. In this respect, Oliveira et al. [70] compared the accuracy of a home portable device versus PSG in these patients and they found a large amount of data loss in the recordings (39% with home devices and 22% with PSG). They therefore could not confirm its usefulness in these patients.
OSAS process management and treatment decision
Type 3 monitors can perform a sleep apnoea diagnosis in patients with a high pre-test probability of OSAS, but is this enough to justify a therapeutic decision? Making a diagnosis of OSAS is very different from choosing a treatment.
Several studies have compared standard PSG diagnosis and titration versus home portable strategies with ambulatory CPAP titration (auto-CPAP) in high patients with a pre-test probability of moderate-to-severe OSAS [71–73]. The authors found no clinical differences between the two groups. Furthermore, CPAP adherence was higher in the home group. Thus, the standard procedure in these patients does not have any advantages over the ambulatory approach in the management of OSAS. Furthermore, a simplified nurse-led model of care and home auto-CPAP was compared with traditional physician-directed care involving PSG in patients with suspicion of OSAS and certain oxygen desaturations [74]. No significant differences were found between the two arms in clinical outcomes, such as the Epworth Sleepiness Scale score and CPAP adherence and patient satisfaction. Thus, a simplified nurse-led management was not inferior to physician-led care, although these nurses had spent more time with patients than the other group and the authors did not perform a PSG in the nurse-led group to assess the effectiveness of CPAP. Similarly, Andreu et al. [24] confirmed that nurses could undertake ambulatory management in patients with a high clinical suspicion of OSAS, with no significant differences in hospital follow-up but with noticeable financial savings.
Most guidelines recommend CPAP, depending on clinical symptoms, comorbidities and AHI based on PSG. Masa et al. [75] studied the therapeutic decisions made by a physician on the basis of HRP or in-laboratory PSG and clinical variables in patients with an intermediate-to-high suspicion of OSAS. There was a better agreement between HRP and PSG when the AHI was higher (≥30 events·h−1), but the results were less satisfactory in patients with mild-to-moderate AHI. The authors therefore recommend CPAP treatment by HRP only in patients with severe sleep apnoea.
Pneumologists normally adjust CPAP pressure according to attended in-laboratory PSG titration. There are currently several approaches to CPAP initiation, including unattended auto-CPAP, CPAP titration based on predicted formula split-night procedure and attended laboratory PSG. Overall, studies comparing these different methods have shown similar improvements in symptoms, the capacity to eliminate respiratory events and adherence to treatment [76–78]. In this respect, using auto-CPAP at home with the device for only one night (using percentile 90) and predicted formula titration with domiciliary adjustment can replace standard titration in the majority of patients [77]. The AASM [79] also approved unattended auto-CPAP to determine a fixed CPAP treatment pressure for patients with moderate-to-severe OSAS and no significant comorbidities. In summary, auto-CPAP titrations have been successfully integrated into the ambulatory management of patients with OSAS. Nevertheless, if central sleep apnoea, relevant gas exchange abnormality, significant comorbidities or uvulopalatopharyngoplasty are present, even in severe nasal obstruction, standard CPAP titration should be considered [77, 79].
Costs
The last HRP studies have revealed both advantages and disadvantages to costs (table 4). Perhaps the main advantage is that this type of study does not require a technician to be in attendance. HRP can be performed in patients with a high probability of OSAS with good efficacy and cost in both diagnosis and treatment [23, 50–53, 75]. There is, however, a scarcity of formal analyses of both direct and indirect costs.
Table 4. Advantages and disadvantages of portable monitoring devices (PMDs).
| Advantages |
| Accessibility |
| Improved patient access |
| Easy self-application of monitoring (no technician required) |
| Possible impact on waiting list |
| Cost |
| Acceptability for patients |
| Patients with possible anxiety or who are uncomfortable sleeping alone in a laboratory bed, under medical guidance |
| Patient sleeps in his/her own bed |
| The effect of environmental factors on sleep variables is still unknown (the sleep pattern is probably more representative of everyday sleep) |
| Disadvantages |
| Reliability |
| Unattended portable monitoring is subject to data loss |
| Equipment malfunction |
| Sensor disconnections |
| Patient or family interference |
| Telephone-line interference (during modem transfer or playback) |
| Diagnostic limitations |
| Nonsleep-apnoea diseases |
| Underestimate of the AHI |
| No electrophysiological signals needed to score and stage sleep, no detection of hypopnoeas associated with arousals and no evaluation of the quality of sleep |
| PMD can vary according to: |
| Number and types of signals |
| Sensors used |
| Methods of scoring |
| Criteria used to define respiratory events |
| Cut-off of the AHI used to define diagnosis and severity of OSAS |
AHI: apnoea/hypopnoea index; OSAS: obstructive sleep apnoea syndrome.
Parra et al. [58] calculated the direct and indirect costs of this portable monitoring versus PSG; the reported cost of home portable monitoring (with or without a technician) was nearly one-third that of full-PSG. Other cost studies have demonstrated savings of 25–50% compared with a full PSG. These studies included the expenses incurred by a nurse visiting patients at home and telemedicine approaches to the transmission of data from portable monitoring devices [52, 53, 72, 74, 80]. Some studies, however, have evaluated the costs of HRP compared with PSG on the basis of simulated models of hypothetical cohorts of patients, including diagnosis, CPAP titration and treatment adherence, with contradictory results [81–83]. Nevertheless these studies were not carried out on a real cohort of patients and the assumptions made in these analyses may not be applicable to clinical practice. Pietzsch et al. [84] compared three different strategies (full-night PSG, split-night PSG and unattended portable home monitoring) using a hypothetical cohort (a decision-analytic Markov model), and the most cost-effective strategy for diagnosing OSAS patients, surprisingly, was full-night PSG. This was due to its better diagnostic accuracy and lower number of false-negative and false-positive results (although these authors may have exaggerated the impact of false-negative and false-positive test results). In any case, these studies question the notion that home studies should automatically be considered the most cost-effective test just because the upfront costs are lower than those of PSG.
