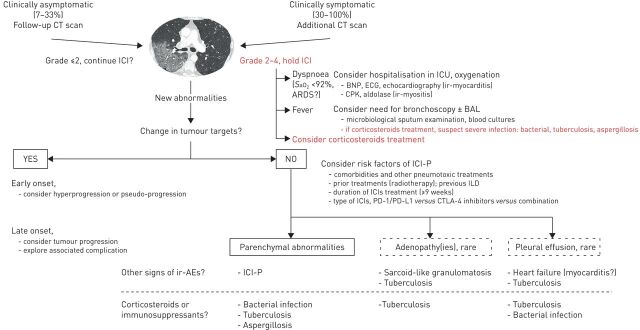
FIGURE 4.
Proposed algorithm for the management of suspected immune checkpoint inhibitor-related pneumonitis (ICI-P). Schematically, two settings may present in a patient treated with ICI for a nonsmall cell lung carcinoma: either new images occur on the cancer follow-up computed tomography (CT) scan or the CT scan is performed because of new respiratory (cough and dyspnoea) or general symptoms (fevers and extrathoracic signs). In each case, CT scan analysis should focus on cancer progression (probable progression) or the occurrence of new parenchymal abnormalities; particularly ground-glass opacities or condensation(s) (possible ICI-P or infection), pleurisy or mediastinal lymphadenopathy being more rarely observed. In case of respiratory or general symptoms, their severity must be graded and a hospitalisation considered in view of the appropriate diagnostic tests and symptomatic treatment initiation. In case of a fever, an extensive microbial investigation must be carried out, particularly if the patient is under immunosuppresants. ICI must be stopped and the initiation of high-dose corticosteroid therapy discussed. In the absence of tumour progression, the discussion between ICI-P or infectious pneumonia is likely to depend on concomitant respective risk factors and on the documentation of an infection. ICU: intensive care unit; BNP: bone natriuretic protein; CPK: creatine phosphokinase; BAL: bronchioloalveolar lavage; ir: immune-related; AE: adverse events; ARDS: acute respiratory distress syndrome; ILD: interstitial lung disease: SaO2: arterial oxygen saturation; PD-1: programmed cell death protein; PD-L1: programmed cell death ligand 1; CTLA: cytotoxic T-lymphocyte associated antigen.