With regard to CPAP titration, although several papers have shown similar improvements in clinical outcomes with different CPAP titration approaches [72, 76, 77], more studies are needed to evaluate cost-effectiveness. However, auto-CPAP and predicted formula titration could lead to considerable savings and significant reductions in waiting lists. In this respect, McArdle et al. [85] reported that the total costs for auto-CPAP titration was much lower than those of laboratory auto-CPAP (less than one-third).
Type 4 sleep study (unattended super-simplified systems)
General characteristics of type 4 monitors
Nowadays, there are many different type 4 monitors but unfortunately they have not been standardised. Some record single channels of nasal pressure [86–88], peripheral artery tone [89], tracheal sound [90] and transthoracic impedance or oxygen saturation [69, 91], while others record combinations of variables [92–97]. We do not yet know, however, which signals or channels are essential for diagnosis in OSAS patients.
Type 4 monitors are supersimplified devices with 1–2 channels (usually oximetry and/or airflow). These devices may measure three or more parameters, but do not meet all the criteria of a higher category device [22].
Diagnostic accuracy
Nocturnal oximetry has been used as a screening method as it can demonstrate the presence of apnoea or hypopnoea, but does not distinguish between central or obstructive disorders; it also does not detect events without desaturation. Its use as a single diagnostic method is, therefore, not recommended.
None of these type 4 devices records sleep state and it is common to underestimate both the AHI and arousals. Various surrogate measures of arousals, such as actigraphy, have tried to improve the arousal index and possibly the agreement between OSAS diagnosis and PSG [50, 98–101]. Any improvement would only be slight, however, and not clinically important, as Masa et al. [54] reported in the case of a type 3 device.
In recent years, these devices have been validated with PSG at different sensitivities and specificities, depending on the device or the AHI cut-off value [34, 89, 102–110].
Several studies have evaluated the diagnostic accuracy of single-channel nasal airflow pressure transducers with oximetry and pulse to identify patients with a high pre-test probability of OSAS in comparison with in-laboratory PSG [103, 106–112]. Overall, the AHI correlation was similar in both these two methods. The predictive values were especially high at AHI ≥10 events·h−1 [108] and AHI ≥20 events·h−1 [109–111]. Moreover, the addition of an oximetry channel to nasal flow did not increase the accuracy of diagnosis [107]. Thus, single-channel nasal airflow pressure can be used as an accurate alternative diagnostic tool either at home or in a sleep clinic in this population.
Another strategy focused on improving the underdiagnosis of OSAS in primary care by using simplified models (obstructive sleep apnoea (OSA)-50 questionnaire followed by home single-channel nasal airflow pressure oximetry and validated against full PSG). The overall accuracy in identifying moderate-to-severe OSAS (>80%) and the high negative predictive value obtained were extremely useful in ruling out disease [34].
Furthermore, other type 4 devices have been evaluated for screening or identifying OSAS in different populations, with mixed results [94, 95, 105, 113].
OSAS process management and therapeutic decisions
Various studies with type 4 monitors have used comprehensive algorithms, incorporating portable monitoring to both diagnose and initiate treatment in their OSAS patients [97, 114]. Berry et al. [97] compared a type 4 device with PSG and they found no statistical difference in clinical outcomes (Epworth Sleepiness Scale, Functional Outcomes of Sleep Questionnaire or CPAP adherence) between the two groups, but considerable time was spent training the patients how to use the portable monitoring device. Furthermore, a randomised study between home oximetry and PSG [114] demonstrated that there were no significant differences in predictions of the outcomes or benefits of CPAP made by home oximetry or PSG. These studies suggest that it may be possible to start CPAP treatment on the basis of portable monitoring type 4 devices, but more studies are needed.
Several studies have compared single-channel nasal pressure via nasal cannulae (SNP) and automatic scoring with in-laboratory PSG [88, 104–111]. The authors suggested performing SNP in all patients with OSAS suspicion and recommending CPAP for severe cases (i.e. SNP RDI ≥30 events·h−1). However, the drawbacks are the underestimation of SNP RDI compared with PSG, particularly for intermediate-to-high RDI values, and the difficulty in obtaining a single cut-off point for SNP RDI that either identifies or rules out OSAS. Large studies are needed to determine whether a SNP with automatic scoring could recommend CPAP treatment in agreement with therapeutic decisions based on in-laboratory PSG.
In recent decades, portable monitoring devices, particularly type 3 monitors, have improved quite considerably, but they are still quite complicated to assemble and score. These factors could contribute to the underdiagnosis and undertreatment of OSAS, especially on a primary care level. Many type 4 portable monitoring devices are currently available, but one in particular, based on single-channel nasal pressure as surrogate airflow, has been developed with encouraging results. It is probable that these devices could be useful at different health levels and even primary care physicians could manage them. Perhaps SNP could be recommended at the primary care level for a more symptomatic group of patients or for a high SNP RDI cut-off, as in the case of a therapeutic decision based on RP [75].
Costs
The availability of cheaper, more user-friendly devices for the management of patients with OSAS, such as type 4 monitors, could develop different approaches applicable by healthcare professionals who are not sleep specialists, such as family doctors.
OSAS is more common than asthma, COPD or diabetes and it needs to be managed at different health levels, given that OSAS is already a great burden to public health.
Cost analyses are complicated by the variability of the type 4 devices, and inferences about cost savings are based on favourable sensitivity and specificity conclusions for portable monitoring devices. Therefore, these results should be treated with caution.
One of the few cost-effectiveness analyses to be performed compared nocturnal oximetry with PSG to determine their usefulness in OSAS [115]. This analysis showed that there were cost savings in oximetry, but the considerable loss of diagnostic accuracy did not ultimately provide a cost-effective approach.
Another study was performed in 150 patients attending a sleep laboratory [116]. All the patients used a portable monitoring device, which was followed by a PSG in two situations: doubtful results (25%) and results that indicated that repeat testing was required (10%). The authors concluded that it could reduce the need for diagnostic PSG in almost 75% of patients, thereby reducing the costs associated with diagnostic approaches.
One recent publication was performed using an apnoea-link device: it compared the primary care management of patients with OSAS (using auto-CPAP) with specialist sleep-centre management with PSG [25]. This interesting study featured treatment from a primary care physician that was managed by a trained nurse. The authors observed that primary care management was ∼40% cheaper than solely specialist care after 6 months of follow-up, with no clinical differences between the two groups. However, more patients withdrew from the study in the primary care group (21% versus 8%).
Given that apnoea-link studies with a single channel of nasal airflow pressure have produced promising results, well-designed cost-effectiveness studies should be performed in the future.
Conclusions
Although in-laboratory PSG is the standard test used to diagnose OSA, the evidence shows that, in adult patients with a high pre-test probability of moderate-to-severe OSAS, unattended portable monitoring devices (type 2 and 3) can be used at home for diagnosis, particularly when access to laboratory sleep studies and sleep specialists is limited [71–74, 97, 98, 117]. This approach could reduce the underdiagnosis and undertreatment of OSAS patients.
Moreover, we should not forget that PSG becomes important in patients who have symptoms and certain comorbidities, such as COPD or stroke, but no significant indication of OSAS on portable monitoring, as well as in patients with a history suggesting a different sleep disorder.
Results obtained from portable monitoring devices may be less accurate compared with those from attended devices, but overall they are less expensive and can be used in the patient's home. There is no ideal portable monitoring device, but the device needs to provide a sufficiently accurate diagnosis and be adaptable for auto-application in the home by inexperienced patients.
Several strategies have considered a primary care model [25] and a trained nurse model using home autoCPAP [74] to diagnose and treat patients with OSAS, with promising results. Moreover, there are many studies that show no difference in short-term compliance and response to CPAP therapy when portable monitoring and CPAP autotitration at home are compared with in-laboratory PSG.
With regard to evidence gathered in type 4 sleep studies, the results are less conclusive. There remains some residual doubt about the generalised use of these devices for diagnosis. Nevertheless, studies performed on SNP versus in-laboratory PSG [88, 104–111] have achieved acceptable outcomes, but more studies are still necessary.
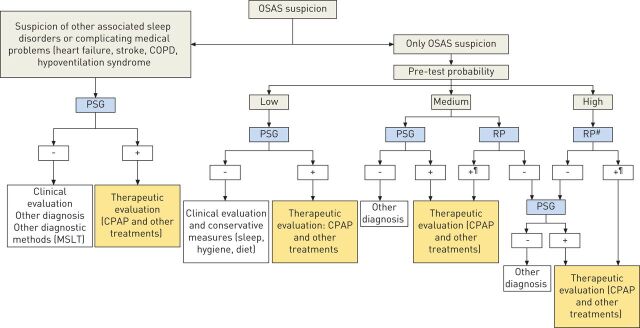
It is probable the management of OSAS patients could be improved by using the type 1–4 sleep studies available in a sleep reference centre, working in coordination with primary care and sleep nonreference centres that only have type 3 or 4 monitoring devices available. This approach could also be enhanced by telematic procedures [52]. One possible diagnostic and management strategy in cases of suspicion of OSAS is summarised in figure 1].
Figure 1.
Diagnostic and management strategy recommended in obstructive sleep apnoea syndrome (OSAS) suspicion [52, 75–77]. Low probability: snoring + apnoea + no sleepiness, no cardiovascular comorbidity. Medium probability: snoring + apnoea and/or Epworth Sleepiness Scale (ESS) 12–15 and/or body mass index (BMI) >30 kg·m−2, no cardiovascular comorbidity. High probability: snoring + apnoea + ESS >15 and/or BMI >30 kg·m−2 and/or cardiovascular comorbidity. #: consider also single nasal pressure and oximetry (type 4 sleep study) and auto-continuous positive airway pressure (CPAP); ¶: no agreement in respiratory polygraphy (RP) apnoea/hypopnoea index (AHI) cut-off point to establish OSAS diagnosis by RP, but could consider OSAS with RP AHI cut-off point ≥10 events·h−1 [52]. COPD: chronic obstructive pulmonary disease; PSG: polysomnography; MSLT: Multiple Sleep Latency Test.
We should really regard ambulatory monitoring as a complementary rather than an exclusive method of in-laboratory PSG in OSAS patients.
It is time to look to the future and, as stated by the official Americal Thoracic Society/AASM/American College of Chest Physicians/European Respiratory Society Workshop report, there are priorities in ambulatory management of adults with OSAS [118]. We should work together to establish adequate research networks for sleep disorders and develop disease management models based on prospective clinical and economic outcome studies because, despite the possible appeal of portable monitoring devices, more cost-effectiveness studies with measures of quality-associated life-years should be performed. There is also a need for studies in specific populations, such as children and patients without any high pre-test probability of OSAS and, finally, scoring methods need to be standardised.
Footnotes
Provenance: Submitted article, peer reviewed.
Conflict of interest: None declared.
References
- 1.American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual, 2nd Edn. Westchester, American Academy of Sleep Medicine, 2005. [Google Scholar]
- 2.Epstein LJ, Kristo D, Strollo PJ, Jr, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009; 5: 263–276. [PMC free article] [PubMed] [Google Scholar]
- 3.Grupo Español de Sueño (GES). Consenso Nacional sobre el síndrome de apneas-hipoapneas del sueño. [National consensus on the syndrome of sleep apneas and hypopneas.]. Arch Bronconeumol 2005; 41: Suppl. 4, 3–110.17125700 [Google Scholar]
- 4.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 1999; 22: 667–689. [PubMed] [Google Scholar]
- 5.Marin JM, Carrizo SJ, Vicente E, et al. Long term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 2005; 365: 1046–1053. [DOI] [PubMed] [Google Scholar]
- 6.Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara JA. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med 1999; 340: 847–851. [DOI] [PubMed] [Google Scholar]
- 7.Masa JF, Rubio M, Findley LJ. Habitually sleepy drivers have a high frequency of automobile crashes associated with respiratory disorders during sleep. Am J Respir Crit Care Med 2000; 162: 1407–1412. [DOI] [PubMed] [Google Scholar]
- 8.Peppard PE, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 2000; 342: 1378–1384. [DOI] [PubMed] [Google Scholar]
- 9.Lévy P, Pépin JL, Arnaud C, et al. Obstructive sleep apnea and atherosclerosis. Prog Cardiovasc Dis 2009; 51: 400–410. [DOI] [PubMed] [Google Scholar]
- 10.Parra O, Arboix A, Bechich S, et al. Time course of sleep-related breathing disorders in first-ever stroke or transient ischemic attack. Am J Respir Crit Care Med 2000; 161: 375–380. [DOI] [PubMed] [Google Scholar]
- 11.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality; eighteen-year follow-up of Wisconsin Sleep Cohort. Sleep 2008; 31: 1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 12.American Academy of Pediatrics. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2002; 109: 704–712. [DOI] [PubMed] [Google Scholar]
- 13.Marcus CL, Moore RH, Rosen CL, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med 2013; 368: 2366–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993; 328: 1230–1235. [DOI] [PubMed] [Google Scholar]
- 15.Durán J, Esnaola S, Rubio R, et al. Obstructive sleep apnea–hypopnea and related clinical features in a population-based simple of subjects aged 30 to 70 yr. Am J Respir Crit Care Med 2001; 163: 685–689. [DOI] [PubMed] [Google Scholar]
- 16.Young T, Evans L, Finn L, et al. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997; 20: 705–706. [DOI] [PubMed] [Google Scholar]
- 17.Flemons WW, Douglas NJ, Kuna ST, et al. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med 2004; 169: 668–672. [DOI] [PubMed] [Google Scholar]
- 18.Pack AI. Sleep disordered breathing: access is the issue. Am J Respir Crit Care Med 2004; 169: 666–667. [DOI] [PubMed] [Google Scholar]
- 19.Douglas NJ, Thomas S, Jan MA. Clinical value of polysomnography. Lancet 1992; 339: 347–350. [DOI] [PubMed] [Google Scholar]
- 20.Ballester E, Solans M, Vila X, et al. Evaluation of a portable respiratory recording device for detecting apnoeas and hypopnoeas in subjects from a general population. Eur Respir J 2000; 16: 123–127. [DOI] [PubMed] [Google Scholar]
- 21.Calleja JM, Esnaola S, Rubio R, et al. Comparison of a cardiorespiratory device versus polysomnography for diagnosis of sleep apnoea. Eur Respir J 2002; 20: 1505–1510. [DOI] [PubMed] [Google Scholar]
- 22.Trikalinos TA, Ip S, Raman G, et al. Home diagnosis of obstructive sleep apnea–hypopnea syndrome. Department of Health & Human Services. Agency for Healthcare Research and Quality, 2007. www.cms.gov/Medicare/Coverage/DeterminationProcess/downloads/id48TA.pdf. [PubMed] [Google Scholar]
- 23.Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 2007; 3: 737–747. [PMC free article] [PubMed] [Google Scholar]
- 24.Andreu AL, Chiner E, Sancho-Chust JN, et al. Effect of an ambulatory diagnostic and treatment programme in patients with sleep apnoea. Eur Respir J 2012; 39: 305–312. [DOI] [PubMed] [Google Scholar]
- 25.Chai-Coetzer CL, Antic NA, Rowland LS, et al. Primary care vs specialist sleep center management of obstructive sleep apnea and daytime sleepiness and quality of life: a randomized trial. JAMA 2013; 309: 997–1004. [DOI] [PubMed] [Google Scholar]
- 26.Flemons WW, Whitelaw WA, Brant R, et al. Likelihood ratios for a sleep apnea clinical prediction rule. Am J Respir Crit Care 1994; 150: 1279–1285. [DOI] [PubMed] [Google Scholar]
- 27.Maislin G, Pack AI, Kribbs NB, et al. A survey screen for prediction of apnea. Sleep 1995; 18: 158–166. [DOI] [PubMed] [Google Scholar]
- 28.Rowley JA, Aboussouan LS, Badr MS. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep 2000; 23: 929–938. [DOI] [PubMed] [Google Scholar]
- 29.Kushida CA, Efron B, Guilleminault C. A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Intern Med 1997; 127: 581–587. [DOI] [PubMed] [Google Scholar]
- 30.Tsai WH, Remmers JE, Brant R, et al. A decision rule for diagnostic testing in obstructive sleep apnea. Am J Respir Crit Care Med 2003; 167: 1427–1432. [DOI] [PubMed] [Google Scholar]
- 31.Lee RW, Chan AS, Grunstein RR, et al. Craniofacial phenotyping in obstructive sleep apnea – a novel quantitative photographic approach. Sleep 2009; 32: 37–45. [PMC free article] [PubMed] [Google Scholar]
- 32.Netzer NC, Stoohs RA, Netzer CM, et al. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999; 131: 485–491. [DOI] [PubMed] [Google Scholar]
- 33.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008; 108: 812–821. [DOI] [PubMed] [Google Scholar]
- 34.Chai-Coetzer CL, Antic NA, Rowland LS, et al. A simplified model of screening questionnaire and home monitoring for obstructive sleep apnoea in primary care. Thorax 2011; 66: 213–219. [DOI] [PubMed] [Google Scholar]
- 35.Ferber R, Millman R, Coppola M, et al. Portable recording in the assessment of obstructive sleep apnea. Sleep 1994; 17: 378–392. [DOI] [PubMed] [Google Scholar]
- 36.Flemons WW, Littner MR, Rowley JA, et al. Home diagnosis of sleep apnea: a systematic review of the literature. An evidence review cosponsored by the American Academy of Sleep Medicine, the American College of Chest Physicians, and the American Thoracic Society. Chest 2003; 124: 1543–1579. [DOI] [PubMed] [Google Scholar]
- 37.Pelletier-Fleury N, Meslier N, Gagnadoux F, et al. Economic arguments for the immediate management of moderate-to-severe obstructive sleep apnoea syndrome. Eur Respir J 2004; 23: 53–60. [DOI] [PubMed] [Google Scholar]
- 38.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 2012; 8: 597–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Masa JF, Corral J, Pereira R, et al. Effectiveness of sequential automatic-manual home respiratory polygraphy scoring. Eur Respir J 2013; 41: 879–887. [DOI] [PubMed] [Google Scholar]
- 40.Chesson AL, Jr, Berry RB, Pack A, et al. Practice parameters for the use of portable monitoring devices in the investigation of suspected obstructive sleep apnea in adults. Sleep 2003; 26: 907–913. [DOI] [PubMed] [Google Scholar]
- 41.Collop NA. Portable monitoring for the diagnosis of obstructive sleep apnea. Curr Opin Pulm Med 2008; 14: 525–529. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Medicare and Medicaid Services. Decision Memo for Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (CAG-00093R2). March 13, 2008.
- 43.Centers for Medicare and Medicaid Services, Decision Memo for Sleep Testing for obstructive sleep apnea (OSA) (CAG-00405N). March 3, 2009. [PubMed]
- 44.Collop NA, Tracy SL, Kapur V, et al. Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med 2011; 7: 531–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Redline S, Sanders MH, Lind BK, et al. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group. Sleep 1998; 21: 759–767. [PubMed] [Google Scholar]
- 46.Iber C, Redline S, Kaplan Gilpin AM, et al. Polysomnography performed in the unattended home versus the attended laboratory setting – Sleep Heart Health Study methodology. Sleep 2004; 27: 536–540. [DOI] [PubMed] [Google Scholar]
- 47.Portier F, Portmann A, Czernichow P, et al. Evaluation of home versus laboratory polysomnography in the diagnosis of sleep apnea syndrome. Am J Respir Crit Care Med 2000; 162: 814–818. [DOI] [PubMed] [Google Scholar]
- 48.Campbell AJ, Neill AM. Home set-up polysomnography in the assessment of suspected obstructive sleep apnea. J Sleep Res 2011; 20: 207–213. [DOI] [PubMed] [Google Scholar]
- 49.Fry JM, DiPhillipo MA, Curran K, et al. Full polysomnography in the home. Sleep 1998; 21: 635–642. [DOI] [PubMed] [Google Scholar]
- 50.García-Díaz E, Quintana-Gallego E, Ruiz A, et al. Respiratory polygraphy with actigraphy in the diagnosis of sleep apnea–hypopnea syndrome. Chest 2007; 131: 725–732. [DOI] [PubMed] [Google Scholar]
- 51.Santos-Silva R, Sartori DE, Truksinas V, et al. Validation of a portable monitoring system for the diagnosis of obstructive sleep apnea syndrome. Sleep 2009; 32: 629–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Masa JF, Corral J, Pereira R, et al. Effectiveness of home respiratory polygraphy for the diagnosis of sleep apnoea and hypopnoea syndrome. Thorax 2011; 66: 567–573. [DOI] [PubMed] [Google Scholar]
- 53.Alonso Alvarez M de L, Terán Santos J, Cordero Guevara J, et al. Fiabilidad de la poligrafia respiratoria domiciliaria para el diagnostico del sindrome de apneas-hipopneas durante el sueno. Analisis de costs. [Reliability of home respiratory polygraphy for the diagnosis of sleep apnea–hypopnea syndrome: analysis of costs]. Arch Bronconeumol 2008; 44: 22–28. [PubMed] [Google Scholar]
- 54.Masa JF, Corral J, Gómez de Terreros J, et al. Significance of including a surrogate arousal for sleep apnea–hypopnea syndrome diagnosis by respiratory polygraphy. Sleep 2013; 36: 249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ancoli-Israel S, Kripke DF, Mason W, et al. Comparisons of home sleep recordings and polysomnograms in older adults with sleep disorders. Sleep 1981; 4: 283–291. [DOI] [PubMed] [Google Scholar]
- 56.Redline S, Tosteson T, Boucher MA, et al. Measurement of sleep-related breathing disturbance in epidemiological studies. Assessment of the validity and reproducibility of a portable monitoring device. Chest 1991; 100: 1281–1286. [DOI] [PubMed] [Google Scholar]
- 57.Man GCW, Kang BV. Validation of a portable sleep apnea monitoring device. Chest 1995; 108: 388–393. [DOI] [PubMed] [Google Scholar]
- 58.Parra O, García-Esclesans N, Montserrat JM, et al. Should patients with sleep apnoea/hypopnoea syndrome be diagnosed and managed on the basis of home sleep studies? Eur Respir J 1997; 10: 1720–1724. [DOI] [PubMed] [Google Scholar]
- 59.Dingli K, Coleman EL, Vennelle M, et al. Evaluation of a portable device for diagnosing the sleep apnoea/hypopnoea syndrome. Eur Respir J 2003; 21: 253–259. [DOI] [PubMed] [Google Scholar]
- 60.Reichert JA, Bloch DA, Cundiff E, et al. Comparison of the NovaSom QSG, a new sleep apnea home-diagnostic system, and polysomnography. Sleep Med 2003; 4: 213–218. [DOI] [PubMed] [Google Scholar]
- 61.Su S, Baroody FM, Kohrman M, et al. A comparison of polysomnography and a portable home sleep study in the diagnosis of obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg 2004; 131: 844–850. [DOI] [PubMed] [Google Scholar]
- 62.Candela A, Hernández L, Asensio S, et al. Validación de un equipo de poligrafía respiratoria en el diagnóstico del síndrome de apneas durante el sueño. [Validation of a respiratory polygraphy system in the diagnosis of sleep apnea syndrome]. Arch Bronconeumol 2005; 41: 71–77. [DOI] [PubMed] [Google Scholar]
- 63.Yin M, Miyazaki S, Ishikawa K. Evaluation of type 3 portable monitoring in unattended home setting for suspected sleep apnea: factors that may affect its accuracy. Otolaryngol Head Neck Surg 2006; 134: 204–209. [DOI] [PubMed] [Google Scholar]
- 64.Tonelli de Oliveira AC, Martinez D, Vasconcelos LF, et al. Diagnosis of obstructive sleep apnea syndrome and its outcomes with home portable monitoring. Chest 2009; 135: 330–336. [DOI] [PubMed] [Google Scholar]
- 65.Hernández L, Torrella M, Roger N, et al. Management of sleep apnea: concordance between nonreference and reference centers. Chest 2007; 132: 1853–1857. [DOI] [PubMed] [Google Scholar]
- 66.Gjevre JA, Taylor-Gjevre RM, Skomro R, et al. Comparison of polysomnographic and portable home monitoring assessments of obstructive sleep apnea in Saskatchewan women. Can Respir J 2011; 18: 271–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Polese JF, Santos-Silva R, de Oliveira Ferrari PM, et al. Is portable monitoring for diagnosing obstructive sleep apnea syndrome suitable in elderly population? Sleep Breath 2013; 17: 679–686. [DOI] [PubMed] [Google Scholar]
- 68.Quintana-Gallego E, Villa-Gil M, Carmona-Bernal C, et al. Home respiratory polygraphy for diagnosis of sleep-disordered breathing in heart failure. Eur Respir J 2004; 24: 443–448. [DOI] [PubMed] [Google Scholar]
- 69.Sériès F, Kimoff RJ, Morrison D, et al. Prospective evaluation of nocturnal oximetry for detection of sleep-related breathing disturbances in patients with chronic heart failure. Chest 2005; 127: 1507–1514. [DOI] [PubMed] [Google Scholar]
- 70.Oliveira MG, Nery LE, Santos-Silva R, et al. Is portable monitoring accurate in the diagnosis of obstructive sleep apnea syndrome in chronic pulmonary obstructive disease? Sleep Med 2012; 13: 1033–1038. [DOI] [PubMed] [Google Scholar]
- 71.Mulgrew AT, Fox N, Ayas NT, et al. Diagnosis and initial management of obstructive sleep apnea without polysomnography: a randomized validation study. Ann Intern Med 2007; 146: 157–166. [DOI] [PubMed] [Google Scholar]
- 72.Rosen CL, Auckley D, Benca R, et al. A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory-based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep 2012; 35: 757–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Skomro RP, Gjevre J, Reid J, et al. Outcomes of home-based diagnosis and treatment of obstructive sleep apnea. Chest 2010; 138: 257–263. [DOI] [PubMed] [Google Scholar]
- 74.Antic NA, Buchan C, Esterman A, et al. A randomized controlled trial of nurse-led care for symptomatic moderate-severe obstructive sleep apnea. Am J Respir Crit Care Med 2009; 179: 501–508. [DOI] [PubMed] [Google Scholar]
- 75.Masa JF, Corral J, Pereira R, et al. Therapeutic decision-making for sleep apnea and hypopnea syndrome using home respiratory polygraphy. A large multicentric study. Am J Respir Crit Care Med 2011; 184: 964–971. [DOI] [PubMed] [Google Scholar]
- 76.Ayas NT, Patel SR, Malhotra A, et al. Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep 2004; 27: 249–253. [DOI] [PubMed] [Google Scholar]
- 77.Masa JF, Jiménez A, Durán J, et al. Alternative methods of titrating continuous positive airway pressure: a large multicenter study. Am J Respir Crit Care Med 2004; 170: 1218–1224. [DOI] [PubMed] [Google Scholar]
- 78.West SD, Jones DR, Stradling JR. Comparison of three ways to determine and deliver pressure during nasal CPAP therapy for obstructive sleep apnoea. Thorax 2006; 61: 226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Morgenthaler TI, Aurora RN, Brown T, et al. Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine report. Sleep 2008; 31: 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Whittle AT, Finch SP, Mortimore IL, et al. Use of home sleep studies for diagnosis of the sleep apnoea/hypopnoea syndrome. Thorax 1997; 52: 1068–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Deutsch PA, Simmons MS, Wallace JM. Cost-effectiveness of split-night polysomnography and home studies in the evaluation of obstructive sleep apnea syndrome. J Clin Sleep Med 2006; 2: 145–153. [PubMed] [Google Scholar]
- 82.Chervin RD, Murman DL, Malow BA, et al. Cost-utility of three approaches to the diagnosis of sleep apnea: polysomnography, home testing, and empirical therapy. Ann Intern Med 1999; 130: 496–505. [DOI] [PubMed] [Google Scholar]
- 83.Reuveni H, Schweitzer E, Tarasiuk A. A cost-effectiveness analysis of alternative at-home or in-laboratory technologies for the diagnosis of obstructive sleep apnea syndrome. Med Decis Making 2001; 21: 451–458. [DOI] [PubMed] [Google Scholar]
- 84.Pietzsch JB, Garner A, Cipriano LE, et al. An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep apnea. Sleep 2011; 34: 695–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McArdle N, Singh B, Murphy M, et al. Continuous positive airway pressure titration for obstructive sleep apnoea: automatic versus manual titration. Thorax 2010; 65: 606–611. [DOI] [PubMed] [Google Scholar]
- 86.Grover SS, Pittman SD. Automated detection of sleep disordered breathing using a nasal pressure monitoring device. Sleep Breath 2008; 12: 339–345. [DOI] [PubMed] [Google Scholar]
- 87.Rees K, Wraith PK, Berthon-Jones M, et al. Detection of apnoeas, hypopnoeas and arousals by the AutoSet in the sleep apnoea/hypopnoea syndrome. Eur Respir J 1998; 12: 764–769. [DOI] [PubMed] [Google Scholar]
- 88.Erman MK, Stewart D, Einhorn D, et al. Validation of the ApneaLink for the screening of sleep apnea: a novel and simple single-channel recording device. J Clin Sleep Med 2007; 3: 387–392. [PMC free article] [PubMed] [Google Scholar]
- 89.Bar A, Pillar G, Dvir I, et al. Evaluation of a portable device based on peripheral arterial tone for unattended home sleep studies. Chest 2003; 123: 695–703. [DOI] [PubMed] [Google Scholar]
- 90.Nakano H, Hayashi M, Ohshima E, et al. Validation of a new system of tracheal sound analysis for the diagnosis of sleep apnoea–hypopnoea syndrome. Sleep 2004; 27: 951–957. [DOI] [PubMed] [Google Scholar]
- 91.Mueller A, Fietze I, Voelker R, et al. Screening for sleep-related breathing disorders by transthoracic impedance recording integrated into a Holter ECG system. J Sleep Res 2006; 15: 455–462. [DOI] [PubMed] [Google Scholar]
- 92.Westbrook PR, Levendowski DJ, Cvetinovic M, et al. Description and validation of the apnoea risk evaluation system: a novel method to diagnose sleep apnoea–hypopnoea in the home. Chest 2005; 128: 2166–2175. [DOI] [PubMed] [Google Scholar]
- 93.Vázquez JC, Tsai WH, Flemons WW, et al. Automated analysis of digital oximetry in the diagnosis of obstructive sleep apnoea. Thorax 2000; 55: 302–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ayappa I, Norman RG, Seelall V, et al. Validation of a self-applied unattended monitor for sleep disordered breathing. J Clin Sleep Med 2008; 4: 26–37. [PMC free article] [PubMed] [Google Scholar]
- 95.Pittman SD, Ayas NT, MacDonald MM, et al. Using a wrist-worn device based on peripheral arterial tonometry to diagnose obstructive sleep apnea: in-laboratory and ambulatory validation. Sleep 2004; 27: 923–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Heneghan C, Chua CP, Garvey JF, et al. A portable automated assessment tool for sleep apnoea using a combined Holter-oximeter. Sleep 2008; 31: 1432–1439. [PMC free article] [PubMed] [Google Scholar]
- 97.Berry RB, Hill G, Thompson L, et al. Portable monitoring and autotitration versus polysomnography for the diagnosis and treatment of sleep apnea. Sleep 2008; 31: 1423–1431. [PMC free article] [PubMed] [Google Scholar]
- 98.Pitson DJ, Stradling JR. Autonomic markers of arousal during sleep in patients undergoing investigation for obstructive sleep apnoea, their relationship to EEG arousals, respiratory events and subjective sleepiness. J Sleep Res 1998; 7: 53–59. [DOI] [PubMed] [Google Scholar]
- 99.Pillar G, Bar A, Shlitner A, et al. Autonomic aorusal index: an automated detection based on peripheral arterial tonometry. Sleep 2002; 25: 543–549. [PubMed] [Google Scholar]
- 100.Ayappa I, Norman RG, Krieger AC, et al. Non-invasive detection of respiratory effort-related arousals (REras) by a nasal cannula/pressure transducer system. Sleep 2000; 23: 763–771. [DOI] [PubMed] [Google Scholar]
- 101.Pillar G, Bar A, Betito M, et al. An automatic ambulatory device for detection of AASM defined arousals from sleep: the WP100. Sleep Med 2003; 4: 207–212. [DOI] [PubMed] [Google Scholar]
- 102.Wiltshire N, Kendrick AH, Catterall JR. Home oximetry studies for diagnosis of sleep apnea/hypopnea syndrome: limitation of memory storage capabilities. Chest 2001; 120: 384–389. [DOI] [PubMed] [Google Scholar]
- 103.Ng SS, Chan TO, To KW, et al. Validation of a portable recording device (ApneaLink) for identifying patients with suspected obstructive sleep apnea syndrome (OSAS). Intern Med J 2009; 39: 757–762. [DOI] [PubMed] [Google Scholar]
- 104.Wong KKH, Jankelson D, Reid A, et al. Diagnostic test evaluation of a nasal flow monitor for obstructive sleep apnea detection in sleep apnea research. Behav Res Methods 2008; 40: 360–366. [DOI] [PubMed] [Google Scholar]
- 105.Watkins MR, Talmage JB, Thiese MS, et al. Correlation between screening for obstructive sleep apnea using a portable device versus polysomnography testing in a commercial driving population. J Occup Environ Med 2009; 51: 1145–1150. [DOI] [PubMed] [Google Scholar]
- 106.Rofail LM, Wong KKH, Unger G, et al. The utility of single-channel nasal airflow pressure transducer in the diagnosis of OSA at home. Sleep 2010; 33: 1097–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rofail LM, Wong KKH, Unger G, et al. Comparison between a single-channel nasal airflow device and oximetry for the diagnosis of obstructive sleep apnea. Sleep 2010; 33: 1106–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ragette R, Wang Y, Weinreich G, et al. Diagnostic performance of single airflow channel recording (Apnea Link) in home diagnosis of sleep apnea. Sleep Breath 2010; 14: 109–114. [DOI] [PubMed] [Google Scholar]
- 109.Clark AL, Crabbe S, Aziz A, et al. Use of a screening tool for detection of sleep-disordered breathing. J Laryngol Otol 2009; 123: 746–749. [DOI] [PubMed] [Google Scholar]
- 110.Oktay B, Rice TB, Atwood CW Jr, et al. Evaluation of a single-channel portable monitor for the diagnosis of obstructive sleep apnea. J Clin Sleep Med 2011; 7: 384–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ayappa I, Norman RG, Suryadevara M, et al. Comparison of limited monitoring using a nasal-cannula flow signal to full polysomnography in sleep-disordered breathing. Sleep 2004; 27: 1171–1179. [DOI] [PubMed] [Google Scholar]
- 112.Gantner D, Ge JY, Li LH, et al. Diagnostic accuracy of a questionnaire and simple home monitoring device in detecting obstructive sleep apnoea in a Chinese population at high cardiovascular risk. Respirology 2010; 15: 952–960. [DOI] [PubMed] [Google Scholar]
- 113.Lesser DJ, Haddad GG, Bush RA, et al. The utility of a portable recording device for screening of obstructive sleep apnea in obese adolescents. J Clin Sleep Med 2012; 8: 271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Whitelaw WA, Brant RF, Flemons WW. Clinical usefulness of home oximetry compared with polysomnography for assessment of sleep apnea. Am J Respir Crit Care Med 2005; 171: 188–193. [DOI] [PubMed] [Google Scholar]
- 115.Epstein LJ, Dorlac GR. Cost-effectiveness analysis of nocturnal oximetry as a method of screening for sleep apnea–hypopnea syndrome. Chest 1998; 113: 97–103. [DOI] [PubMed] [Google Scholar]
- 116.Esnaola D, Durán J, Infante-Rivard C, et al. Diagnostic accuracy of a portable recording device (MESAM IV) in suspected obstructive sleep apnoea. Eur Respir J 1996; 9: 2597–2605. [DOI] [PubMed] [Google Scholar]
- 117.Kuna ST, Gurubhagavatula I, Maislin G, et al. Noninferiority of functional outcome in ambulatory management of obstructive sleep apnea. Am J Respir Crit Care Med 2011; 183: 1238–1244. [DOI] [PubMed] [Google Scholar]
- 118.Kuna ST, Badr MS, Kimoff RJ, et al. An official ATS/AASM/ACCP/ERS Workshop report: research priorities in ambulatory management of adults with obstructive sleep apnea. Proc Am Thorac Soc 2011; 8: 1–16. [DOI] [PubMed] [Google Scholar]